Injuries We Treat in Pasadena, TX
Expert Treatment for Car Accident & Personal Injury Victims
At AccidentDoc Pasadena, we specialize in comprehensive medical care for accident-related injuries. Our board-certified physicians and injury specialists provide evidence-based treatment for whiplash, back injuries, soft tissue damage, and more. With over 400+ patients successfully treated, we understand the physical, emotional, and legal complexities of accident recovery. We accept all insurance, including PIP and MedPay, and offer Letter of Protection treatment—meaning $0 out-of-pocket until your case settles. Same-day appointments available for new patients.
Whiplash & Neck Injuries

Whiplash is the most common injury resulting from car accidents, affecting over 3 million Americans annually. This cervical spine injury occurs when sudden deceleration causes the head to rapidly move forward and backward, straining the delicate muscles, ligaments, and vertebrae in the neck. At AccidentDoc Pasadena, our board-certified physicians specialize in comprehensive whiplash treatment, from initial diagnosis through complete recovery.
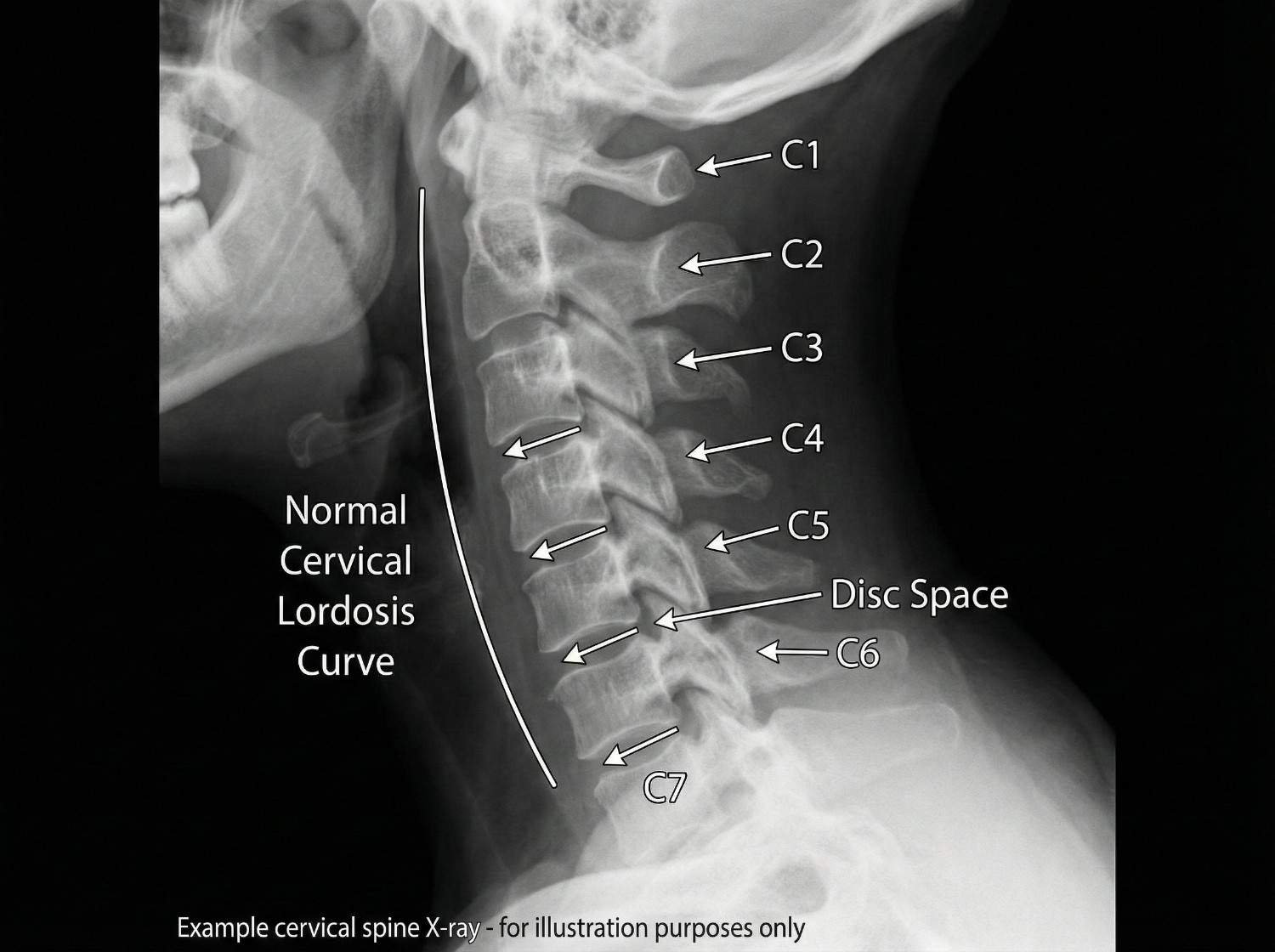
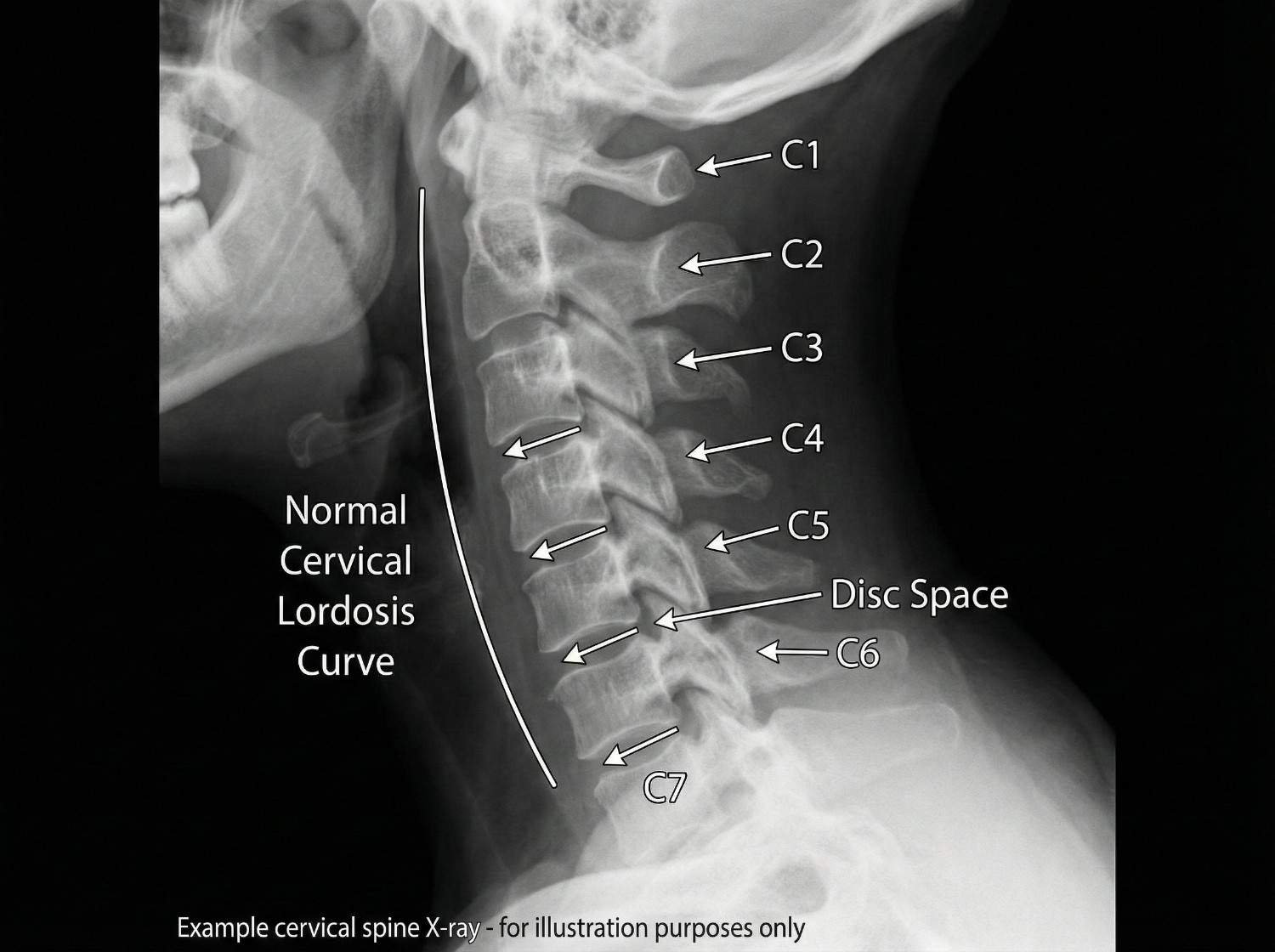
Whiplash is a complex soft tissue injury involving the cervical spine's intricate network of seven vertebrae (C1-C7), intervertebral discs, facet joints, muscles, ligaments, and nerve roots. The injury mechanism typically involves a hyperextension-hyperflexion sequence: during rear-end collisions, the torso is thrust forward by the seatback while the head momentarily remains stationary due to inertia. This creates an S-shaped curve in the cervical spine, straining the anterior longitudinal ligament and anterior neck muscles. Milliseconds later, the head snaps forward into hyperflexion, overstretching the posterior ligaments, facet joint capsules, and paraspinal muscles.
The forces involved can exceed 5G of acceleration, causing microscopic tears in muscle fibers, ligament strains, facet joint capsule injuries, and in severe cases, intervertebral disc damage or nerve root compression. The C5-C6 and C6-C7 spinal segments bear the greatest stress due to their location at the cervical spine's mobile center. Research published in the Journal of Orthopaedic & Sports Physical Therapy demonstrates that even low-speed collisions (5-10 mph) can generate sufficient force to cause whiplash, as the sudden acceleration-deceleration exceeds the neck's protective muscle contraction response time.
What makes whiplash particularly challenging is its biomechanical complexity. Unlike a simple muscle strain, whiplash often involves multiple tissue types simultaneously: muscle-tendon units, ligamentous structures, facet joint capsules, and sometimes disc integrity. The injury cascade doesn't stop at the moment of impact—inflammatory mediators released by damaged tissues can sensitize nerve endings, leading to chronic pain if left untreated. Our team at AccidentDoc Pasadena employs advanced diagnostic protocols to identify all involved structures, ensuring comprehensive treatment rather than symptomatic relief alone.
Rear-end collisions account for approximately 80% of all whiplash injuries, making them the leading cause by a substantial margin. These accidents generate the classic hyperextension-hyperflexion mechanism as the struck vehicle rapidly accelerates forward while the occupant's head lags behind. Even at seemingly minor speeds of 5-15 mph, the force differential between vehicle acceleration and head inertia creates significant cervical strain. Side-impact collisions represent the second most common cause, producing lateral whiplash where the head is thrown sideways, straining the scalene muscles and contralateral facet joints.
Frontal collisions, while often associated with more severe injuries, also cause whiplash through a hyperflexion-hyperextension sequence—the reverse of rear-end impacts. Here, the head initially snaps forward (hyperflexion) before rebounding backward (hyperextension). Pedestrian-vehicle collisions generate particularly severe whiplash as the unrestrained pedestrian experiences full-body acceleration without seatbelt protection, often resulting in rotational head movements that combine flexion, extension, and lateral forces simultaneously.
Less common but significant causes include slip-and-fall accidents where the head snaps backward upon impact, sports injuries involving helmet-to-helmet contact or sudden deceleration (football, hockey, rugby), and workplace accidents such as being struck by falling objects or equipment. Even aggressive amusement park rides with rapid acceleration-deceleration cycles have been documented as whiplash causes. The common denominator across all mechanisms is sudden, forceful neck movement that exceeds the cervical spine's physiological range of motion before protective muscle reflexes can activate.
In Pasadena and the greater Houston area, 18-wheeler accidents on Highway 225 and I-45 produce particularly severe whiplash injuries due to the massive size differential between commercial trucks and passenger vehicles. The forces generated in these collisions often result in Grade 2 or Grade 3 whiplash (moderate to severe) with associated complications like disc herniations or radiculopathy.
- Rear-end collisions (80% of cases) - classic hyperextension-hyperflexion
- Side-impact accidents - lateral whiplash with scalene muscle strain
- Frontal collisions - reverse mechanism with airbag forces
- Pedestrian accidents - rotational forces without restraint
- Slip-and-fall with head snap - hyperextension dominant
- 18-wheeler accidents - high-force impacts with severe tissue damage
Whiplash symptoms follow a characteristic temporal pattern that clinicians use to assess injury severity and predict outcomes. Immediate symptoms (0-6 hours post-injury) include neck stiffness, reduced cervical range of motion particularly in rotation and extension, muscle spasms palpable in the paraspinal muscles, and localized pain at the injury site. These acute symptoms reflect the initial inflammatory response and protective muscle guarding. Many patients report feeling "fine" immediately after the accident, only to develop severe symptoms hours later as inflammatory mediators accumulate and muscle spasms intensify.
Delayed symptoms (24-72 hours post-injury) are hallmark features of whiplash and include cervicogenic headaches originating from the occipital region and radiating forward, upper back pain between the shoulder blades (thoracic paraspinal muscle involvement), shoulder pain from muscle strain and referral patterns, dizziness or vertigo from cervical proprioceptor dysfunction, TMJ pain from jaw clenching during impact, and cognitive difficulties like concentration problems or mental fog. This delayed onset occurs because tissue inflammation peaks 24-48 hours after injury, and microscopic muscle tears don't produce pain until inflammatory swelling develops.
Chronic symptoms (persisting beyond 3 months) develop in approximately 50% of whiplash patients without proper treatment and indicate transition to chronic whiplash-associated disorder (WAD). These include persistent neck pain with activity-related flares, radicular symptoms like arm numbness, tingling, or weakness indicating nerve root compression from disc herniation or foraminal stenosis, chronic headaches often refractory to over-the-counter medications, reduced cervical mobility with measurable range of motion deficits, sleep disturbances from pain-related arousals, and psychological symptoms including anxiety about driving or chronic pain-related depression.
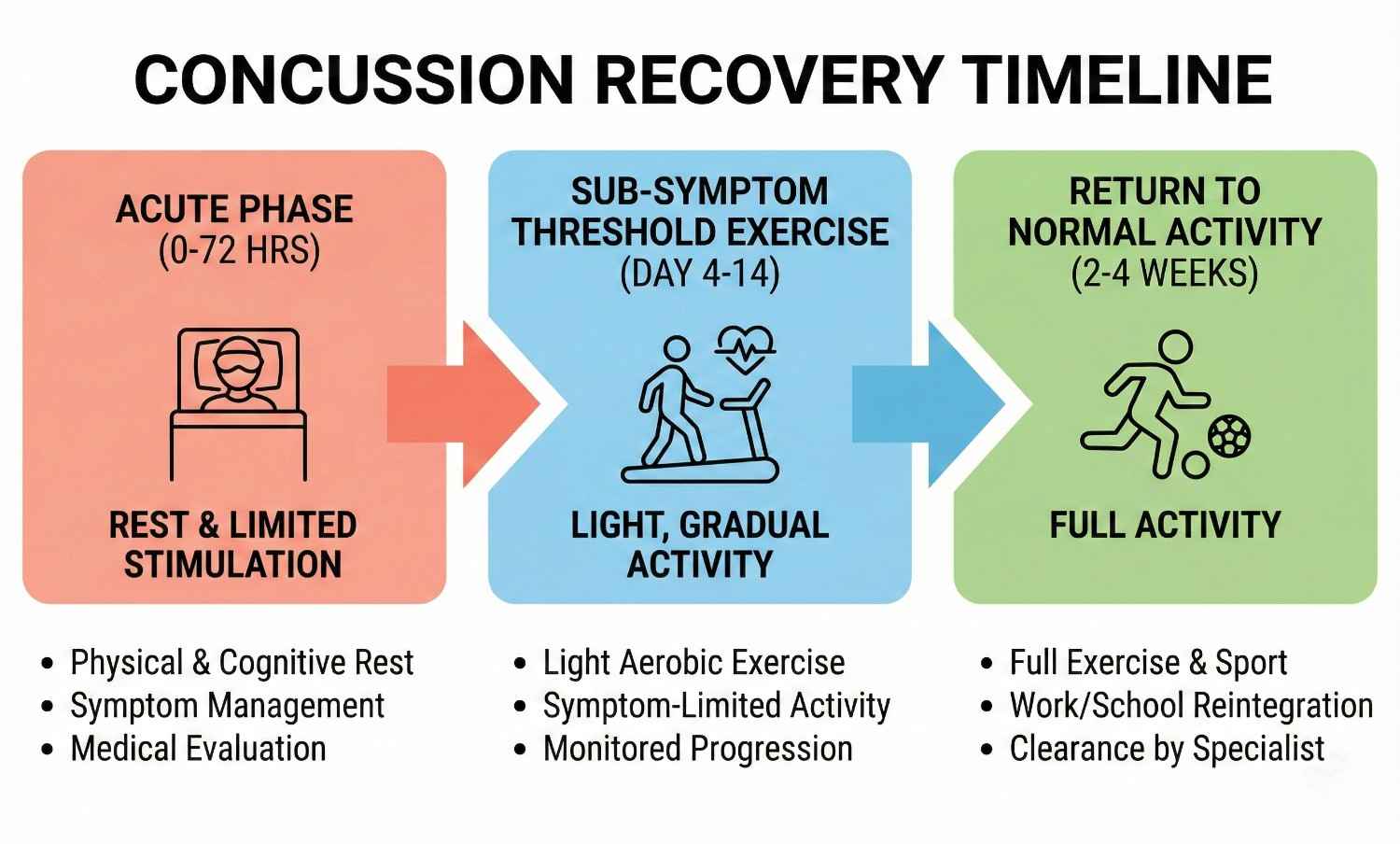
The Quebec Task Force Classification System grades whiplash severity from I (neck pain without objective findings) to IV (neck pain with fracture or dislocation). Grade II injuries (neck pain with musculoskeletal signs) represent the majority of cases we treat at AccidentDoc Pasadena. Early intervention within the first 72 hours significantly improves outcomes, which is why we offer same-day appointments for accident victims.

| Symptom | Timing / Description |
|---|---|
| Neck stiffness and pain | Immediate (0-6 hours) |
| Reduced range of motion | Immediate (0-6 hours) |
| Cervicogenic headaches | Delayed (24-72 hours) |
| Shoulder/upper back pain | Delayed (24-72 hours) |
| Arm numbness/weakness | Delayed or Chronic |
| Dizziness or vertigo | Delayed (24-72 hours) |
| TMJ pain | Delayed (24-72 hours) |
| Cognitive difficulties | Delayed or Chronic |
| Chronic pain with flares | Chronic (>3 months) |
| Sleep disturbances | Chronic (>3 months) |
Accurate whiplash diagnosis requires a systematic approach combining clinical examination with appropriate imaging studies. Our evaluation begins with a detailed medical history documenting accident mechanism, time to symptom onset, symptom progression, and any neurological symptoms. This information guides the physical examination and imaging selection.
Physical examination assesses multiple cervical spine parameters: active and passive range of motion measurement in six planes (flexion, extension, right/left rotation, right/left lateral flexion) using inclinometry or goniometry for objective documentation. We palpate all cervical vertebrae (C1-C7) for point tenderness, assess paraspinal muscle tone and spasm severity, and examine facet joint tenderness with pressure over the lateral masses. Neurological testing includes deep tendon reflexes (biceps C5, brachioradialis C6, triceps C7), sensory examination in all dermatomes, and manual muscle testing for myotomal weakness. Spurling's test (cervical compression with rotation and extension) reproduces radicular symptoms if nerve root compression exists.
Imaging studies are selected based on clinical presentation: Standard cervical X-rays (AP, lateral, open-mouth odontoid) are initial studies to rule out fractures, assess vertebral alignment, measure cervical lordosis, and evaluate disc space heights. While X-rays don't visualize soft tissues, they identify bony abnormalities and instability. MRI (magnetic resonance imaging) is the gold standard for soft tissue evaluation, revealing disc herniations, ligament tears (especially the alar and transverse ligaments at C1-C2), facet joint effusions indicating capsule injury, spinal cord signal changes, and nerve root compression. We order MRI when neurological symptoms exist, severe pain persists beyond 4-6 weeks, or clinical examination suggests disc or ligament injury.
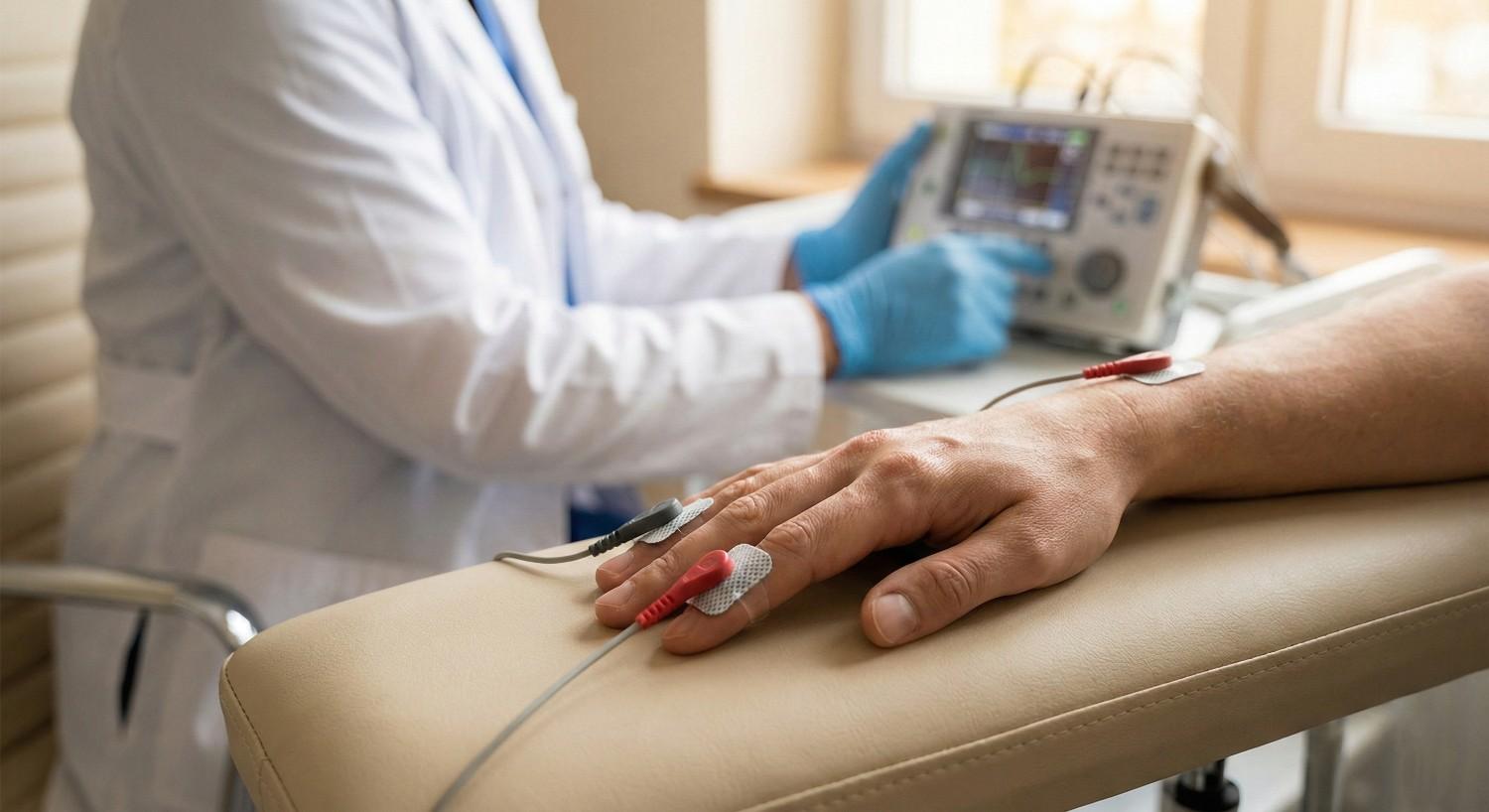
CT scanning provides superior bony detail and is reserved for suspected fractures not visible on X-ray, especially C1-C2 injuries or facet fractures. Electrodiagnostic studies (EMG/NCS - electromyography/nerve conduction studies) performed 3-4 weeks post-injury can confirm radiculopathy when MRI findings are equivocal, differentiating nerve root injury from peripheral nerve entrapment.
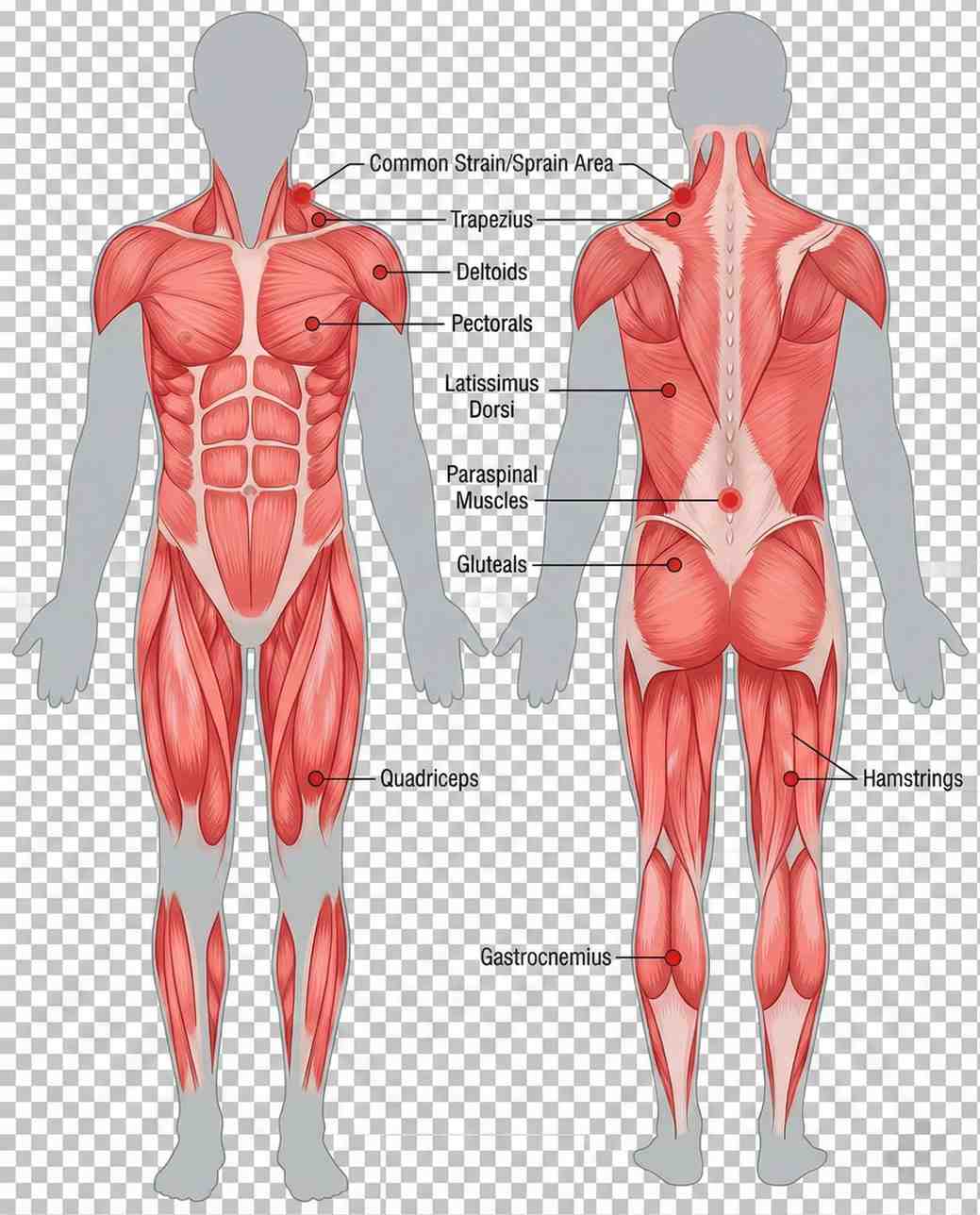
Functional capacity evaluations objectively measure how whiplash affects daily activities, providing documentation for personal injury claims and return-to-work decisions. This comprehensive diagnostic approach ensures we identify all injury components, enabling targeted treatment rather than generic neck pain management.

AccidentDoc Pasadena employs evidence-based treatment protocols progressing through four phases based on injury severity and patient response. All treatment is available through Letter of Protection, meaning $0 out-of-pocket cost until your case settles.
Phase 1 (Acute: Days 1-14) focuses on pain control and inflammation reduction. We prescribe NSAIDs (nonsteroidal anti-inflammatory drugs) like ibuprofen or naproxen to reduce inflammation and pain. Muscle relaxants such as cyclobenzaprine or tizanidine address muscle spasms. Ice application (15-20 minutes every 2-3 hours) reduces inflammation in the first 48-72 hours, then alternating ice/heat improves muscle relaxation. Soft cervical collars are used judiciously for 3-5 days maximum, as prolonged use causes muscle deconditioning. We emphasize active recovery over immobilization, encouraging gentle range of motion within pain tolerance.
Phase 2 (Subacute: Weeks 2-8) introduces active rehabilitation. Physical therapy includes cervical stretching exercises (chin tucks, corner stretches), progressive strengthening of deep neck flexors and stabilizers, postural training to correct forward head posture common in whiplash patients, and manual therapy including soft tissue mobilization. Chiropractic care with gentle cervical adjustments restores normal joint mobility, particularly at C5-C6 and C6-C7 where restriction commonly occurs. We use flexion-distraction techniques and activator methods rather than high-velocity rotational manipulation in acute whiplash. Massage therapy addresses myofascial trigger points in upper trapezius, levator scapulae, and suboccipital muscles that develop secondary to initial injury.
Phase 3 (Intermediate: Weeks 8-16) employs interventional procedures for patients not achieving adequate relief from conservative care. Trigger point injections deliver local anesthetic and sometimes corticosteroid to hyperactive muscle knots, providing immediate pain relief and allowing progression of physical therapy. Facet joint injections target the cervical zygapophyseal joints with fluoroscopically-guided anesthetic and steroid, diagnostic and therapeutic for facet-mediated pain. Medial branch blocks anesthetize the nerves supplying facet joints; positive response (>80% pain relief) predicts success with radiofrequency ablation for long-term pain control. Epidural steroid injections address cervical radiculopathy from disc herniation or foraminal stenosis, delivering anti-inflammatory medication directly to the inflamed nerve root.
Phase 4 (Surgical: Rarely Needed) is reserved for severe cases with progressive neurological deficits, confirmed structural pathology (large disc herniation compressing spinal cord or nerve root), or failure of 6+ months of comprehensive conservative care. Anterior cervical discectomy and fusion (ACDF) removes herniated disc material and fuses adjacent vertebrae, reliably decompressing neural structures. Artificial disc replacement preserves motion at the surgical level, potentially reducing adjacent segment degeneration. Surgical intervention is appropriate for less than 5% of whiplash patients; our goal is always maximum recovery through non-surgical means.
Our treatment selection is individualized based on Quebec Task Force Classification, presence of radiculopathy, patient functional goals, and response to initial interventions. We provide comprehensive documentation for your attorney including causation analysis, treatment plans, and prognosis statements.


Acute Phase (Days 1-14)
1-2 weeksPain control, inflammation reduction, gentle mobility. NSAIDs, muscle relaxants, ice/heat therapy, soft collar (3-5 days max). Active recovery emphasis.
Subacute Phase (Weeks 2-8)
2-8 weeksActive rehabilitation with physical therapy, chiropractic adjustments, massage therapy. Progressive strengthening, range of motion restoration, postural correction.
Intermediate Phase (Weeks 8-16)
8-16 weeksInterventional procedures for persistent pain. Trigger point injections, facet joint injections, medial branch blocks, epidural steroid injections.
Surgical Phase (If Needed)
Case dependentReserved for progressive neurological deficits or failed conservative care. ACDF or artificial disc replacement. Less than 5% of cases.
Whiplash recovery follows predictable patterns correlated with injury severity, though individual variability exists based on age, pre-existing conditions, accident biomechanics, and treatment compliance. Understanding expected recovery timelines helps patients maintain realistic expectations and adhere to treatment protocols.
Grade 1 whiplash (neck pain without objective musculoskeletal signs) typically resolves in 6-12 weeks with conservative care. These patients experience complete functional recovery and return to pre-injury activities without restrictions. Pain decreases progressively with occasional minor flares during physical therapy progression.
Grade 2 whiplash (neck pain with musculoskeletal signs like restricted range of motion or point tenderness) requires 3-6 months for substantial recovery. Most patients achieve 80-90% improvement by 3 months with appropriate treatment, with residual symptoms manageable through self-care. Return to work occurs at 4-8 weeks depending on job demands—sedentary work earlier than labor-intensive positions. Functional capacity evaluations at 8-12 weeks objectively document work capabilities.
Grade 3 whiplash (neck pain with neurological signs including radiculopathy or cord compression) demands 6-12+ months for recovery, with some patients experiencing permanent limitations. Neurological recovery progresses slower than musculoskeletal healing; nerve regeneration occurs at approximately 1mm per day. Patients with confirmed nerve root compression may require 4-6 months to regain normal strength and sensation even after successful treatment. A subset develops chronic whiplash-associated disorder (WAD) with persistent symptoms beyond 6 months, requiring ongoing pain management and functional restoration.
Factors predicting prolonged recovery include high initial pain intensity (VAS >6/10), rapid onset of symptoms (<24 hours), presence of radicular symptoms, older age (>40 years), female gender (smaller neck musculature provides less protection), pre-existing cervical degenerative changes, rear-end collision mechanism, and delayed treatment initiation (>72 hours post-injury). Conversely, early mobilization, compliance with physical therapy, psychological resilience, and prompt treatment access predict favorable outcomes.
Recovery milestones we monitor include pain reduction (50% improvement by 4-6 weeks), range of motion improvement (within 10% of normal by 8 weeks), functional capacity (return to daily activities by 8-12 weeks), and return to work (light duty by 4-6 weeks, full duty by 8-16 weeks for most occupations). Our treatment approach accelerates progress through these milestones while preventing chronic pain development through comprehensive care addressing all injury components.
Comprehensive medical documentation is crucial for personal injury claims, insurance negotiations, and potential litigation. AccidentDoc Pasadena provides detailed documentation specifically designed for legal proceedings, going beyond standard medical records to establish causation, document disability, and support damages claims.
Our initial evaluation documents the accident mechanism in detail, correlating biomechanical forces with observed injuries. We note the specific collision type (rear-end, side-impact, frontal), estimated speed if known, whether the patient was aware of impending impact (bracing muscles provides some protection), seatbelt use, airbag deployment, vehicle damage, and whether the patient could drive away or required ambulance transport. This narrative establishes the temporal relationship between accident and injury onset, critical for proving causation.
Physical examination findings are documented with specificity: cervical range of motion measured in degrees using goniometry (normal: flexion 50°, extension 60°, rotation 80°, lateral flexion 45°), exact location of muscle tenderness and spasm, vertebral point tenderness at specific levels (e.g., "exquisite tenderness to palpation over C5 and C6 spinous processes"), neurological examination results including specific myotomes and dermatomes affected, and positive provocative tests with descriptions (e.g., "Spurling's test right side reproduced right arm radicular pain in C6 distribution").
Diagnostic imaging results are incorporated with clinical correlation: "MRI cervical spine dated [DATE] reveals C5-C6 disc herniation with rightward lateral component causing moderate right neural foraminal stenosis, consistent with patient's C6 radiculopathy characterized by right arm pain, biceps weakness, and diminished sensation over the radial forearm." This correlation between imaging findings and clinical presentation strengthens causation arguments.
Treatment plans document not just what we're doing but why: "Patient requires physical therapy 3x weekly for 8 weeks to restore normal cervical lordosis, improve deep neck flexor strength, and address myofascial trigger points. Failure to treat comprehensively risks chronic pain syndrome development." Progress notes document objective functional improvements: "Cervical rotation improved from 40° to 65° bilaterally. Patient now able to check blind spots while driving, previously impossible."
Causation statements explicitly link injuries to the accident: "It is my professional opinion within a reasonable degree of medical certainty that this patient's cervical spine injuries including C5-C6 disc herniation, cervical facet syndrome, and myofascial pain syndrome are directly and proximately caused by the motor vehicle collision of [DATE]. The documented mechanism (rear-end collision with sudden hyperextension-hyperflexion) is consistent with and sufficient to cause the observed injuries."
Disability ratings and restrictions are provided when maximum medical improvement (MMI) is reached: "Patient has reached MMI with 15% permanent partial impairment of the cervical spine per AMA Guides to the Evaluation of Permanent Impairment, 6th Edition. Permanent restrictions include: no overhead work, no lifting >25 lbs, frequent breaks from static postures, no work requiring sustained neck rotation."
Prognostic statements inform settlement negotiations: "Patient likely requires ongoing pain management including occasional trigger point injections and maintenance physical therapy. Future medical costs estimated at $2,500-3,500 annually. Risk of accelerated cervical degenerative changes (post-traumatic arthritis) is moderate to high, potentially requiring surgical intervention in 10-15 years."
We also provide expert witness testimony when needed, appearing for depositions or trial testimony to explain injuries, treatment, causation, and prognosis to attorneys, insurance adjusters, and juries. Our documentation is prepared with litigation in mind from day one, ensuring your attorney has the strongest possible medical evidence supporting your claim.
- Detailed accident mechanism documentation correlating forces with injuries
- Objective physical examination findings with measurements and specific locations
- Diagnostic imaging results with clinical correlation to symptoms
- Comprehensive treatment plans with medical necessity justification
- Causation statements linking injuries to accident within reasonable medical certainty
- Disability ratings using AMA Guides when at maximum medical improvement
- Work restrictions and functional capacity documentation
- Prognosis statements including future medical needs and costs
- Expert witness availability for depositions and trial testimony
While most whiplash injuries are managed on an outpatient basis through our clinic, certain symptoms indicate potentially serious complications requiring emergency department evaluation. Patients and family members should be educated to recognize these red flags and seek immediate care when present.
Neurological emergency signs include progressive arm numbness or weakness (suggests worsening nerve root compression or spinal cord injury), bilateral arm symptoms (indicates central spinal cord involvement rather than isolated nerve root), bowel or bladder dysfunction including urinary retention or incontinence (cauda equina syndrome or central cord syndrome), lower extremity weakness or numbness (cervical myelopathy from spinal cord compression), and difficulty with balance or coordination (posterior column involvement or vertebral artery injury).
Vascular emergency signs include severe headache with sudden onset reaching maximum intensity within seconds ("thunderclap headache" suggests vertebral artery dissection or subarachnoid hemorrhage), headache with vision changes such as double vision, visual field cuts, or transient blindness (posterior circulation stroke from vertebral artery injury), dizziness with dysphagia (difficulty swallowing), dysarthria (slurred speech), or facial numbness (brainstem stroke), and Horner's syndrome (ptosis, miosis, anhidrosis indicating sympathetic chain disruption from carotid or vertebral artery dissection).
Infectious warning signs include fever >101°F with neck pain and stiffness (meningitis, though rare after trauma), increasing pain despite treatment with constitutional symptoms like fever and night sweats (discitis or epidural abscess, typically developing weeks after penetrating injury or iatrogenic seeding).
Structural instability signs include severe pain with any neck movement suggesting instability, palpable cervical deformity or step-off (fracture-dislocation), and severe pain that is completely unrelenting despite all conservative measures (possible occult fracture).
When any of these red flag symptoms develop, we instruct patients to proceed immediately to the emergency department, preferably one with neurosurgery capabilities. Memorial Hermann Southeast Hospital, Houston Methodist Baytown Hospital, and Clear Lake Regional Medical Center all have neurosurgical coverage and advanced imaging available 24/7. After emergency stabilization and treatment, patients return to our care for ongoing management coordinated with the emergency intervention.
- Progressive arm numbness, weakness, or bilateral arm symptoms (nerve/cord injury)
- Bowel or bladder dysfunction - urinary retention or incontinence (cauda equina)
- Lower extremity weakness or numbness (cervical myelopathy)
- Sudden severe "thunderclap" headache (vertebral artery dissection)
- Headache with vision changes, double vision, or visual field defects (stroke)
- Dizziness with swallowing difficulty, slurred speech, or facial numbness (brainstem)
- Horner's syndrome - drooping eyelid, small pupil, no sweating on one side (arterial injury)
- Fever >101°F with neck stiffness (infection)
- Severe unrelenting pain despite all treatments (possible fracture)
- Difficulty with balance or coordination (posterior column or cerebellar involvement)
While many accidents are unavoidable, certain strategies reduce whiplash risk and severity. Proper headrest positioning is critical: the headrest should be adjusted so its top is level with the top of your head, positioned 2-3 inches from the back of your skull. This minimizes head travel distance during rear-end impacts. Studies show optimal headrest position reduces whiplash risk by up to 40%.
Maintaining good posture while driving—sitting upright with ears aligned over shoulders rather than forward head posture—provides better cervical spine alignment to withstand impact forces. Strengthening neck muscles through targeted exercises creates muscular protection. Awareness of surroundings and anticipating potential collisions allows protective muscle bracing, though this requires seeing the impending impact.
Post-injury self-care accelerates recovery: maintain gentle activity rather than prolonged immobilization, perform prescribed home exercises consistently, apply ice/heat as directed (ice for acute flares, heat for chronic stiffness), practice good sleep posture using cervical contour pillows, avoid prolonged static postures like computer work without breaks, and attend all scheduled therapy appointments. Ergonomic workstation setup prevents symptom exacerbation in office workers: monitor at eye level, keyboard positioned to keep elbows at 90°, lumbar support, and frequent posture changes every 30 minutes. These strategies combined with our comprehensive treatment approach optimize recovery and prevent chronic disability.
Seek Emergency Care Immediately If You Experience:
- Progressive arm numbness, weakness, or bilateral arm symptoms
- Bowel or bladder dysfunction (urinary retention or incontinence)
- Sudden severe "thunderclap" headache with vision changes
- Dizziness with difficulty swallowing or slurred speech
- Fever >101°F with neck stiffness
- Horner's syndrome (drooping eyelid, small pupil, facial asymmetry)
- Lower extremity weakness or difficulty walking
- Severe unrelenting pain despite all treatment measures
Call 911 or go to the nearest emergency room immediately
Back Pain & Spinal Injuries

Lower back pain affects 80% of Americans at some point in their lives, with car accidents, workplace injuries, and slip-and-falls being leading causes of acute spinal trauma. The lumbar spine bears tremendous compressive and rotational forces during accidents, making it vulnerable to disc herniations, facet joint injuries, and muscular strains. AccidentDoc Pasadena's physicians employ comprehensive diagnostic and treatment protocols to address both acute injury and prevent chronic disability.
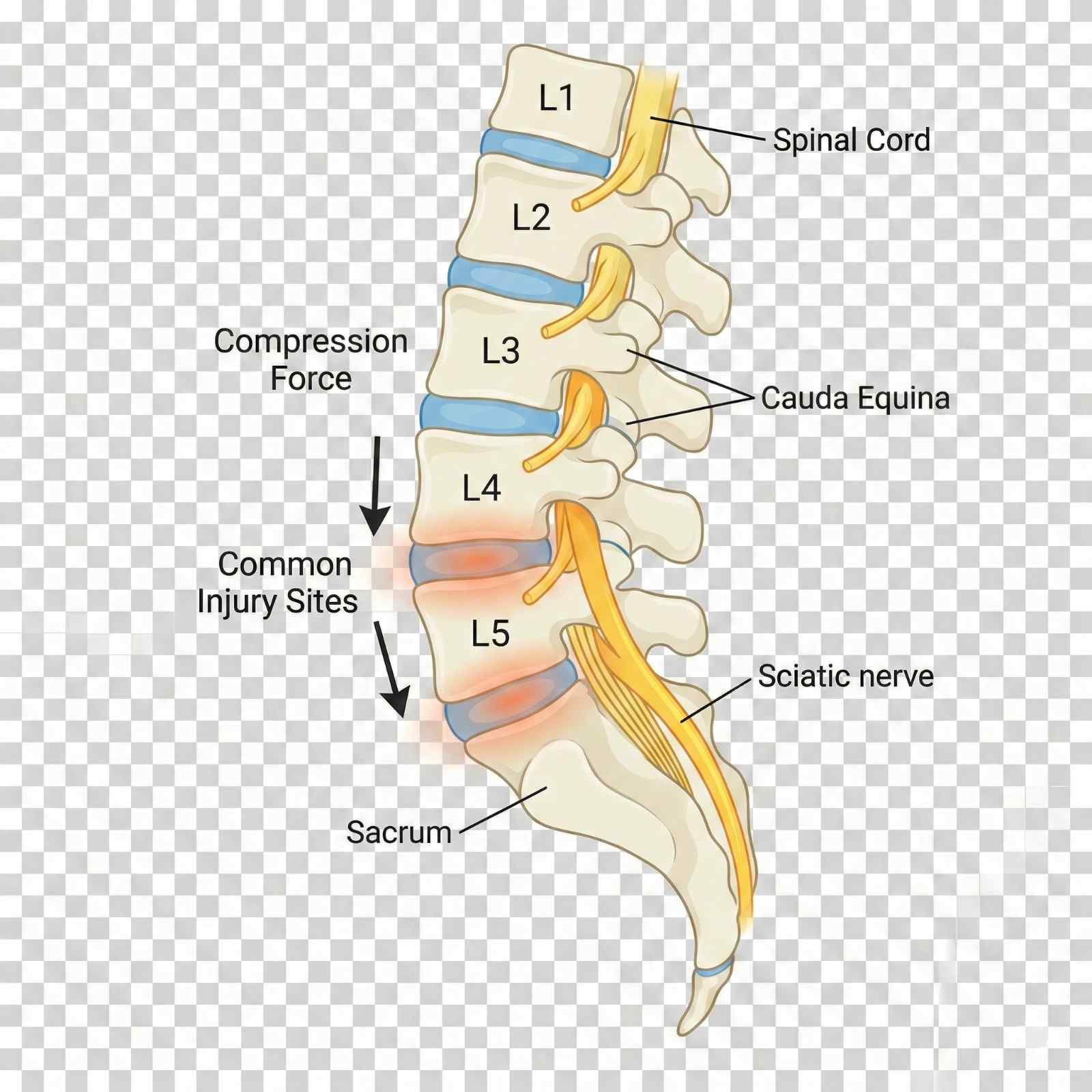
The lumbar spine consists of five vertebrae (L1-L5) plus the sacrum (S1), bearing the body's full weight during standing, walking, and lifting. Each motion segment includes the vertebral body, intervertebral disc, paired facet joints, ligamentous structures (anterior and posterior longitudinal ligaments, ligamentum flavum, interspinous and supraspinous ligaments), and surrounding musculature (erector spinae, multifidus, transversospinalis). The spinal canal houses the conus medullaris (spinal cord ending at L1-L2) and cauda equina (nerve roots L2-S5), with nerve roots exiting through neural foramina at each level.
Intervertebral discs are the spine's primary shock absorbers, consisting of a gelatinous nucleus pulposus surrounded by the tough annulus fibrosus. During compression forces typical of car accidents—particularly rear-end collisions where the torso is thrown into the seatback—the nucleus pulposus experiences tremendous pressure. If annular fibers are weakened by age-related degeneration or suddenly overloaded, the nucleus can herniate through the annular tear, typically in a posterolateral direction where annular fibers are thinnest and posterior longitudinal ligament support is minimal.
Facet joints are true synovial joints located posteriorly at each spinal level, guiding and limiting spinal motion. They are richly innervated by medial branch nerves and can generate significant pain when injured through capsular tears, cartilage damage, or inflammation. Rotational injuries during side-impact collisions or slip-and-falls particularly stress facet joints, as they limit rotational motion in the lumbar spine.
The L4-L5 and L5-S1 motion segments experience the greatest biomechanical stress due to their position at the lumbosacral junction, where the lumbar spine meets the relatively immobile sacrum. Approximately 95% of lumbar disc herniations occur at these two levels. The L5 nerve root (exiting at L4-L5) and S1 nerve root (exiting at L5-S1) are most commonly compressed, producing characteristic sciatica patterns: L5 radiculopathy causes dorsiflexion weakness (foot drop), lateral leg and dorsal foot numbness, and pain radiating down the posterior thigh and lateral leg. S1 radiculopathy causes plantarflexion weakness (difficulty standing on toes), posterior leg and plantar foot numbness, and pain radiating down the posterior leg to the heel.
Musculoligamentous injuries occur when sudden forces exceed tissue tolerances: multifidus and erector spinae muscles undergo eccentric overload during sudden deceleration, producing tears ranging from microscopic fiber disruption to complete muscle rupture. Ligamentous injuries involve the posterior ligamentous complex (supraspinous ligament, interspinous ligament, ligamentum flavum) and can create subtle spinal instability not always visible on static imaging.
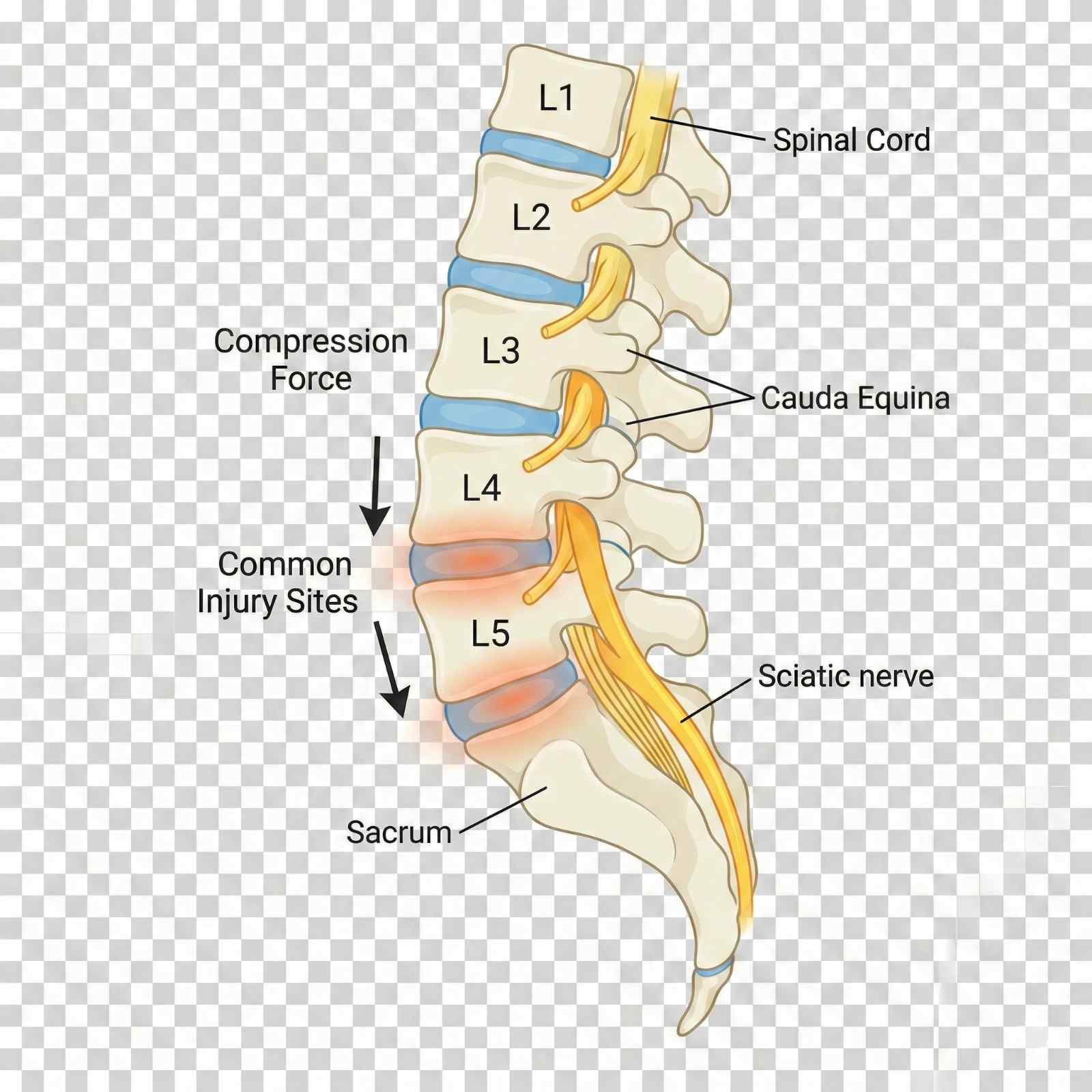
Compressive loading from rear-end and frontal collisions represents the most common mechanism of lumbar injury in motor vehicle accidents. When the vehicle suddenly decelerates, the torso continues forward until restrained by the seatbelt, creating compressive and flexion forces on the lumbar spine. These forces can exceed 3,000 Newtons, sufficient to cause annular tears and disc herniations. The L4-L5 disc, positioned at the apex of lumbar lordosis, experiences maximal stress and is most frequently injured.
Lifting injuries in workplace settings account for substantial lumbar spine trauma, particularly in warehouse, construction, and healthcare workers. Improper lifting mechanics—bending at the waist rather than knees, twisting while lifting, or sudden unexpected loads—create asymmetric compressive and rotational forces exceeding disc and ligament tolerances. The Occupational Safety and Health Administration (OSHA) estimates that overexertion injuries, primarily lumbar strain and disc injuries, cost American businesses $15.1 billion annually in workers' compensation claims.
Slip-and-fall accidents generate unique injury patterns depending on landing position: landing on the buttocks creates axial loading through the sacrum, potentially causing sacral fractures, L5-S1 disc injury, or compression fractures in osteoporotic vertebrae. Landing on the side produces lateral compression and rotational forces, injuring facet joints and causing transverse process fractures. The sudden unexpected nature of falls prevents protective muscle activation, allowing full force transmission to skeletal structures.
Repetitive bending, twisting, and lifting in occupations like construction, refinery work, and warehouse operations causes cumulative trauma to lumbar discs. Each loading cycle causes microscopic annular fiber tears; when accumulated over months to years, these coalesce into macroscopic defects allowing nuclear herniation. Even without a specific acute event, workers develop symptomatic disc herniations that are compensable under Texas workers' compensation law as cumulative trauma injuries.
In Pasadena's industrial corridor along Highway 225, refinery and petrochemical workers experience unique mechanisms including falls from height, being struck by falling equipment or materials, and crush injuries from machinery. These high-energy mechanisms often cause multiple-level injuries, fractures, and combined bone-soft tissue trauma requiring comprehensive multidisciplinary care.
- Motor vehicle accidents (rear-end and frontal) - compression and flexion forces
- Lifting injuries with improper mechanics - twisting, bending, unexpected loads
- Slip-and-fall on buttocks - axial loading through sacrum to L5-S1
- Repetitive occupational bending and lifting - cumulative disc trauma
- Falls from height - high-energy compression and fracture risk
- Industrial accidents - crush injuries, being struck by objects
- 18-wheeler accidents - severe multi-level injuries from high forces
Lumbar spine injury symptoms range from localized mechanical back pain to severe radiculopathy with neurological deficits, depending on involved structures. Understanding this symptom spectrum guides diagnostic workup and treatment selection.
Mechanical low back pain from muscular strain and facet joint injury manifests as localized lumbar discomfort, often described as deep aching or sharp with movement. Pain worsens with extension (bending backward, overhead reaching) in facet-mediated pain, and with flexion (forward bending, sitting) in discogenic pain. Muscle spasm is palpable as firm, tender bands in the paraspinal muscles, representing protective guarding. Range of motion is restricted, particularly in the direction stressing injured structures. Mechanical pain typically remains localized to the back and buttocks without leg radiation.
Sciatica, the hallmark of nerve root compression, presents as sharp, burning, or electric pain radiating from the lower back down the posterior or lateral thigh, through the calf, and into the foot. The pain distribution follows specific dermatomal patterns: L5 radiculopathy produces lateral leg and dorsal foot pain, while S1 radiculopathy causes posterior leg and plantar foot pain. Patients often describe the pain as "shooting" or "like an electric shock," distinctly different from muscular aching. The pain intensity often exceeds back pain, and patients report that leg pain is their primary complaint.
Neurological symptoms accompany more severe nerve compression: numbness or paresthesias (tingling) in dermatomal distributions, weakness in specific muscle groups (L5: foot dorsiflexion and toe extension; S1: plantarflexion and toe flexion), and reduced or absent deep tendon reflexes (L5: medial hamstring; S1: Achilles). These neurological deficits indicate need for prompt MRI and potentially urgent intervention if progressive.
Cauda equina syndrome represents a surgical emergency requiring immediate decompression, characterized by bilateral leg symptoms, saddle anesthesia (numbness in the perineal region), bowel or bladder dysfunction (urinary retention most common initially, followed by overflow incontinence), and progressive bilateral leg weakness. Though rare (occurring in 1-2% of large disc herniations), cauda equina syndrome risk necessitates education of all patients with severe sciatica about warning signs.
Delayed symptom onset is common in lumbar injuries: patients may feel "fine" immediately after accidents, only to develop severe pain 24-48 hours later as inflammation peaks. This delayed onset doesn't invalidate causation—it reflects the natural inflammatory timeline following soft tissue injury.
| Symptom | Timing / Description |
|---|---|
| Localized low back pain | Immediate to Delayed |
| Pain with forward bending | Immediate to Delayed |
| Pain with backward bending | Immediate to Delayed |
| Sciatica (leg pain) | Delayed (24-72 hours) |
| Leg numbness/tingling | Delayed to Chronic |
| Foot drop (L5) | Delayed to Chronic |
| Difficulty standing on toes (S1) | Delayed to Chronic |
| Reduced reflexes | Delayed to Chronic |
| Bilateral leg symptoms | Emergency |
| Bowel/bladder dysfunction | Emergency |
Comprehensive diagnostic evaluation combines clinical assessment with targeted imaging to identify all injured structures and guide treatment decisions. Our systematic approach ensures accurate diagnosis while avoiding unnecessary testing.
Clinical examination begins with observing gait, posture, and spinal contour—loss of normal lumbar lordosis suggests muscle spasm and protective guarding. Active range of motion testing quantifies functional limitations: forward flexion (normal: fingers to floor or within 10cm), extension (normal: 25-30°), lateral flexion (normal: 25-30° each side), and rotation (normal: 30-45° each direction, though limited in lumbar spine). We use goniometry or inclinometry for objective documentation supporting disability ratings.
Palpation identifies point tenderness over spinous processes (suggesting fracture, ligament injury, or facet pathology), paraspinal muscle spasm and trigger points, and sacroiliac joint tenderness (commonly injured in falls on buttocks). Percussion over spinous processes elicits pain in vertebral fractures. Straight leg raise test (SLR) is the gold standard provocative maneuver for lumbar radiculopathy: with the patient supine, we slowly raise the extended leg; pain radiating below the knee between 30-70° of elevation indicates nerve root tension, highly specific for disc herniation when the pain is reproduced in the contralateral leg (crossed SLR). Femoral nerve stretch test (patient prone, knee flexed, hip extended) reproduces anterior thigh pain in upper lumbar radiculopathy (L2-L4).
Neurological examination systematically assesses motor function (manual muscle testing of hip flexors L2, quadriceps L3/L4, ankle dorsiflexion L5, ankle plantarflexion S1), sensory function (light touch and pinprick in all dermatomes), and reflexes (patellar L4, medial hamstring L5, Achilles S1). Documentation notes specific findings: "4/5 strength ankle dorsiflexion right, 2+ Achilles reflex left vs 0 right, sensory deficit plantar foot S1 distribution right—consistent with S1 radiculopathy."
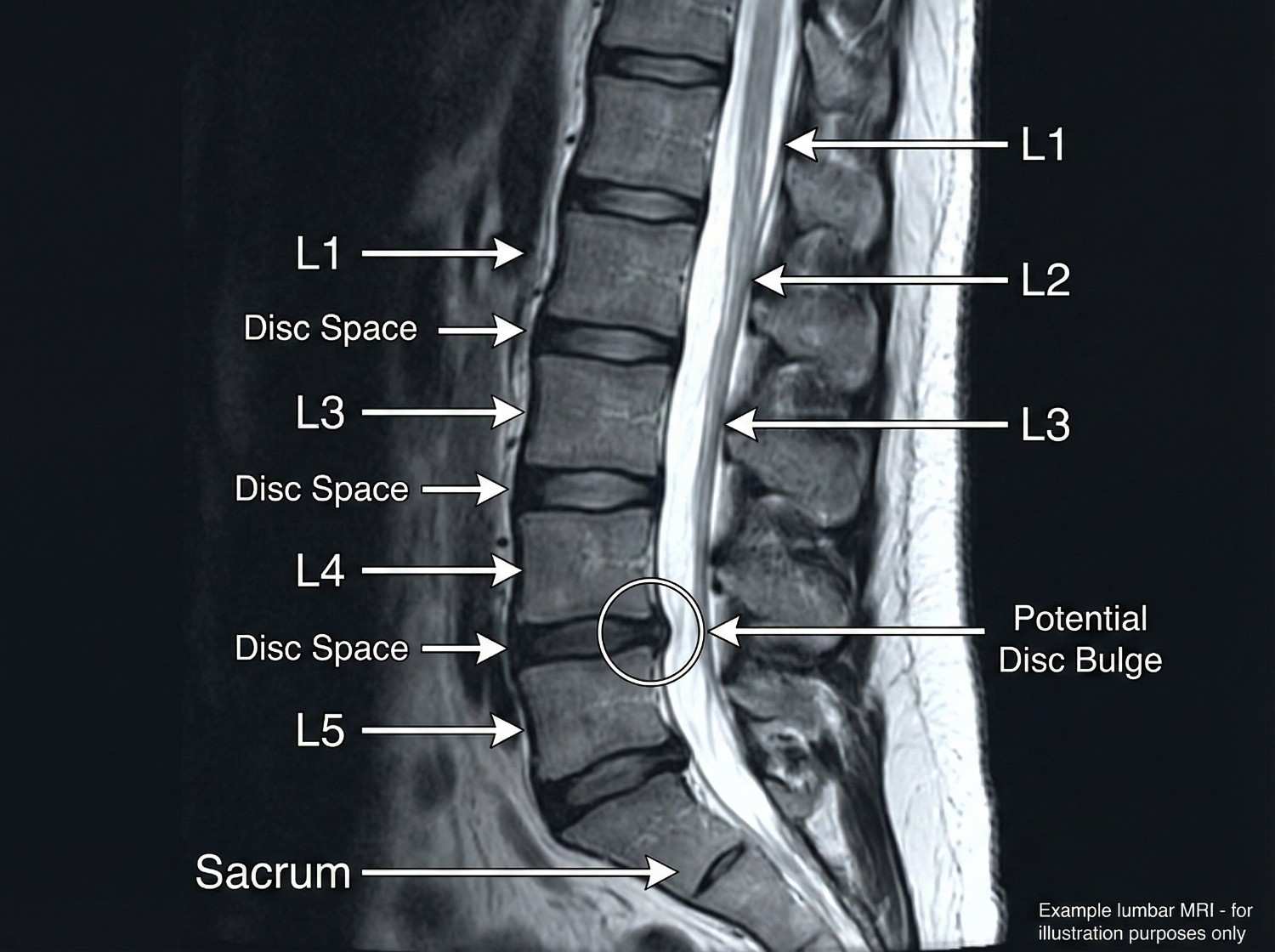
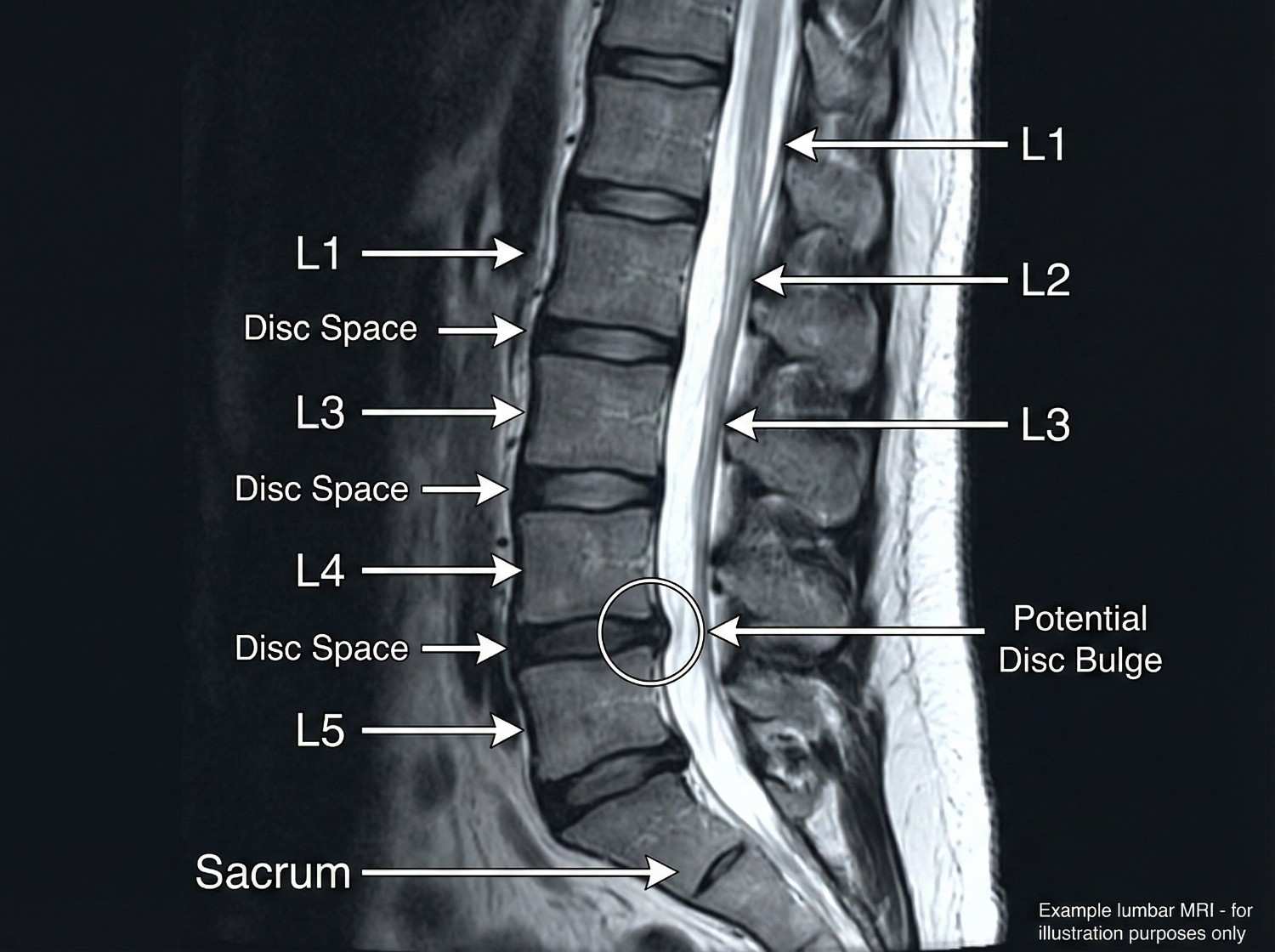
Imaging selection follows evidence-based guidelines: Lumbar X-rays (AP and lateral views) are initial studies to assess alignment, measure disc space heights (narrowing suggests degeneration), identify fractures or spondylolisthesis (vertebral slippage), and evaluate for degenerative changes. Flexion-extension views assess spinal stability when ligamentous injury is suspected. X-rays have limited utility for soft tissue evaluation but are valuable for initial screening.
MRI lumbar spine without contrast is the definitive study for disc herniations, nerve root compression, spinal stenosis, ligamentous injuries, and bone marrow edema indicating fractures. We order MRI when radicular symptoms exist, neurological deficits are present, severe pain persists beyond 4-6 weeks of conservative care, or red flag symptoms suggest serious pathology (cauda equina, infection, malignancy). MRI findings are correlated with clinical presentation—incidental disc bulges without nerve compression don't explain radicular symptoms, while a right posterolateral disc herniation compressing the right S1 nerve root perfectly explains right S1 radiculopathy.
CT scanning provides superior bony detail for fractures, pars defects (spondylolysis), and bony stenosis, but lacks MRI's soft tissue resolution. CT myelography (CT after intrathecal contrast injection) is reserved for patients unable to undergo MRI (pacemakers, certain metal implants) when soft tissue visualization is necessary.
Electrodiagnostic studies (EMG/NCS) performed 3-4 weeks post-injury detect physiological nerve injury even when MRI shows anatomical compression. Abnormal findings include fibrillation potentials and positive sharp waves (denervation), reduced motor unit recruitment (weakness), and slowed nerve conduction velocities. EMG differentiates radiculopathy from peripheral nerve entrapments (peroneal nerve palsy mimics L5 radiculopathy) and polyneuropathy.
Our evidence-based treatment protocols progress through phases based on injury severity, patient response, and functional goals. All care is available through Letter of Protection with $0 out-of-pocket cost.
Phase 1 (Acute: Days 1-10) emphasizes controlled activity, not bed rest. Research demonstrates that prolonged bed rest delays recovery and increases chronic pain risk; we recommend limiting bed rest to 2-3 days maximum. Activity modification avoids pain-provoking movements (heavy lifting, prolonged sitting, twisting) while maintaining general activity. Ice application (20 minutes every 2-3 hours) reduces inflammation in the first 48 hours, then alternating ice/heat provides symptomatic relief. Medication includes NSAIDs (ibuprofen 800mg TID or naproxen 500mg BID) for inflammation, muscle relaxants (cyclobenzaprine 5-10mg at bedtime, tizanidine 4mg TID) for muscle spasm, and neuropathic pain medications (gabapentin, pregabalin) for radiculopathy. Short-course oral corticosteroids (methylprednisolone dose pack) provide potent anti-inflammatory effect for severe radiculopathy.
Phase 2 (Subacute: Weeks 2-8) introduces active rehabilitation. Physical therapy employs multiple modalities: McKenzie method (repeated extension exercises) centralizes pain from the leg back to the central spine, indicating favorable prognosis; core stabilization strengthens transversus abdominis, multifidus, and other deep stabilizers that protect the spine; manual therapy including soft tissue mobilization and joint mobilization improves mobility; and functional training retrains proper movement patterns for daily activities and work tasks. A typical protocol involves 2-3 sessions weekly for 6-8 weeks.
Chiropractic care utilizes flexion-distraction technique (Cox technique) which gently stretches the lumbar spine, creating negative intradiscal pressure that may reduce disc herniations while mobilizing facet joints. High-velocity low-amplitude (HVLA) adjustments restore normal joint motion in restricted segments. Side-posture manipulation is employed cautiously in acute disc herniation, prioritizing flexion-distraction initially. Treatment frequency typically starts at 3x weekly, tapering to 2x then 1x weekly as symptoms improve.
Massage therapy addresses secondary myofascial dysfunction: gluteus medius, piriformis, quadratus lumborum, and erector spinae often develop trigger points and hypertonicity secondary to primary lumbar pathology. Deep tissue massage, myofascial release, and trigger point therapy reduce muscle pain and improve flexibility, allowing more effective participation in strengthening exercises.
Phase 3 (Intermediate: Weeks 8-16) employs interventional procedures when conservative care provides inadequate relief. Epidural steroid injections are the gold standard for radiculopathy from disc herniation. Performed under fluoroscopic guidance, we deliver corticosteroid and local anesthetic directly to the inflamed nerve root via transforaminal (most specific, targets individual nerve root), interlaminar (midline approach, broader coverage), or caudal (through sacral hiatus, good for multi-level or S1 pathology) approaches. Success rates range from 50-70% for significant pain reduction lasting 3+ months, with best results in acute radiculopathy (<3 months duration) from contained disc herniations.
Facet joint injections target the zygapophyseal joints with fluoroscopically-guided injection of anesthetic and corticosteroid, both diagnostic (>80% pain relief confirms facet-mediated pain) and therapeutic. Medial branch blocks anesthetize the nerves innervating facet joints; patients achieving >80% pain relief for the duration of local anesthetic action are candidates for radiofrequency ablation. Radiofrequency ablation (RFA) uses thermal energy to create controlled lesions in medial branch nerves, providing 6-12 months of pain relief with repeatability. RFA is particularly effective for chronic facet-mediated pain unresponsive to conservative care.
Trigger point injections deliver local anesthetic (and sometimes corticosteroid) to hyperactive muscle trigger points in paraspinal, gluteal, and piriformis muscles, providing immediate pain relief and allowing advancement of physical therapy. Sacroiliac joint injections address SI joint dysfunction common after falls on buttocks or asymmetric loading patterns.
Phase 4 (Surgical: When Conservative Care Fails) is considered after 6+ months of comprehensive non-surgical treatment without adequate improvement, or sooner if progressive neurological deficits, cauda equina syndrome, or severe functional impairment exist. Microdiscectomy is the gold standard for disc herniation with radiculopathy, involving microscopic removal of herniated disc material compressing the nerve root. Success rates exceed 85-90% for leg pain relief, though back pain improves less reliably. Laminectomy removes bone (lamina) to decompress spinal canal stenosis causing neurogenic claudication. Spinal fusion stabilizes painful motion segments using bone graft and instrumentation (pedicle screws and rods), appropriate for spondylolisthesis, instability, or severe degenerative disc disease after failed conservative care.


Acute Phase (Days 1-10)
1-10 daysControlled activity (bed rest <3 days), ice/heat, NSAIDs, muscle relaxants, neuropathic pain medication. Activity modification avoiding pain triggers.
Subacute Phase (Weeks 2-8)
2-8 weeksPhysical therapy (McKenzie method, core stabilization), chiropractic (flexion-distraction, HVLA), massage therapy for myofascial pain. 2-3x weekly.
Intermediate Phase (Weeks 8-16)
8-16 weeksInterventional procedures: epidural steroid injections, facet injections, medial branch blocks, radiofrequency ablation, trigger point injections.
Surgical Phase (If Needed)
Case dependentMicrodiscectomy for disc herniation, laminectomy for stenosis, fusion for instability. After 6+ months conservative care or if progressive neurological deficits.
Lumbar spine injury recovery varies significantly based on specific pathology, severity, patient age, baseline fitness, and psychosocial factors including job satisfaction and litigation status. Understanding expected timelines helps maintain realistic expectations.
Lumbar muscle strain (no radiculopathy, no disc herniation) typically resolves in 6-8 weeks with conservative care. Most patients achieve 80% improvement by 4 weeks, with residual discomfort managed through home exercise and occasional NSAIDs. Return to sedentary work occurs at 2-3 weeks with activity modification; return to heavy labor at 6-8 weeks with gradual job conditioning.
Lumbar disc herniation with radiculopathy follows a longer course: natural history studies show that 60-70% of patients improve significantly with non-surgical care over 3-6 months. Initial severe leg pain typically improves first (within 4-8 weeks), followed by neurological recovery (strength, sensation) over 2-4 months. Approximately 10-15% of patients undergo surgery due to either failure of conservative care (persistent severe pain and disability) or progressive neurological deficits. Post-surgical recovery from microdiscectomy typically allows return to light work at 4-6 weeks, heavy work at 3 months, with continued improvement to one year.
Chronic low back pain (>3 months duration) requires multifaceted treatment addressing physical deconditioning, pain psychology, and functional restoration. Functional restoration programs combining intensive physical therapy, cognitive-behavioral therapy, and work conditioning produce superior outcomes compared to passive treatment modalities, with 65-75% of patients returning to pre-injury work status within 6 months of program completion.
Spinal fusion recovery is prolonged: bony fusion consolidation requires 6-12 months, though functional recovery allows desk work at 6-8 weeks, light physical work at 3-4 months, and unrestricted activity at 6-9 months post-surgery. Fusion at one level increases adjacent segment stress by approximately 30-40%, potentially accelerating degeneration at adjacent levels with 20-30% of patients developing adjacent segment disease within 10 years.
Factors predicting prolonged recovery include high initial pain intensity, widespread pain beyond primary injury site, catastrophic thinking and fear-avoidance beliefs, job dissatisfaction or workplace conflict, pending litigation (though treatment shouldn't be delayed), smoking (impairs tissue healing), obesity (increases mechanical spine loading), and pre-existing degenerative changes. Conversely, positive prognostic factors include rapid initial improvement (>30% pain reduction in first 2 weeks), good treatment compliance, strong social support, satisfying job with supportive employer, non-smoking status, and healthy body weight.
We monitor specific functional milestones: walking tolerance (goal: 30+ minutes continuous), sitting tolerance (goal: 45-60 minutes before requiring position change), lifting capacity (progressively increasing from 5 lbs to job-specific requirements), and pain-free sleep. Functional capacity evaluations performed at 8-12 weeks objectively document work capabilities and restrictions, invaluable for workers' compensation and personal injury cases.

Comprehensive documentation for lumbar spine injuries requires correlation of mechanism, clinical findings, imaging results, and functional limitations. Our reports are specifically designed for legal proceedings, insurance negotiations, and workers' compensation claims.
Mechanism documentation establishes causation: "Patient sustained lumbar spine injury on [DATE] when struck from behind while stopped at traffic light on Red Bluff Road. The sudden deceleration and compressive loading of the lumbar spine in seated position is biomechanically consistent with and sufficient to cause the observed L5-S1 disc herniation." For workers' compensation cases: "Cumulative trauma from repetitive lifting of 50-75 lb boxes while employed as warehouse associate for [EMPLOYER] from 2020-2024 caused progressive annular deterioration and eventual L4-L5 disc herniation becoming symptomatic on [DATE]."
Physical examination findings are documented with quantification: "Lumbar forward flexion limited to 40° (normal 90°), extension 10° (normal 25°), right lateral flexion 15° (normal 25°). Positive straight leg raise test right side reproducing S1 radiculopathy at 35° elevation. Absent right Achilles reflex, 4/5 plantarflexion strength right, sensory deficit plantar foot S1 distribution. Positive facet loading test L4-L5 and L5-S1 bilaterally."
Imaging correlation strengthens causation arguments: "MRI lumbar spine dated [DATE] demonstrates large right posterolateral disc herniation at L5-S1 with moderate to severe right neural foraminal stenosis and displacement of the right S1 nerve root. These findings directly correlate with and explain the patient's clinical presentation of right S1 radiculopathy characterized by posterior leg pain radiating to heel, plantar foot numbness, reduced plantarflexion strength, and absent Achilles reflex."
Treatment documentation emphasizes medical necessity: "Patient requires epidural steroid injection at L5-S1 to reduce neural inflammation and facilitate participation in physical therapy. Conservative measures including 8 weeks of physical therapy, chiropractic care, and medication management have provided only partial relief (30% improvement per VAS). Without interventional treatment, patient faces high risk of chronic pain syndrome development and possible surgical necessity."
Causation opinions are stated clearly: "Within a reasonable degree of medical probability, this patient's L5-S1 disc herniation and resultant S1 radiculopathy are directly and proximately caused by the motor vehicle collision of [DATE]. The documented mechanism (sudden deceleration with compressive loading) is biomechanically consistent with disc herniation. The temporal relationship (symptoms developing within 24 hours of accident) supports causation. The patient had no prior history of lumbar radiculopathy or disc herniation, with prior medical records documenting only occasional mechanical back pain responsive to over-the-counter medication. The current condition represents new injury directly attributable to the accident."
Disability ratings using AMA Guides to Evaluation of Permanent Impairment, 6th Edition, are provided at maximum medical improvement: "Patient has reached MMI 14 months post-injury after conservative care and one-level microdiscectomy. Residual findings include: 25% loss of lumbar range of motion, persistent 4+/5 ankle plantarflexion weakness right, diminished S1 dermatomal sensation. Using DRE (Diagnosis-Related Estimate) Category III (radiculopathy with objective findings), patient has 13% whole person impairment." Permanent restrictions guide return-to-work planning: "Permanent restrictions include: lifting limited to occasional 25 lbs, frequent 15 lbs; no repetitive bending or twisting; no prolonged static postures (sitting/standing >45 minutes without position change); no work requiring prolonged driving; no climbing ladders or scaffolds."
Future medical needs and costs are estimated: "Patient will require ongoing pain management including episodic physical therapy (estimated 8-12 sessions annually), periodic epidural injections (1-2 annually), medication management, and possible additional surgery if adjacent segment degeneration develops (20-30% risk over 10 years, estimated cost $75,000-100,000)."
Life care planning for catastrophic injuries documents all future medical, therapeutic, and supportive care needs with associated costs over the patient's remaining lifetime, supporting economic damages claims in personal injury litigation.
- Mechanism documentation establishing biomechanical causation
- Quantified physical examination with range of motion measurements
- Imaging findings correlated with clinical presentation
- Treatment plans with medical necessity justification
- Causation opinions stated within reasonable medical probability
- Disability ratings per AMA Guides at maximum medical improvement
- Permanent work restrictions for return-to-work and vocational assessment
- Future medical needs and costs for life care planning
- Expert witness testimony availability for depositions and trial
Certain lumbar spine injury presentations indicate surgical emergencies or serious underlying pathology requiring immediate advanced care. Patient education about these red flags is critical for preventing permanent disability.
Cauda equina syndrome is a neurosurgical emergency caused by massive central disc herniation or other space-occupying lesion compressing multiple nerve roots of the cauda equina. Classic presentation includes bilateral leg pain and weakness (distinguishing it from typical unilateral radiculopathy), saddle anesthesia (numbness in the perineal region, inner thighs, and buttocks—areas that would contact a saddle), and bowel/bladder dysfunction initially presenting as urinary retention (inability to void despite full bladder sensation), progressing to overflow incontinence and fecal incontinence. Sexual dysfunction is also common. Cauda equina requires emergency MRI and surgical decompression within 24-48 hours; delays beyond 48 hours are associated with significantly increased rates of permanent bowel/bladder dysfunction and sexual impairment. Any patient presenting with bilateral leg symptoms and saddle symptoms should proceed immediately to an emergency department with neurosurgical coverage.
Progressive motor weakness, particularly rapid progression or weakness affecting multiple myotomes bilaterally, suggests either cauda equina syndrome or conus medullaris syndrome (injury to the spinal cord terminus at L1-L2). Isolated foot drop (L5) developing or worsening despite treatment warrants urgent MRI and possible surgical consultation, as prolonged nerve compression beyond 6-8 weeks reduces likelihood of neurological recovery even after successful decompression.
Bowel or bladder changes including urinary retention (most sensitive early sign of cauda equina), new onset urinary incontinence, fecal incontinence, or loss of rectal tone (assessed by digital rectal examination in emergency department) all mandate emergency evaluation. Patients should be instructed that difficulty initiating urination or decreased awareness of bladder fullness warrants immediate ER evaluation.
Fever with back pain raises concern for spinal infection including discitis (disc space infection), osteomyelitis (vertebral body infection), or epidural abscess. Risk factors include diabetes, immunosuppression, IV drug use, recent spine procedure/injection, or penetrating injury. Spinal infections can progress rapidly to neurological compromise and sepsis; immediate evaluation with MRI and laboratory studies (white blood cell count, erythrocyte sedimentation rate, C-reactive protein, blood cultures) is essential.
Nocturnal pain worse than daytime pain, particularly pain that awakens the patient from sleep and is not relieved by any position, raises concern for neoplasm (primary spinal tumor or metastatic disease). Constitutional symptoms including unexplained weight loss, fever, night sweats, or history of cancer increase suspicion. These patients require prompt MRI to evaluate for pathologic fracture, epidural tumor, or metastatic disease.
Significant trauma, especially in elderly patients or those with known osteoporosis, risks vertebral compression fractures. Acute severe back pain after fall, motor vehicle accident, or other trauma warrants X-rays initially; MRI is added if neurological symptoms develop or if fracture involves the posterior vertebral body (risk of retropulsed fragments compressing neural elements).
When any red flag symptom develops, we direct patients to emergency departments with neurosurgical capabilities: Memorial Hermann Southeast, Houston Methodist Baytown, Clear Lake Regional Medical Center, or Ben Taub Hospital for indigent patients. After emergency stabilization, patients return to our clinic for coordinated ongoing care.
- Cauda equina syndrome - bilateral leg pain/weakness, saddle anesthesia, urinary retention - SURGICAL EMERGENCY
- Progressive motor weakness, especially bilateral or multi-level
- Bowel or bladder dysfunction - incontinence or retention
- Fever with back pain - suggests infection (discitis, epidural abscess)
- Nocturnal pain worse than daytime - concern for neoplasm
- Unexplained weight loss, night sweats - systemic disease
- Significant trauma in elderly/osteoporotic patients - fracture risk
- Pain unrelieved by any position or intervention - severe pathology
- Bilateral leg numbness or weakness - central compression
- Loss of rectal tone or anal sphincter control - cauda equina
While many lumbar injuries result from unavoidable accidents, risk reduction strategies and proper ergonomics minimize injury severity and prevent chronic disability. Proper lifting mechanics are fundamental: always bend at knees rather than waist, keep load close to body (increasing lever arm by holding load away from body exponentially increases lumbar compression forces), avoid twisting while lifting (rotational forces maximally stress annulus fibrosus), and test load weight before committing to the lift. OSHA recommends limiting repetitive lifting to 51 lbs maximum for most workers, with lower limits (25 lbs) for frequent lifting.
Workplace ergonomics modifications include adjustable-height workstations allowing sit-stand alternation for office workers, anti-fatigue mats for workers in static standing positions, mechanical lifting aids (forklifts, pallet jacks, hoists) for material handling, team lifts for loads exceeding individual safe lifting limits, and job rotation to vary physical demands and prevent cumulative trauma. Core strengthening through targeted exercises creates muscular protection: transversus abdominis and multifidus provide spinal stability, while erector spinae, quadratus lumborum, and hip muscles contribute to load distribution. A basic core program includes planks, bird-dogs, dead bugs, and bridges performed 3-4x weekly.
Maintaining healthy body weight reduces chronic lumbar loading—each pound of excess abdominal weight creates amplified force on lumbar discs due to leverage effects. Smoking cessation improves disc nutrition (nicotine impairs blood flow to intervertebral discs) and enhances healing capacity. Post-injury, adherence to prescribed rehabilitation exercises prevents recurrence and chronic disability. Workplace accommodation through light duty assignments during recovery allows earlier return to work while respecting healing tissue limitations, reducing overall disability duration.
Seek Emergency Care Immediately If You Experience:
- Bilateral leg pain, weakness, or numbness (cauda equina syndrome)
- Saddle anesthesia - numbness in perineal area, inner thighs, buttocks
- Urinary retention, inability to void, or new incontinence
- Fecal incontinence or loss of bowel control
- Progressive motor weakness despite treatment
- Fever >101°F with back pain (possible infection)
- Nocturnal pain worse than daytime pain (possible tumor)
- Unexplained weight loss with back pain
- Significant trauma in elderly patients (fracture risk)
Call 911 or go to the nearest emergency room immediately
Need Treatment for Your Injuries?
Don't wait for your injuries to worsen. Get same-day evaluation and treatment from our accident injury specialists. We accept Letter of Protection—$0 out of pocket until your case settles.
Soft Tissue Damage

Soft tissue injuries encompassing muscles, tendons, and ligaments account for over 70% of all accident-related injuries. These injuries range from minor strains resolving in weeks to severe ruptures requiring surgical repair. Despite often lacking dramatic imaging findings, soft tissue injuries can cause substantial pain, functional impairment, and long-term disability. AccidentDoc Pasadena provides comprehensive evaluation and treatment of all soft tissue injury grades.
Soft tissues include all non-bony, non-neural structures: skeletal muscles that generate movement, tendons connecting muscles to bones, ligaments connecting bones to each other, and fascia providing structural support and force transmission. Understanding the grading system for soft tissue injuries guides treatment selection and prognosis.
Muscle injuries are classified by severity: Grade 1 (Mild Strain) involves microscopic muscle fiber tears with minimal loss of strength and function. Pain develops gradually and is typically manageable with over-the-counter medication. Swelling is minimal, and ecchymosis (bruising) is often absent. Patients maintain >80% of normal strength. Recovery typically occurs within 2-3 weeks with conservative care.
Grade 2 (Moderate Strain/Partial Tear) involves significant muscle fiber disruption with measurable loss of strength and function. A palpable defect or divot may be felt at the injury site. Pain is moderate to severe, especially with muscle activation. Swelling appears within 24-48 hours, and ecchymosis develops 2-5 days post-injury as blood dissects through tissue planes. Patients retain 50-80% of normal strength. Recovery requires 6-12 weeks including rehabilitation.
Grade 3 (Severe Strain/Complete Rupture) involves full-thickness muscle or musculotendinous junction tear with complete loss of function. A visible or palpable defect exists, often with bunching of the retracted muscle belly. Initial pain may be severe but can paradoxically decrease as torn nerve endings separate. Massive ecchymosis develops. Patients have <50% of normal strength or complete inability to contract the muscle. These injuries often require surgical repair, particularly in critical muscles like Achilles tendon, patellar tendon, or rotator cuff, with 3-6 month recovery.
Tendon injuries follow similar grading: Grade 1 (tendinopathy) involves inflammatory changes and microscopic fiber disruption without gross tear. Grade 2 (partial tear) involves significant fiber disruption with preserved continuity. Grade 3 (complete rupture) is full-thickness tear with loss of continuity, causing complete functional loss and requiring surgical repair in most locations.
Ligament sprains use the same three-grade classification: Grade 1 involves microscopic tears with preserved stability (stress testing shows normal joint stability). Grade 2 involves partial tear with mild-to-moderate laxity on stress testing but preserved endpoint. Grade 3 involves complete tear with marked laxity and absent endpoint, often requiring surgical reconstruction.
Contusions (bruises) result from direct trauma causing muscle crushing, capillary rupture, and hematoma formation without fiber tearing. They range from mild (minor pain, small hematoma) to severe (large intramuscular hematoma causing compartment-like pressure and possible myositis ossificans—heterotopic bone formation in muscle). Seatbelt contusions across the shoulder, chest, and abdomen are classic accident injuries, sometimes associated with underlying organ injury (liver or spleen in severe cases).

Soft tissue injuries result from multiple mechanisms in accident scenarios. Seatbelt trauma represents a unique injury pattern where the three-point restraint system loads soft tissues in a diagonal band across the chest, shoulder, and abdomen during sudden deceleration. The shoulder belt crosses the pectoralis major muscle, anterior deltoid, and trapezius, potentially causing strains or contusions. Chest wall contusions can extend to rib fractures or costochondral separation in severe impacts. Abdominal seatbelt injuries include rectus abdominis and oblique muscle strains, with severe cases causing bowel or mesenteric injury (seatbelt syndrome). The characteristic diagonal bruise pattern appearing 24-48 hours post-accident is pathognomonic for seatbelt loading.
Airbag deployment generates unique injuries through rapid inflation (deploying at 200+ mph). Upper extremity injuries occur when hands are positioned on the steering wheel in improper positions (10-and-2 versus recommended 9-and-3), with airbag impact causing wrist extension injuries, forearm contusions, and finger dislocations. Facial and chest contusions result from airbag contact, occasionally causing ocular injuries if eyeglasses shatter. Chemical burns from airbag propellant (sodium azide) can occur, presenting as erythematous rash on contact areas.
Dashboard and interior impacts cause location-specific injuries: knee impact against dashboard produces quadriceps contusions, patellar injuries, and posterior cruciate ligament tears (dashboard knee). Shoulder impact against door frames causes rotator cuff strains and contusions. Hip and thigh contusions occur from center console or door panel impacts. These injuries often present with massive ecchymosis developing over 3-5 days.
Slip-and-fall accidents generate injuries based on landing position and protective reflexes: landing on an outstretched hand (FOOSH injury) causes wrist and forearm soft tissue injuries plus possible fractures. Lateral falls produce hip, shoulder, and lateral thigh contusions. Catching oneself during a fall creates eccentric muscle loading (muscle lengthening under tension), particularly affecting quadriceps, hamstrings, and rotator cuff, leading to Grade 2 strains.
Workplace accidents including repetitive motion create overuse injuries: rotator cuff tendinopathy in overhead workers (painters, electricians, construction), lateral epicondylitis (tennis elbow) in tool users requiring repetitive wrist extension (carpentry, assembly work), and medial epicondylitis (golfer's elbow) in gripping activities. These cumulative trauma injuries are compensable under Texas workers' compensation when work activities are the major contributing cause.
Direct trauma from being struck by objects, equipment, or during falls creates contusions with potential complications including compartment syndrome (elevated pressure within fascial compartments compromising perfusion) requiring emergency fasciotomy, traumatic rhabdomyolysis (muscle breakdown releasing myoglobin causing acute kidney injury), and myositis ossificans (heterotopic bone formation in healing muscle hematoma).
- Seatbelt trauma - diagonal chest/shoulder contusions, abdominal strains
- Airbag deployment - upper extremity contusions, wrist extension injuries
- Dashboard/interior impacts - knee contusions, quadriceps strains, shoulder injuries
- Slip-and-fall - FOOSH injuries, hip contusions, eccentric muscle loading
- Workplace repetitive motion - rotator cuff tendinopathy, epicondylitis
- Direct trauma - struck by objects causing contusions and possible compartment syndrome
- Sports-type injuries during accidents - sudden acceleration/deceleration strains
Soft tissue injury symptoms follow a characteristic temporal pattern useful for diagnosis and patient education. Immediate symptoms (0-6 hours) include pain at the injury site, often described as sharp or aching, worsening with movement or palpation. Muscle spasm or cramping develops as protective splinting. Swelling is typically minimal immediately post-injury unless significant vascular disruption occurred. Range of motion is reduced due to pain and protective guarding. Strength is decreased if muscle fibers are torn, though initial adrenaline and pain-mediated guarding can mask true weakness.
Delayed symptoms (24-72 hours) often exceed initial symptoms as inflammatory cascade peaks. Swelling becomes apparent as capillary permeability increases and inflammatory mediators accumulate. Ecchymosis (bruising) appears, typically 2-5 days post-injury, as extravasated blood dissects through tissue planes and breaks down. Bruise color evolution follows a predictable pattern: red-purple initially (oxyhemoglobin), blue-purple days 1-3 (deoxyhemoglobin), green days 4-6 (biliverdin), yellow-brown days 7+ (bilirubin and hemosiderin). Stiffness peaks in morning or after prolonged static postures as inflammatory exudate accumulates during immobility.
Functional limitations depend on injury location and severity: shoulder injuries impair overhead reaching, dressing, and hair grooming. Elbow and forearm injuries affect lifting, carrying, and keyboard use. Hip and quadriceps injuries impair stair climbing, rising from chairs, and squatting. Hamstring injuries affect walking speed, running, and bending. Seemingly minor soft tissue injuries can cause substantial functional impairment and work disability, particularly in labor-intensive occupations.
Chronic symptoms develop when acute injuries aren't properly rehabilitated: persistent weakness from inadequate strengthening allows compensatory movement patterns stressing other structures. Adhesions and scar tissue formation in healing muscle limits flexibility and creates pain with stretching. Tendinopathy develops from inadequately healed tendon undergoing repetitive loading before tissue remodeling completes. Chronic pain syndromes including myofascial pain with trigger points can perpetuate pain months to years after initial injury.
Physical examination reveals specific findings: palpable muscle spasm or taut bands, point tenderness at the injury site, possible palpable defect or gap in Grade 2-3 injuries, ecchymosis with characteristic distribution, reduced active range of motion (patient-initiated movement) out of proportion to passive range of motion (examiner moves limb—less limited as muscle activation not required), pain with resisted testing of specific muscle groups, and strength deficit quantified using manual muscle testing graded 0-5 (0=no contraction, 1=flicker, 2=movement with gravity eliminated, 3=movement against gravity only, 4=movement against some resistance, 5=normal strength).

| Symptom | Timing / Description |
|---|---|
| Pain at injury site | Immediate (0-6 hours) |
| Muscle spasm/cramping | Immediate (0-6 hours) |
| Reduced range of motion | Immediate (0-6 hours) |
| Decreased strength | Immediate (0-6 hours) |
| Swelling | Delayed (24-48 hours) |
| Ecchymosis (bruising) | Delayed (2-5 days) |
| Morning stiffness | Delayed (24-72 hours) |
| Functional limitations | Immediate to Chronic |
| Persistent weakness | Chronic (>6 weeks) |
| Trigger points | Chronic (>3 months) |
Soft tissue injury diagnosis relies heavily on clinical examination, with imaging serving a confirmatory role or ruling out associated bony injuries. Our systematic approach ensures accurate diagnosis and guides treatment selection.
Clinical examination begins with inspection noting ecchymosis distribution (diagonal across chest suggests seatbelt, localized suggests direct impact), swelling patterns, and visible deformities. Palpation identifies point tenderness, muscle spasm or taut bands, palpable defects or gaps suggesting complete tears, and temperature changes (warmth suggests active inflammation). Active and passive range of motion testing differentiates muscular limitation (active more limited than passive) from joint capsule restriction (both equally limited). Resisted strength testing isolates specific muscle groups: manual resistance applied while patient contracts muscle reproduces pain in injured muscle/tendon and reveals strength deficits graded 0-5.
Special tests target specific structures: for shoulder injuries, we perform empty can test (supraspinatus), drop arm test (supraspinatus tear), Hawkins-Kennedy test (impingement), and Speed's test (biceps tendon). For knee, we assess Lachman and anterior drawer (ACL), posterior drawer (PCL), varus and valgus stress (collateral ligaments), and McMurray's test (meniscus). For ankle, anterior drawer and talar tilt assess ligament integrity. Positive tests combined with mechanism and clinical presentation establish diagnosis.
Imaging selection follows clinical indication: Plain X-rays are initial imaging for any injury involving joint or bone proximity, ruling out fractures, dislocations, and foreign bodies. X-rays don't visualize soft tissue injuries directly but show secondary signs like joint effusion or soft tissue swelling. Ottawa rules guide ankle and knee X-ray necessity, reducing unnecessary imaging.
Ultrasound is excellent for superficial soft tissue evaluation including rotator cuff tears, Achilles tendon ruptures, patellar tendon tears, muscle tears with hematoma, and joint effusions. Ultrasound is real-time, allows dynamic assessment (imaging during movement), and is cost-effective. Limitations include operator dependence and limited depth penetration (not useful for deep structures like hip rotator cuff).
MRI provides definitive soft tissue imaging with superior contrast resolution, visualizing muscle tears, tendon tears (complete vs partial), ligament injuries, cartilage damage, bone marrow edema, and joint effusions. MRI is ordered when clinical examination suggests Grade 2 or 3 injury, surgical intervention is considered, or diagnosis remains unclear after examination and X-ray. For medico-legal cases, MRI provides objective documentation of injury severity.
CT scanning is reserved for complex fractures or when MRI is contraindicated (pacemaker, certain metal implants). CT arthrography (CT after intra-articular contrast injection) can evaluate cartilage and ligaments when MRI unavailable. Electrodiagnostic studies (EMG/NCS) are rarely needed for pure soft tissue injuries but can identify associated nerve injuries (brachial plexus injury with shoulder trauma, radial nerve injury with humeral fracture, peroneal nerve injury with knee dislocation).

Soft tissue injury treatment progresses through phases targeting inflammation reduction, pain control, tissue healing, and functional restoration. Our evidence-based protocols optimize recovery while preventing chronic dysfunction.
Phase 1 (Acute: Days 1-7) implements RICE protocol: Rest means activity modification avoiding pain-provoking movements, not complete immobilization which delays recovery. "Relative rest" maintains general activity while protecting injured tissue. Ice application (15-20 minutes every 2-3 hours) for first 48-72 hours reduces inflammation and pain through vasoconstriction and decreased metabolic rate. Compression with elastic bandages reduces swelling by preventing fluid accumulation—avoid excessive tightness compromising circulation. Elevation above heart level uses gravity to facilitate venous and lymphatic drainage.
Medication includes NSAIDs (ibuprofen 800mg TID or naproxen 500mg BID) for anti-inflammatory effect, though some evidence suggests NSAIDs may slightly impair early tendon healing—balance symptom relief against theoretical healing concerns. Acetaminophen provides analgesia without anti-inflammatory effect. Muscle relaxants (cyclobenzaprine, tizanidine) address secondary muscle spasm. Immobilization is used judiciously: slings for shoulder injuries during first 1-2 weeks, walking boots for ankle injuries, knee braces for ligament sprains—but prolonged immobilization (>2 weeks) causes muscle atrophy and joint stiffness, delaying recovery.
Phase 2 (Subacute: Weeks 1-6) introduces progressive rehabilitation. Physical therapy begins with gentle range of motion exercises, progressing from passive (therapist moves limb) to active-assisted (patient initiates movement with assistance) to active (patient performs independently). Early controlled motion prevents adhesions and maintains joint nutrition. Strengthening starts with isometric exercises (muscle contraction without joint movement), progressing to isotonic (movement through range with constant resistance) and finally isokinetic (movement at constant speed with variable resistance). Progressive resistance training rebuilds strength: initial loads at 50% of injured side strength, gradually increasing as tolerated. The contralateral limb often trains at higher resistance to maintain fitness and provide neuromuscular input via cross-education effect.
Manual therapy including soft tissue mobilization (massage techniques targeting specific tissues), myofascial release (sustained pressure releasing fascial restrictions), and trigger point therapy addresses secondary myofascial dysfunction. Therapeutic modalities include ultrasound therapy (high-frequency sound waves producing deep tissue heating, promoting blood flow and collagen extensibility), electrical stimulation (TENS for pain modulation, NMES for muscle re-education and preventing atrophy), and iontophoresis (using electrical current to drive anti-inflammatory medication transdermally).
Phase 3 (Intermediate: Weeks 6-12) emphasizes functional restoration. Sport/work-specific training incorporates movements and demands of patient's activities: plyometric exercises for athletes (explosive movements training muscle-tendon unit to store and release elastic energy), work simulation for injured workers (lifting, carrying, reaching tasks at progressively increasing loads), and activity-specific drills. Proprioceptive training on balance boards, foam pads, or single-leg stance improves neuromuscular control, reducing re-injury risk by up to 50% in ankle sprains.
Injection therapies for refractory cases include corticosteroid injections for inflamed tendons (though limited evidence for efficacy and concerns about tendon weakening—used selectively), PRP (platelet-rich plasma) showing promise for chronic tendinopathy and partial tendon tears by delivering growth factors promoting healing, and prolotherapy (injection of dextrose or other proliferants) theoretically stimulating healing response though evidence is mixed.
Phase 4 (Surgical: Rarely Needed) is reserved for complete ruptures of critical structures: rotator cuff complete tears in active patients (arthroscopic repair), Achilles tendon ruptures (open or percutaneous repair—surgery reduces re-rupture rates from 15% to <5% compared to conservative care), patellar tendon ruptures (primary surgical repair required for restoration of extensor mechanism), and severe ligament injuries like combined ACL/MCL tears. Post-surgical rehabilitation follows similar progressive loading principles but with timeline modifications protecting surgical repair during early healing (6-12 weeks protected motion, 3-6 months return to full activity).


Acute Phase (Days 1-7)
1-7 daysRICE protocol - Rest (relative), Ice (first 48-72h), Compression, Elevation. NSAIDs, activity modification. Brief immobilization if needed (1-2 weeks max).
Subacute Phase (Weeks 1-6)
1-6 weeksProgressive rehabilitation - range of motion (passive→active), progressive strengthening (isometric→isotonic→isokinetic), manual therapy, therapeutic modalities.
Intermediate Phase (Weeks 6-12)
6-12 weeksFunctional restoration - sport/work-specific training, plyometrics, proprioceptive training, PRP or injections if refractory. Return to activity progression.
Surgical Phase (If Needed)
Case dependentComplete ruptures of critical structures - rotator cuff, Achilles, patellar tendon, severe ligament tears. Followed by 3-6 month rehabilitation.
Soft tissue injury recovery varies by grade, location, and patient factors. Understanding expected timelines manages expectations and guides return-to-activity decisions.
Grade 1 (mild) strains typically resolve in 2-4 weeks with conservative care. Most patients achieve full pain-free function and return to pre-injury activities without restrictions by 3-4 weeks. Athletes can often continue training with modifications during recovery.
Grade 2 (moderate) strains require 6-12 weeks for substantial recovery. Pain decreases progressively but may persist at low levels for 2-3 months. Return to light duty work occurs at 4-6 weeks; return to heavy labor or competitive athletics at 8-12 weeks. Comprehensive rehabilitation is essential—inadequately rehabilitated Grade 2 injuries frequently progress to chronic tendinopathy or recurrent strains.
Grade 3 (severe/complete) tears demand 3-6 months for recovery, often including surgery. Post-surgical timelines vary by location: Achilles tendon repair allows weight-bearing in walking boot at 6-8 weeks, return to jogging at 4 months, return to sports at 6-9 months. Rotator cuff repair follows similar timeline: passive motion only for 6 weeks (protecting repair), active motion 6-12 weeks, strengthening 12+ weeks, return to overhead sports at 6-9 months. Surgical success rates are excellent when performed acutely but decline with delay—chronic tears develop muscle atrophy and fatty infiltration decreasing repair success and functional outcomes.
Contusions (bruises) without hematoma resolve in 2-4 weeks. Large intramuscular hematomas require 6-12 weeks, occasionally longer if myositis ossificans develops (heterotopic bone formation in 9-20% of large contusions, particularly in quadriceps). Myositis ossificans appears as firm mass palpable within muscle 3-6 weeks post-injury; X-rays show calcification. Treatment is conservative (NSAIDs, gentle stretching, avoid aggressive massage which may worsen) with gradual resolution over 6-12 months. Surgical excision is rarely needed for symptomatic cases after maturation.
Factors affecting recovery include age (younger patients heal faster), injury severity (higher grade = longer recovery), location (well-vascularized muscles heal faster than tendons and ligaments with limited blood supply), prior injuries (previously injured tissues more prone to recurrence), and rehabilitation compliance (consistent therapy adherence improves outcomes significantly). Smoking impairs healing through vasoconstriction and should be strongly discouraged.
Return-to-work criteria include pain-free or near-pain-free daily activities, strength ≥80% of contralateral side for light duty, ≥90% for moderate duty, ≥95% for heavy labor, ability to perform essential job functions without exacerbating injury, and clearance by treating physician. Functional capacity evaluations objectively document capabilities supporting return-to-work decisions.
Return-to-sport criteria are more stringent: full pain-free range of motion, strength ≥90% of contralateral side (>95% preferred), sports-specific functional testing passed (agility drills, jumping, cutting), and athlete psychologically ready. Premature return risks recurrent injury, often more severe than initial injury.
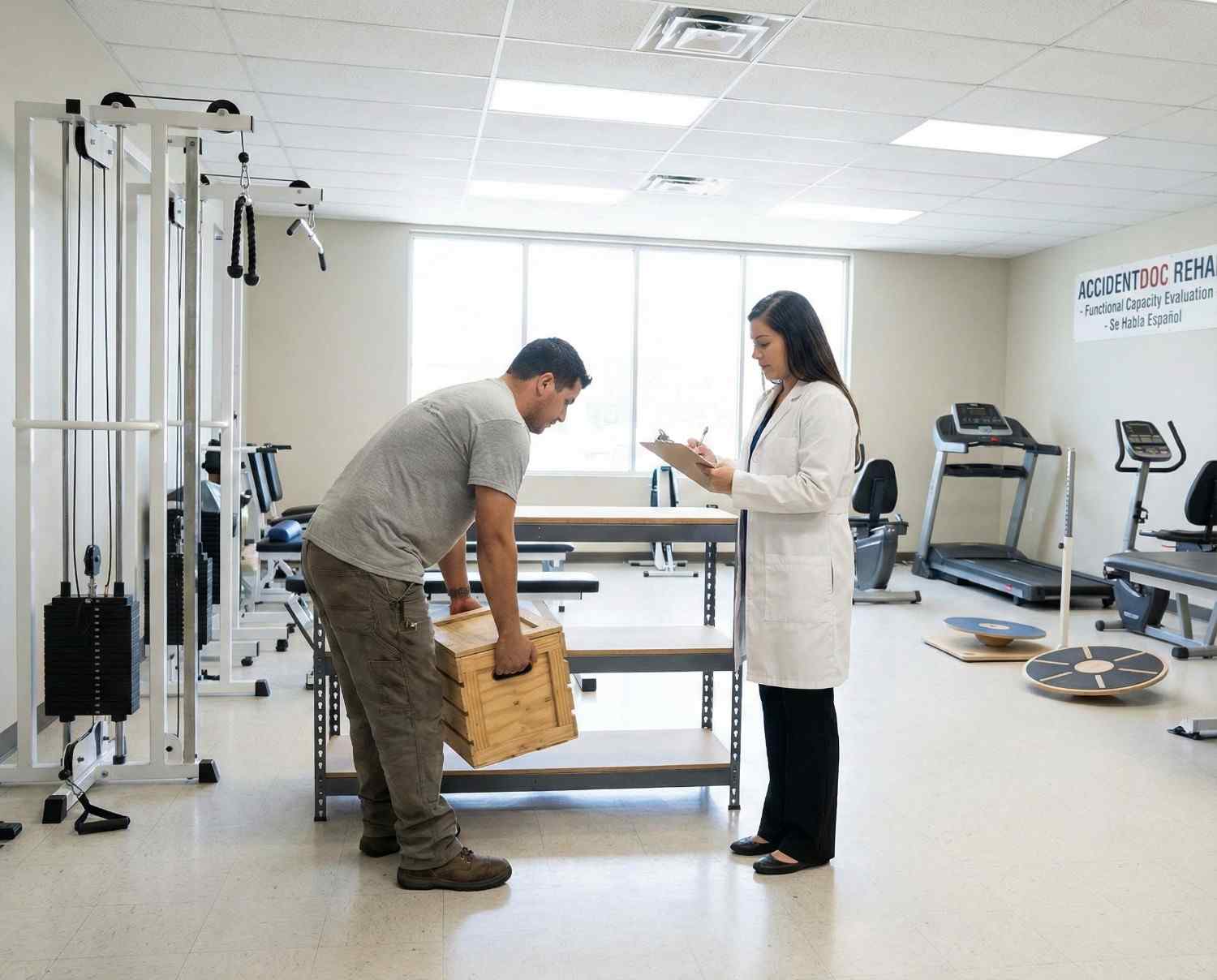
Soft tissue injuries present unique documentation challenges as they often lack dramatic imaging findings despite substantial pain and functional impairment. Thorough clinical documentation is essential for insurance claims and legal cases.
Mechanism documentation establishes causation: "Patient sustained Grade 2 pectoralis major strain when seatbelt loaded chest wall during sudden deceleration in rear-end collision on [DATE]. Physical examination reveals diagonal ecchymosis pattern across right chest consistent with seatbelt mechanism, palpable tenderness over pectoralis insertion, pain with resisted shoulder horizontal adduction, and 4/5 strength compared to 5/5 left side. Mechanism is consistent with and sufficient to cause observed injury."
Physical examination findings must be specific and quantified: "Right pectoralis major demonstrates 15×8 cm ecchymosis from clavicle to mid-chest. Point tenderness to palpation over sternal insertion. Palpable taut band in muscle belly. Active range of motion: shoulder flexion 110° (normal 180°), abduction 90° (normal 180°), internal rotation 45° (normal 70°). Strength testing: flexion 4+/5, abduction 4+/5, horizontal adduction 4/5 (pain-limited, normal 5/5 left). Negative impingement signs. Diagnosis: Grade 2 pectoralis major strain."
Imaging correlation: "Ultrasound right pectoralis major on [DATE] reveals hypoechoic region measuring 3.2×1.8 cm within mid muscle belly with increased vascularity on Doppler, consistent with Grade 2 intramuscular tear with associated hematoma. No complete fiber disruption. These findings correlate with clinical presentation."
Functional limitations documentation supports disability and damages claims: "Patient unable to perform essential job functions as automotive technician due to pectoralis strain. Job requires frequent overhead reaching, pushing/pulling of 25-50 lbs, and use of pneumatic tools creating vibration and resistance. Current restrictions: no lifting >15 lbs, no overhead work, no pushing/pulling >20 lbs. Patient cannot perform oil changes (overhead arm positioning), tire changes (torque wrench use), or brake work (sustained forceful pushing). Recommend light duty assignment if available; otherwise off work. Expected duration of restrictions: 8-12 weeks with comprehensive rehabilitation."
Causation opinion: "Within reasonable medical probability, patient's right pectoralis major strain is directly and proximately caused by the motor vehicle collision of [DATE]. The injury mechanism (seatbelt restraint causing eccentric loading during sudden deceleration) is consistent with the injury. The temporal relationship (symptoms developing immediately post-accident) supports causation. The diagonal ecchymosis pattern is pathognomonic for seatbelt loading. Patient had no prior history of pectoralis injury and was asymptomatic prior to accident."
Prognosis and future medical needs: "Patient prognosis is good for substantial recovery with appropriate rehabilitation. Expected timeline: 50% improvement by 4-6 weeks, 80% improvement by 8-10 weeks, maximum medical improvement at 3-4 months. Future medical needs include completion of physical therapy (estimated 12-16 sessions), possible ultrasound-guided injection if plateau at 8 weeks, and 5-10% risk of chronic pain requiring ongoing intermittent treatment. Permanent partial impairment rating expected at 0-5% upper extremity impairment (converts to 0-3% whole person). No permanent restrictions anticipated for sedentary work; possible permanent restrictions for heavy overhead labor."
- Detailed mechanism documentation with injury causation correlation
- Specific physical examination findings with measurements and functional testing
- Imaging correlation when available (ultrasound, MRI)
- Functional limitations and work restrictions with job-specific analysis
- Causation opinion stated within reasonable medical probability
- Treatment plan with medical necessity justification
- Prognosis with expected recovery timeline
- Future medical needs and estimated costs
- Disability ratings at maximum medical improvement if permanent impairment
While most soft tissue injuries are managed conservatively, certain presentations indicate serious complications requiring emergency evaluation.
Compartment syndrome occurs when pressure within a fascial compartment (containing muscles, nerves, vessels) exceeds perfusion pressure, causing ischemia and potential permanent damage. It develops after severe contusions, crush injuries, or fractures. Classic presentation is "6 P's": Pain out of proportion to injury and worsening despite treatment, Pressure (tense, swollen compartment), Paresthesias (numbness/tingling), Pallor (pale skin), Pulselessness (late finding—irreversible damage likely occurred), Paralysis (late finding). Pain with passive stretching of muscles in affected compartment is the most sensitive early sign. Compartment syndrome is a surgical emergency requiring immediate fasciotomy (incising fascia to release pressure). Any patient with severe contusion and worsening pain, especially if pain with passive stretching develops, requires immediate emergency evaluation with compartment pressure measurement.
Vascular injury with diminished or absent pulses, pale or cool extremity, or expanding hematoma suggests arterial injury requiring immediate vascular surgery consultation. Nerve injury with severe neurological deficits (complete motor/sensory loss) may require surgical exploration and repair. Open wounds with exposed tendon or muscle require emergent irrigation and repair—contamination risk demands antibiotic prophylaxis and tetanus update.
Signs of infection including fever, spreading erythema, warmth, purulent drainage, or red streaking (lymphangitis) warrant immediate evaluation as soft tissue infections can progress rapidly to necrotizing fasciitis, a life-threatening emergency. Patients with large ecchymosis should be monitored for signs of rhabdomyolysis including dark urine (myoglobinuria), decreased urine output, and systemic symptoms—severe cases require hospitalization for IV hydration preventing acute kidney injury.
- Compartment syndrome - Pain out of proportion, tense swelling, pain with passive stretch
- Paresthesias or paralysis developing after injury
- Pulselessness, pallor, or cool extremity (vascular injury)
- Expanding hematoma or uncontrolled bleeding
- Open wound with exposed tendon or muscle
- Fever with spreading redness or purulent drainage (infection)
- Dark urine after severe muscle injury (rhabdomyolysis)
- Chest/abdominal pain after seatbelt injury (internal organ injury)
- Severe pain unrelieved by any intervention
While accidents are often unpredictable, strategies reduce soft tissue injury severity and promote recovery. Proper seatbelt positioning (shoulder belt across clavicle and chest, lap belt across pelvis) distributes forces optimally. Strengthening programs particularly for workers in physical occupations build resilience: rotator cuff strengthening for overhead workers, core and lower extremity strengthening for material handlers. Proper warm-up before physical activity increases muscle temperature and flexibility, reducing strain risk. Post-injury, gradual return to activity following rehabilitation prevents recurrence—studies show inadequately rehabilitated injuries recur at rates exceeding 50%. Maintaining healthy body weight, smoking cessation, and adequate protein intake (0.8-1.0 g/kg bodyweight, higher during healing) support tissue health and repair. Ergonomic modifications and assistive devices reduce workplace injury risk.
Seek Emergency Care Immediately If You Experience:
- Compartment syndrome - severe pain, tense swelling, pain with passive muscle stretching
- Paresthesias (numbness/tingling) or paralysis developing after injury
- Diminished or absent pulses, pale or cool extremity (vascular injury)
- Expanding hematoma or uncontrolled bleeding
- Open wound with exposed muscle, tendon, or bone
- Fever, spreading redness, purulent drainage (infection)
- Dark or tea-colored urine after crush injury (rhabdomyolysis)
- Chest or abdominal pain after seatbelt injury (internal organs)
- Severe unrelenting pain despite medication and ice
Call 911 or go to the nearest emergency room immediately
Concussions & Head Injuries

Traumatic brain injuries (TBI), including concussions, affect over 2.8 million Americans annually, with motor vehicle accidents representing the leading cause among adults. Concussions are complex neurometabolic injuries affecting brain function without necessarily showing structural damage on standard imaging. At AccidentDoc Pasadena, our board-certified physicians specialize in comprehensive concussion evaluation and evidence-based treatment protocols, from acute management through post-concussion syndrome recovery. Early diagnosis and proper treatment prevent long-term cognitive impairment and accelerate return to normal function.
A concussion is a mild traumatic brain injury (mTBI) resulting from biomechanical forces transmitted to the brain, causing a complex neurometabolic cascade without necessarily producing structural injury visible on CT or standard MRI. Understanding the injury mechanism is critical for recognizing concussions that might otherwise go undiagnosed and untreated.
The brain consists of approximately 86 billion neurons suspended in cerebrospinal fluid within the rigid skull. During sudden acceleration-deceleration or rotational forces—common in car accidents—the brain moves within the skull despite CSF cushioning, creating strain on neural tissue, blood vessels, and axonal connections. This movement occurs in two phases: the coup injury where the brain impacts the skull at the point of force application, and the contrecoup injury where the brain rebounds and impacts the opposite skull surface. Rotational acceleration, where the head twists suddenly, creates the most severe shearing forces on axons, particularly at gray-white matter junctions where tissue density differences create maximal strain.
At the cellular level, concussion triggers a neurometabolic cascade: mechanically-stressed neurons release excessive excitatory neurotransmitters, particularly glutamate, causing ionic flux (potassium efflux, calcium influx). This ionic imbalance forces energy-dependent sodium-potassium pumps to work overtime, depleting ATP (adenosine triphosphate) stores when mitochondrial function is simultaneously impaired by calcium overload. The result is an energy crisis where neurons require increased glucose while cerebral blood flow is paradoxically reduced, creating a mismatch between supply and demand. This metabolic dysfunction typically lasts 7-10 days in uncomplicated concussions but can persist weeks to months in severe cases or repeat injuries.
Axonal injury occurs through mechanical shearing and secondary metabolic dysfunction: the disruption of microtubules and neurofilaments impairs axonal transport, causing accumulation of proteins and eventual axonal disconnection. Diffuse axonal injury (DAI) represents the severe end of this spectrum and can occur even without loss of consciousness. Research using advanced neuroimaging including diffusion tensor imaging (DTI) demonstrates that structural axonal injury exists in many "mild" concussions, explaining persistent symptoms despite normal CT scans.
The brain regions most vulnerable to concussion injury include the prefrontal cortex (executive function, impulse control), temporal lobes (memory formation), corpus callosum (interhemispheric communication), and brainstem centers regulating autonomic function. This explains the constellation of cognitive, emotional, and autonomic symptoms characterizing concussion. The developing adolescent brain is particularly vulnerable due to ongoing myelination and synaptic pruning, while elderly brains with age-related atrophy have more space for brain movement within the skull, paradoxically increasing injury risk.
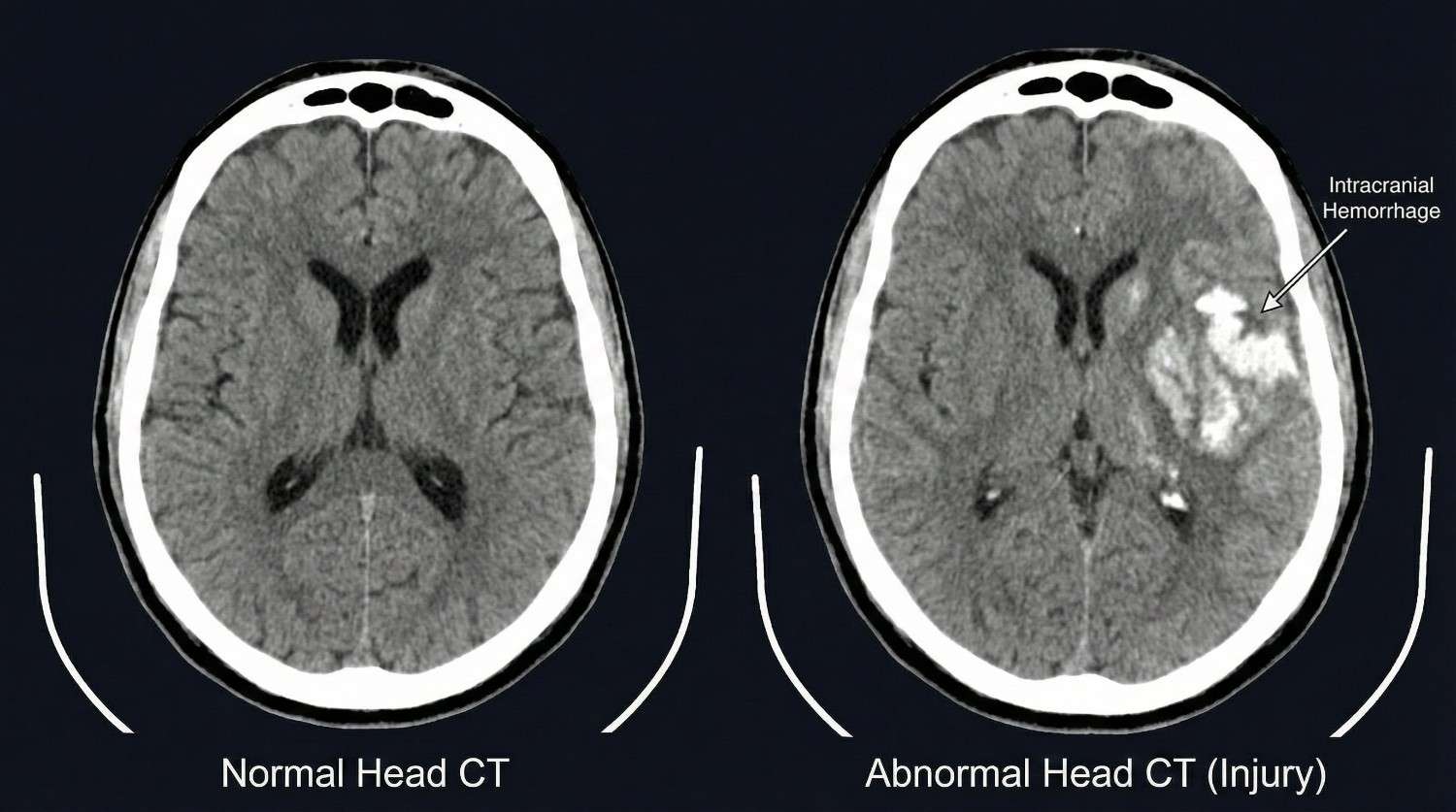
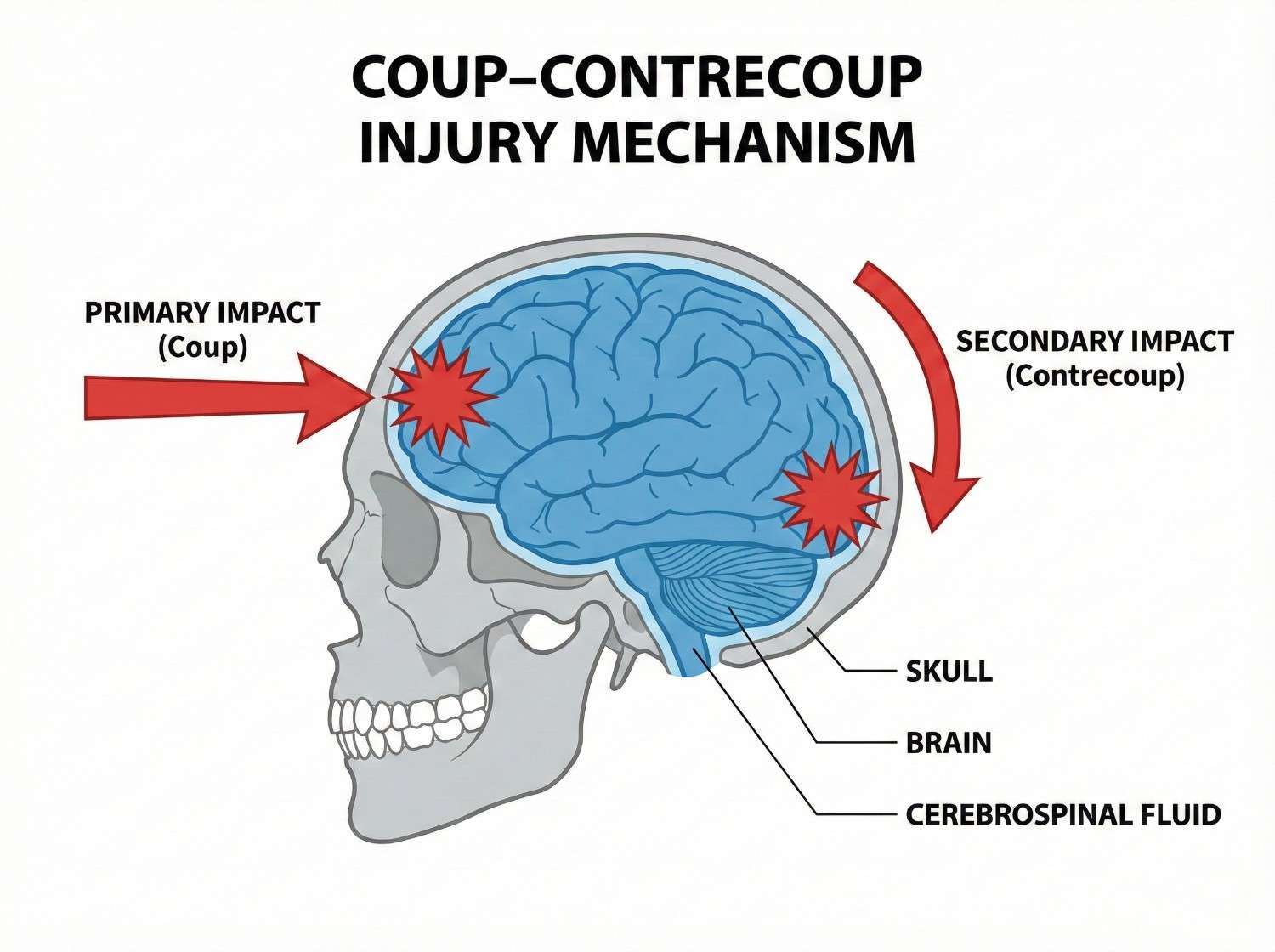
Motor vehicle accidents are the leading cause of traumatic brain injury among adults aged 20-60, accounting for approximately 50% of TBI-related emergency department visits in this demographic. Rear-end collisions produce rapid head acceleration-deceleration: the torso accelerates forward with the seat while the head initially lags (inertia), then snaps forward as neck muscles contract and anterior structures limit extension. This whiplash-type mechanism can cause concussion even without direct head impact, as the brain moves within the skull. Frontal collisions create the reverse mechanism, with airbag deployment sometimes contributing additional impact force to the head, particularly if the occupant is unrestrained or improperly positioned.
Side-impact collisions generate rotational acceleration, the most damaging force for brain tissue. The head rotates suddenly as it's struck by the window, B-pillar, or intruding vehicle structure, creating maximal shearing strain on axons at gray-white matter junctions. Side impacts produce higher concussion rates than frontal or rear collisions of equivalent severity due to these rotational forces. Rollover accidents combine all force vectors—linear, rotational, and vertical—often with multiple impacts as the vehicle rotates, producing severe TBI including both concussion and more serious intracranial hemorrhage.
Pedestrian-vehicle collisions create unique injury patterns: the initial vehicle impact, fall to ground surface (often striking the head on pavement), and sometimes secondary impact from being run over by the vehicle. The unrestrained pedestrian experiences full-body acceleration without protection, frequently resulting in moderate to severe TBI. In the Pasadena and Houston area, pedestrian accidents along high-traffic corridors like Highway 225, Fairmont Parkway, and Red Bluff Road represent significant sources of severe head trauma.
Slip-and-fall accidents, particularly common in retail, restaurant, and workplace settings, cause head injury when the victim strikes their head during the fall or when the head impacts the ground. Falls onto hard surfaces like concrete, tile, or metal grating create high-impact forces despite relatively low falling heights—a fall from standing height can generate 500+ Gs of deceleration when the head strikes concrete. Elderly patients with osteoporosis, balance disorders, or anticoagulation are particularly vulnerable to severe TBI from falls, with subdural hematomas common even from seemingly minor impacts.
Workplace accidents in Pasadena's industrial sector include being struck by falling objects (pipes, tools, equipment), scaffolding collapses, falls from height in construction and refinery work, and blast injuries in petrochemical facilities. Hard hat use reduces but doesn't eliminate concussion risk—the helmet prevents skull fractures but doesn't fully eliminate the internal brain movement causing concussion. Confined space accidents with oxygen deprivation can cause global hypoxic brain injury combined with traumatic injury if the worker collapses and strikes their head.
Assault-related head injuries from physical altercations include direct blows to the head and injuries sustained during falls after being struck. Sports and recreation injuries, while less common in our accident-focused practice, do occur and include cycling accidents without proper helmet use, ATV rollovers, and boating accidents.
- Rear-end collisions - acceleration-deceleration without direct impact (coup-contrecoup)
- Frontal collisions with airbag deployment - combined mechanism
- Side-impact collisions - rotational forces (most dangerous mechanism)
- Rollover accidents - multiple impacts, all force vectors
- Pedestrian-vehicle collisions - multiple injury phases
- Slip-and-fall - head impact on hard surfaces
- Workplace struck-by injuries - falling objects, scaffolding collapses
- Falls from height - construction, ladder, refinery work
- Assault - direct blows and fall-related head impact
Concussion symptoms are organized into four clusters—physical, cognitive, emotional, and sleep-related—with temporal patterns critical for diagnosis and management. Understanding the full symptom spectrum is essential because concussions often lack visible external injury, and patients may not immediately recognize they've sustained a brain injury.
Immediate physical symptoms (0-24 hours) include headache (present in 85-90% of concussions), often described as pressure-like or throbbing, typically generalized or frontal. Dizziness or vertigo occurs in 50-70% of patients, reflecting vestibular system dysfunction or cervical proprioceptor injury. Visual disturbances include blurred vision, difficulty focusing, sensitivity to light (photophobia), and diplopia (double vision). Nausea or vomiting results from brainstem autonomic dysfunction or vestibular disruption. Balance problems and unsteady gait are common, detectable on objective testing like tandem stance or Balance Error Scoring System (BESS). Sensitivity to noise (phonophobia) reflects auditory processing dysfunction. Immediate loss of consciousness (LOC) occurs in only 10-15% of concussions—its absence doesn't rule out concussion.
Immediate cognitive symptoms include confusion or feeling "in a fog," disorientation to time, place, or situation, amnesia for the event (retrograde amnesia) or period after the event (anterograde amnesia), slowed reaction time, and difficulty concentrating. Patients may ask repetitive questions, showing impaired short-term memory formation. Confusion severity doesn't correlate perfectly with injury severity—brief LOC with rapid return to normal orientation may indicate less severe injury than prolonged confusion without LOC.
Delayed symptoms (24 hours to 2 weeks) often exceed initial symptoms as the metabolic crisis persists and patients return to cognitive demands. Headaches may worsen or change character, sometimes evolving into post-traumatic migraine with throbbing pain, photophobia, and phonophobia. Cognitive difficulties become more apparent: impaired concentration and attention particularly noticeable when returning to work, short-term memory problems affecting daily activities, mental fogginess described as "wading through water," slowed processing speed making tasks take longer, and executive function deficits affecting planning, organization, and multitasking. These cognitive symptoms worsen with mental exertion, a phenomenon called cognitive fatigue unique to concussion.
Emotional symptoms emerge as patients struggle with functional limitations: irritability and mood changes, anxiety particularly about cognitive deficits, depression from loss of function and quality of life, emotional lability with inappropriate crying or emotional reactions, and personality changes noticed by family members before patients recognize them. These aren't simply psychological reactions to injury—they reflect actual neurophysiological changes in frontal lobe and limbic system function.
Sleep disturbances are nearly universal: initial hypersomnia (excessive sleeping) in the first week as the brain attempts recovery, followed by insomnia with difficulty falling or staying asleep, disrupted sleep architecture with reduced REM sleep, and daytime fatigue despite adequate sleep hours. Sleep disturbance both results from and worsens concussion recovery, creating a challenging cycle.
Post-concussion syndrome (PCS) develops when symptoms persist beyond expected recovery (>4 weeks in adults, >4-6 weeks in adolescents). PCS affects 10-15% of concussion patients, with risk factors including previous concussions, female gender, younger age, high initial symptom burden, early return to activity, and psychiatric history. PCS symptoms mirror acute concussion but with greater functional impairment and treatment resistance. Some patients develop chronic PCS lasting months to years, requiring comprehensive multidisciplinary treatment.
Symptom exacerbation with activity is a key diagnostic feature: physical exertion, cognitive effort (screen time, reading, problem-solving), and sensory stimulation (bright lights, loud environments) all provoke symptom worsening, distinguishing concussion from other headache disorders or psychological conditions. This symptom provocation guides return-to-activity protocols.
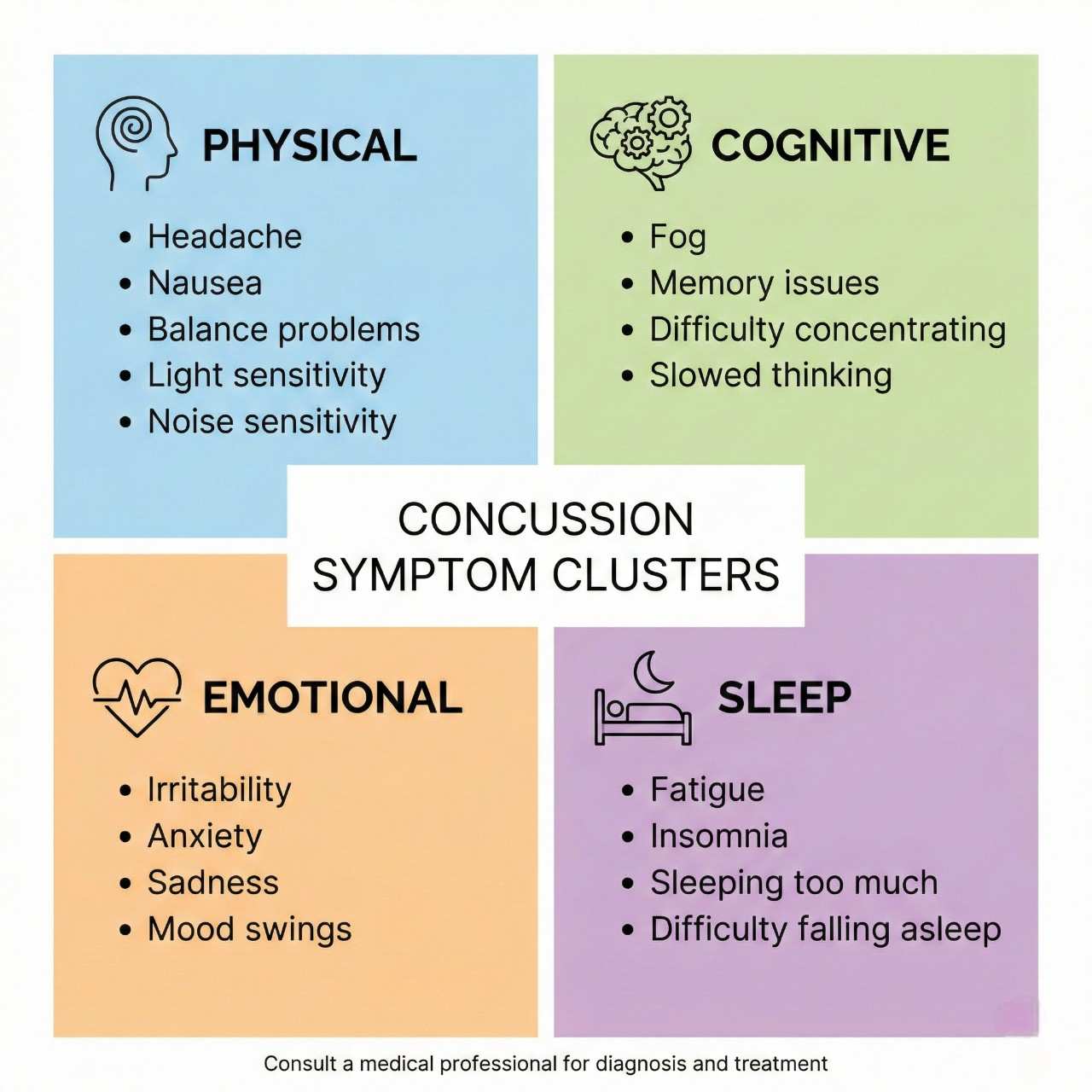
| Symptom | Timing / Description |
|---|---|
| Headache | Immediate (0-24 hours) |
| Dizziness or vertigo | Immediate (0-24 hours) |
| Visual disturbances | Immediate (0-24 hours) |
| Nausea or vomiting | Immediate (0-24 hours) |
| Balance problems | Immediate (0-24 hours) |
| Confusion or "fogginess" | Immediate (0-24 hours) |
| Amnesia | Immediate (0-24 hours) |
| Cognitive difficulties | Delayed (24hrs-2 weeks) |
| Emotional changes | Delayed (24hrs-2 weeks) |
| Sleep disturbances | Immediate to Chronic |
| Post-concussion syndrome | Chronic (>4 weeks) |
| Cognitive fatigue | Delayed to Chronic |
Concussion diagnosis is primarily clinical, based on mechanism of injury, symptom presentation, and structured examination, as standard imaging often appears normal in concussion despite significant functional impairment. Our comprehensive diagnostic approach identifies all injury components and guides treatment selection.
Initial evaluation documents injury mechanism in detail: type of accident, direction and estimated magnitude of forces, whether the head struck an object (direct impact) or the brain moved within the skull without contact (indirect mechanism), immediate symptoms including any LOC duration, and witness observations. This narrative establishes causation for legal documentation.
Structured symptom assessment uses validated tools including the Sport Concussion Assessment Tool 5th Edition (SCAT5) for adults and Child SCAT5 for patients under 13. The SCAT5 documents 22 symptoms across physical, cognitive, emotional, and sleep domains, each scored 0-6 for severity. This quantification allows objective tracking of recovery. Baseline testing, when available from pre-injury evaluations, provides invaluable comparison, though most accident victims lack pre-injury data.
Physical examination assesses multiple domains: Neurological examination includes cranial nerve testing (visual fields, pupillary reflexes, extraocular movements, facial symmetry, hearing, palatal elevation, tongue movement), motor function with strength testing of all major muscle groups, sensory examination for deficits, deep tendon reflexes comparing symmetry, and cerebellar testing (finger-to-nose, heel-to-shin, rapid alternating movements). Abnormalities suggest more severe TBI or structural injury.
Vestibular and balance testing objectively quantifies common concussion deficits: Balance Error Scoring System (BESS) tests three stances (double leg, single leg, tandem) on firm and foam surfaces with eyes closed, counting errors over 20 seconds. Concussed patients show significantly more errors than healthy controls. Vestibular ocular motor screening (VOMS) assesses smooth pursuits, saccades, convergence, and vestibular-ocular reflex (VOR), with symptoms provoked by these maneuvers indicating vestibular dysfunction. Dix-Hallpike maneuver tests for benign paroxysmal positional vertigo (BPPV), common after head trauma.
Cognitive screening uses validated tools: Montreal Cognitive Assessment (MoCA) screens for deficits in attention, executive function, memory, language, and visuospatial skills. Scores <26/30 indicate impairment. Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) is a computerized battery measuring verbal and visual memory, processing speed, and reaction time. While baseline testing is ideal, normative data allows interpretation of post-injury scores. Deficits correlate with symptom severity and predict recovery duration.
Cervical spine examination is critical as whiplash commonly accompanies concussion: cervical range of motion measurement, palpation for vertebral and facet tenderness, upper extremity neurological examination, and Spurling's test for radiculopathy. Cervicogenic headache from concurrent neck injury can complicate concussion management.
Imaging selection follows evidence-based indications: Head CT without contrast is the initial study for moderate to severe TBI or when intracranial hemorrhage is suspected. Indications include Glasgow Coma Scale (GCS) <15, focal neurological deficits, severe persistent headache, repeated vomiting (>2 episodes), seizure, amnesia >30 minutes, dangerous mechanism (high-speed collision, fall >3 feet, pedestrian struck), age >65, or anticoagulation use. CT identifies skull fractures, epidural hematomas, subdural hematomas, subarachnoid hemorrhage, intracerebral hemorrhage, and cerebral contusions requiring neurosurgical consultation. However, CT is often normal in concussion, as the injury is primarily metabolic and functional rather than structural.
MRI brain is more sensitive for subtle structural injury but rarely changes acute management. We order MRI for persistent symptoms beyond 4-6 weeks, atypical symptom progression, focal neurological deficits with negative CT, or suspicion of diffuse axonal injury. Susceptibility-weighted imaging (SWI) and diffusion tensor imaging (DTI) detect microhemorrhages and axonal injury not visible on standard MRI sequences, though these advanced techniques are primarily research tools currently.
Cervical spine imaging (X-rays or MRI) is obtained when neck pain persists or radicular symptoms develop, as concurrent cervical injury affects treatment planning. Neuropsychological testing provides comprehensive cognitive assessment when ImPACT or MoCA suggest deficits, evaluating attention, memory, executive function, processing speed, and emotional functioning. This testing guides cognitive rehabilitation and documents disability for legal proceedings.
Electroencephalography (EEG) is reserved for suspected post-traumatic seizures, not routine concussion evaluation. Blood biomarkers including S100B protein and glial fibrillary acidic protein (GFAP) show promise for concussion diagnosis but aren't yet standard clinical practice. This comprehensive evaluation ensures accurate diagnosis while identifying structural injuries requiring urgent intervention.
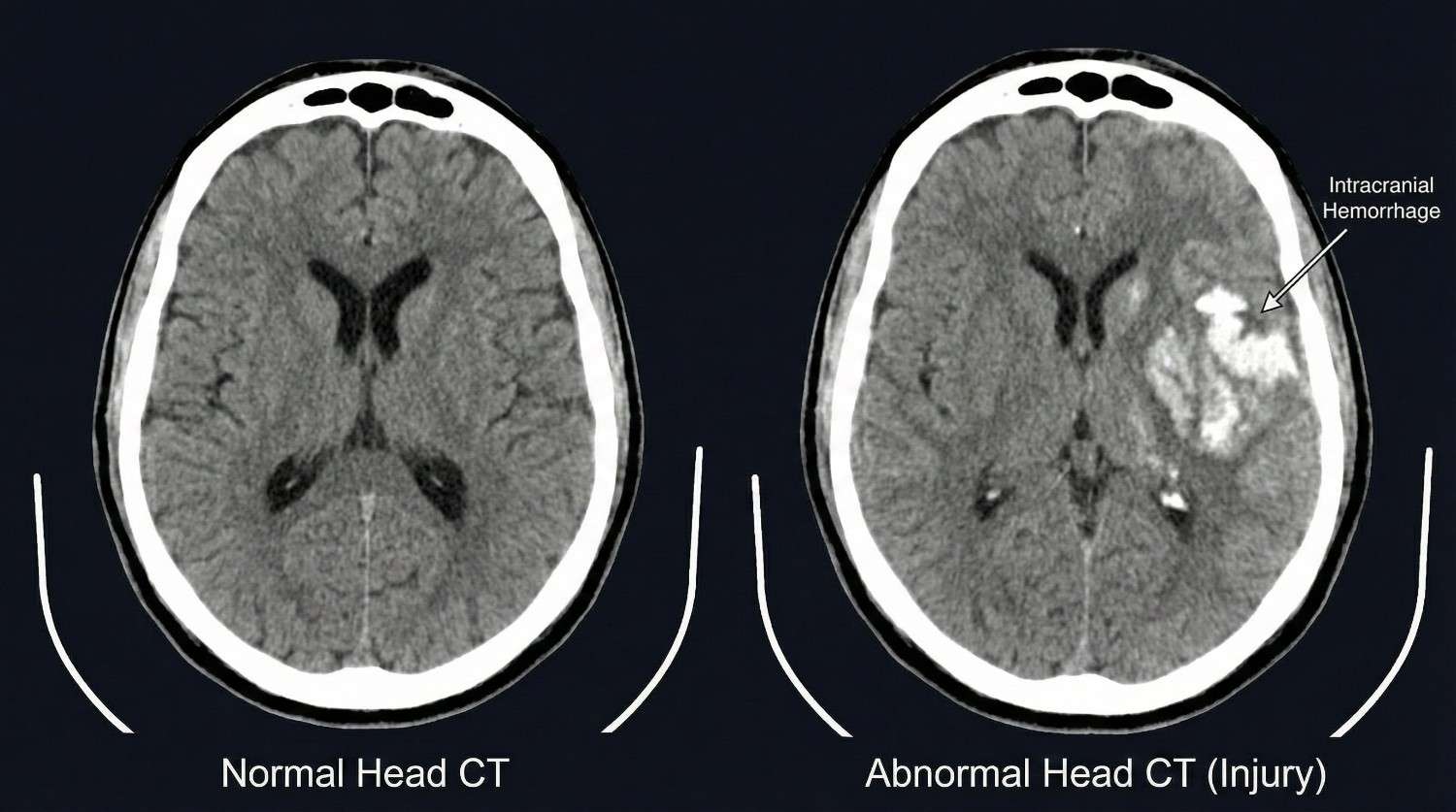

Modern concussion treatment has evolved from prolonged rest in dark rooms to active rehabilitation protocols that optimize recovery while preventing post-concussion syndrome. Our evidence-based approach progresses through phases based on symptom severity and patient response. All treatment is available through Letter of Protection with $0 upfront cost.
Phase 1 (Acute Rest Phase: Days 1-3) emphasizes brief initial rest to allow the neurometabolic crisis to stabilize, but not prolonged inactivity which delays recovery. We recommend 24-48 hours of relative cognitive and physical rest: limiting screen time (phones, computers, television) to <30 minutes at a time, avoiding reading or activities requiring sustained concentration, taking frequent breaks during necessary activities, and avoiding physically demanding activities. However, light activity is encouraged—short walks, light household tasks—as complete bedrest impairs recovery. Sleep optimization is prioritized: maintaining regular sleep schedule, creating dark quiet sleep environment, and avoiding caffeine after noon. Many patients naturally require increased sleep (12-14 hours) in the first few days; this should be allowed.
Symptom management includes analgesics for headache: acetaminophen (Tylenol) is first-line, as NSAIDs theoretically increase bleeding risk in the acute phase, though this risk is likely minimal. If headaches persist beyond 3-4 days, we prescribe migraine-specific medications including triptans (sumatriptan, rizatriptan) for severe headaches, or preventive medications for frequent headaches. Anti-nausea medications (ondansetron, promethazine) address persistent nausea. We avoid opioids and benzodiazepines due to cognitive effects that impair assessment and recovery.
Vestibular symptoms are managed with vestibular suppressants (meclizine) for acute severe vertigo, though these are limited to 2-3 days to avoid delaying central compensation. Canalith repositioning maneuvers (Epley maneuver) treat post-traumatic BPPV if Dix-Hallpike testing is positive.
Phase 2 (Graduated Return to Activity: Days 4-14) introduces progressive activity following the Berlin Consensus Statement on Concussion in Sport guidelines. The protocol includes six stages with 24-hour minimum intervals between stages, advancing only if symptoms don't worsen: Stage 1 (days 1-3): Daily activities that don't provoke symptoms, limited physical and cognitive activity. Stage 2 (days 4-5): Light aerobic exercise—walking, stationary cycling at <70% maximum heart rate for 10-15 minutes. Purpose: increase heart rate without symptom provocation. Stage 3 (days 6-8): Sport-specific exercise without contact—moderate intensity aerobic activity, beginning sport-specific drills. Stage 4 (days 9-11): Non-contact training drills with increased cognitive load—more complex drills, resistance training. Stage 5 (days 12-14): Full-contact practice—after medical clearance, participate in normal training. Stage 6 (day 15+): Return to full activity without restrictions.
This graduated protocol applies to work, school, and physical activity. Cognitive exertion is similarly graduated: initial 30-minute blocks of work or school with breaks, progressively increasing to half-days, then full days as tolerated. Importantly, patients should operate at 80-90% of symptom threshold—mild symptom provocation is acceptable and facilitates recovery, but severe symptom exacerbation requires dropping back to the previous stage.
Phase 3 (Active Rehabilitation: Weeks 2-8) addresses persistent symptoms with targeted interventions. Vestibular rehabilitation therapy is critical for balance and dizziness problems, utilizing habituation exercises (repeated exposure to symptom-provoking movements to facilitate central compensation), gaze stabilization exercises (VOR exercises improving visual stability during head movement), and balance training progressing from stable to unstable surfaces. Studies show 80% of patients with persistent vestibular symptoms improve with vestibular therapy.
Cervical spine treatment addresses concurrent whiplash using physical therapy, chiropractic manipulation, and soft tissue therapy. Cervicogenic headache responds to cervical treatments often better than traditional headache medications. Vision therapy addresses convergence insufficiency (difficulty focusing on near objects) and smooth pursuit or saccade dysfunction affecting reading. Accommodative exercises and vergence therapy improve visual function.
Cognitive rehabilitation for persistent cognitive deficits uses attention training, memory strategy development, compensatory strategy training (external memory aids, organizational systems), and graduated return to work/school with accommodations (extended test time, reduced workload, frequent breaks). Neuropsychologist-guided rehabilitation optimizes outcomes.
Exercise therapy using sub-symptom threshold aerobic exercise (Buffalo Concussion Treadmill Test protocol) demonstrates both diagnostic and therapeutic value: patients exercise to symptom exacerbation, identifying heart rate threshold, then train daily at 80% of threshold heart rate for 20 minutes. This improves autonomic dysregulation and accelerates recovery. Studies show patients using this protocol recover 1-2 weeks faster than standard rest protocols.
Phase 4 (Advanced Interventions: Weeks 8-24) treats persistent post-concussion syndrome with specialized procedures. Greater occipital nerve blocks deliver local anesthetic and corticosteroid to the occipital nerves for cervicogenic and occipital headaches, providing 4-8 weeks of relief and allowing advancement of rehabilitation. Trigger point injections address myofascial pain in cervical, suboccipital, and temporalis muscles contributing to headache. Stellate ganglion blocks show emerging evidence for treating autonomic dysfunction and cognitive symptoms in chronic PCS, modulating sympathetic nervous system dysregulation.
Pharmacological management for specific persistent symptoms includes: amitriptyline or nortriptyline (tricyclic antidepressants) for post-traumatic headache and sleep disturbance; topiramate for headache prophylaxis; methylphenidate for attention and processing speed deficits (used cautiously); selective serotonin reuptake inhibitors (SSRIs) for depression and anxiety; and melatonin for sleep cycle normalization. Medications are selected based on symptom profile and comorbidities.
Psychological support addresses emotional symptoms and teaches coping strategies: cognitive-behavioral therapy (CBT) for anxiety and depression, relaxation techniques and mindfulness training for stress management, and sleep hygiene education. The multidisciplinary approach combining physical rehabilitation, cognitive therapy, and psychological support achieves the best outcomes for complex PCS.

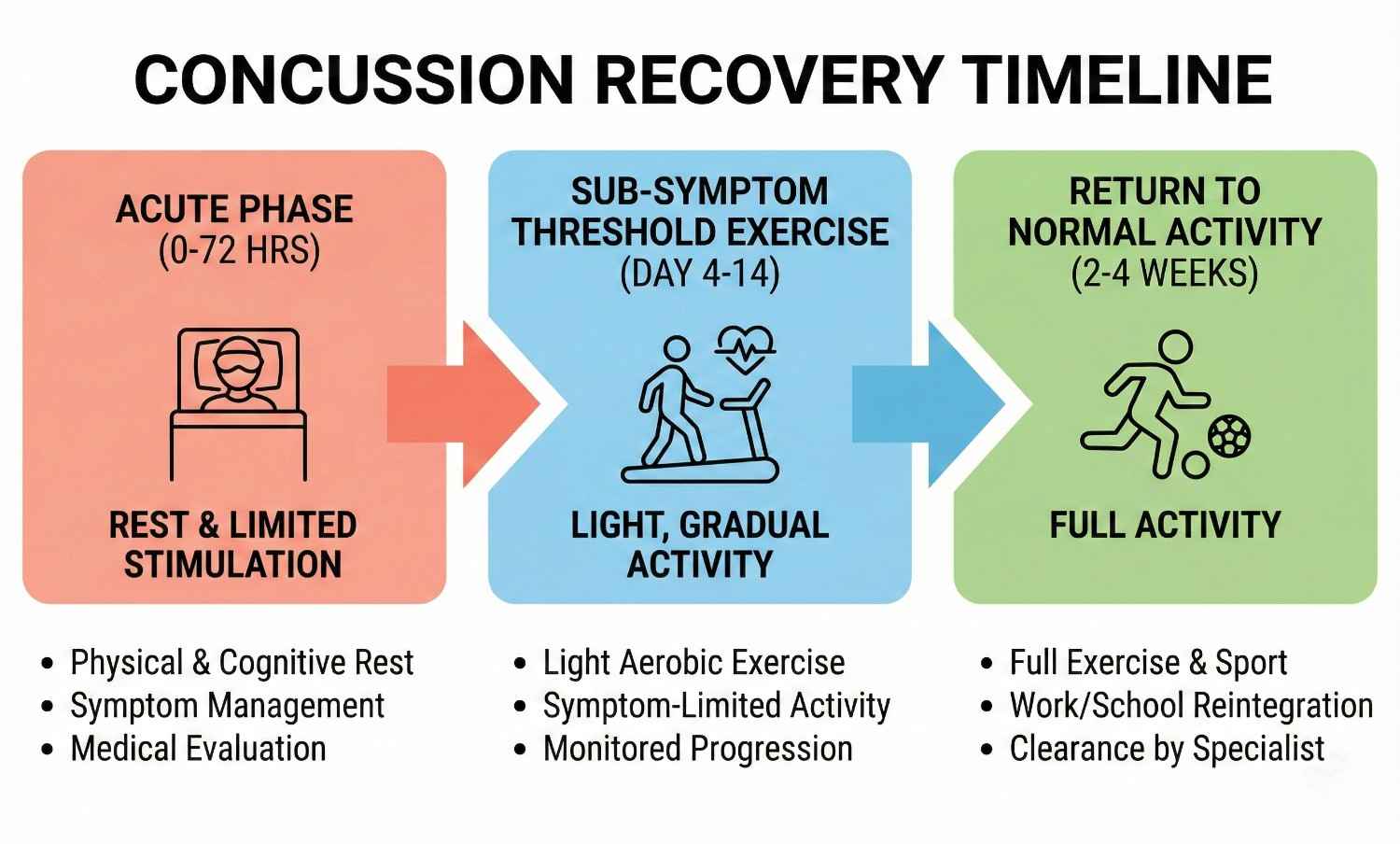
Acute Rest Phase (Days 1-3)
1-3 daysBrief relative rest (24-48 hours), limited screen time and cognitive activity, sleep optimization, symptom management with acetaminophen, anti-nausea medications. Light physical activity encouraged.
Graduated Return to Activity (Days 4-14)
4-14 daysProgressive six-stage protocol: light aerobic exercise, sport-specific drills, non-contact training, full-contact practice, return to full activity. Advance every 24 hours if asymptomatic. Cognitive activity similarly graduated.
Active Rehabilitation (Weeks 2-8)
2-8 weeksVestibular rehabilitation, cervical spine treatment, vision therapy, cognitive rehabilitation, sub-symptom threshold aerobic exercise training. Addresses persistent symptoms.
Advanced Interventions (Weeks 8-24+)
8-24+ weeksOccipital nerve blocks, trigger point injections, stellate ganglion blocks, pharmacological management, psychological support. For post-concussion syndrome and chronic symptoms.
Concussion recovery follows variable timelines influenced by injury severity, patient age, concussion history, and treatment adherence. Understanding expected recovery patterns helps patients maintain realistic expectations and clinicians identify complicated courses requiring advanced intervention.
Uncomplicated concussion in adults typically resolves within 7-14 days, with 80-90% of patients recovering fully by two weeks. Symptom progression follows a predictable pattern: physical symptoms (headache, dizziness) improve first, typically within the first week. Cognitive symptoms (concentration, memory) improve next, by days 7-14. Emotional and sleep symptoms resolve last, by weeks 2-3. This temporal pattern guides return to activity—patients can resume physical activity once physical symptoms resolve but may still require cognitive accommodations at work or school until cognitive symptoms clear.
Adolescents (ages 13-18) require longer recovery, typically 3-4 weeks, due to ongoing brain development and increased vulnerability to metabolic disruption. Children under 13 may require even longer, though they also demonstrate remarkable neuroplasticity facilitating ultimate recovery. Pediatric patients require more conservative return-to-learn and return-to-sport protocols with physician clearance.
Complicated concussion with persistent symptoms beyond 4 weeks (post-concussion syndrome) affects 10-15% of patients. Risk factors include female gender (possibly hormonal influences or reporting differences), history of prior concussions (cumulative injury effect), history of migraines (shared pathophysiology), psychiatric history including depression and anxiety, learning disabilities or ADHD (reduced cognitive reserve), and high initial symptom burden (>4 symptoms or total SCAT5 severity score >30). These patients require specialized multidisciplinary treatment combining vestibular rehabilitation, cognitive therapy, exercise training, and often pharmacological intervention. Recovery timelines extend to 3-6 months with appropriate treatment, though some patients develop chronic symptoms persisting beyond six months.
Second impact syndrome, while rare, represents a catastrophic complication where a second concussion before full recovery from the first causes rapid cerebral edema and often death or severe disability. This risk, though documented primarily in adolescents, mandates that patients be fully asymptomatic and cleared by a physician before returning to contact sports or high-risk activities. We use objective assessments (normal SCAT5 scores, normal balance testing, normal cognitive testing, normal exertional tolerance) in addition to subjective symptom resolution before clearance.
Return-to-work protocols vary by occupation: sedentary office work can typically resume at 50% capacity (half-days) once cognitive symptoms are mild, progressing to full-time over 1-2 weeks as tolerated. Jobs requiring driving, operation of heavy machinery, or work at heights require complete symptom resolution and normal reaction time testing given safety implications. Healthcare providers, pilots, and others in safety-sensitive positions may require formal fitness-for-duty evaluations before full clearance.
Return-to-drive is often overlooked but critical: reaction time impairment persists for days to weeks after concussion, increasing motor vehicle accident risk. We recommend no driving in the first 24-48 hours, then daytime low-demand driving only (short trips, familiar routes, light traffic) until symptoms fully resolve. Patients should not drive if taking sedating medications, experiencing significant cognitive slowing, or having visual disturbances.
Long-term outcomes for single concussions with appropriate treatment are generally excellent, with >95% of patients returning to pre-injury function. However, repeated concussions, particularly when occurring before complete recovery from prior injury, carry cumulative risks: chronic traumatic encephalopathy (CTE) is a progressive neurodegenerative disease associated with repetitive head impacts and concussions, presenting with cognitive decline, mood disturbance, and behavioral changes, typically not apparent until years or decades after injury exposure. While originally described in athletes and military personnel with extensive exposure, emerging evidence suggests CTE may develop with fewer impacts than previously thought. This underscores the importance of proper concussion management preventing repeat injury during the vulnerable recovery period.
Prognostic factors predicting favorable recovery include young age (excluding very young children and elderly), no prior concussions, low initial symptom burden, early presentation for treatment (within 24-48 hours), good social support, no psychiatric comorbidities, and ability to rest adequately initially. Conversely, poor prognostic factors include delayed treatment presentation (>1 week), premature return to activity with symptom exacerbation, multiple prior concussions, pre-existing psychiatric conditions, ongoing stressors (litigation, job loss, family conflict), and comorbid cervical spine injury complicating symptom attribution.
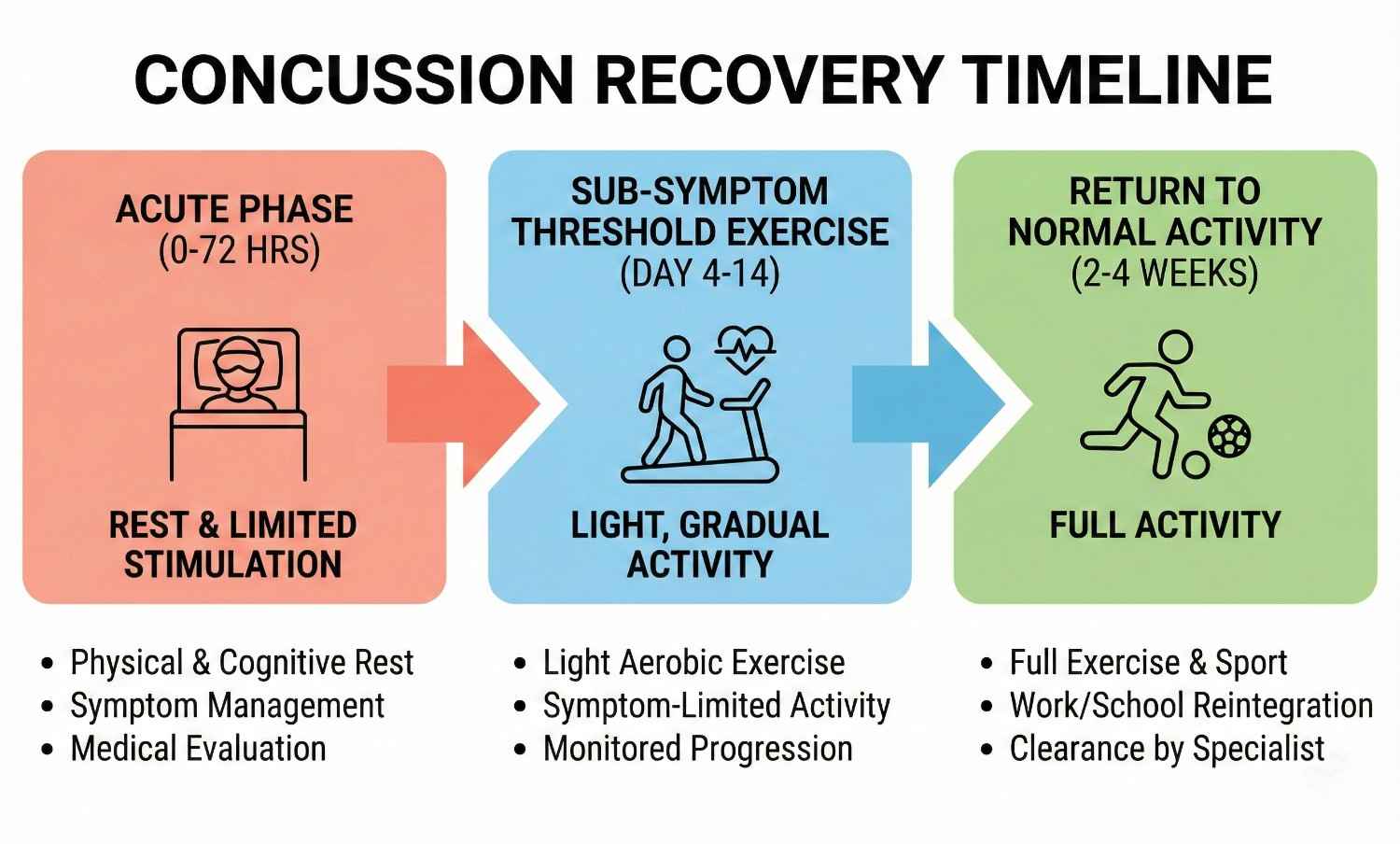
Comprehensive documentation is essential for personal injury claims involving concussion, as the injury often lacks visible external evidence and symptoms may be subjectively reported, creating challenges in proving injury and damages. AccidentDoc Pasadena provides detailed documentation specifically designed to support legal proceedings.
Injury mechanism documentation establishes causation by correlating accident biomechanics with concussion pathophysiology: "Patient sustained concussion on [DATE] when struck from behind at estimated 35 mph while stopped at traffic light on Highway 225. The sudden acceleration-deceleration created coup-contrecoup forces as the brain impacted the frontal skull (coup) then rebounded posteriorly (contrecoup). The documented mechanism is biomechanically consistent with and sufficient to cause mild traumatic brain injury. The patient reports immediate onset of headache, dizziness, and confusion beginning at the accident scene, with symptoms progressing over subsequent hours to include nausea, photophobia, and difficulty concentrating—symptom complex characteristic of acute concussion."
Initial evaluation documentation includes detailed symptom inventory using standardized tools (SCAT5), objective examination findings (balance testing errors, cognitive screening deficits), and functional limitations: "Patient demonstrates 8 errors on BESS testing (normal <5 errors), indicating significant balance impairment. MoCA score 22/30 (<26 abnormal) with deficits in attention and delayed recall. Patient unable to complete work tasks requiring sustained attention, forcing medical leave from employment as [OCCUPATION]."
Serial examinations document symptom evolution and treatment response, critical for establishing persistent injury: "Week 2: Patient reports partial improvement in headache (VAS 8→5) but worsening cognitive symptoms as attempted return to work. Concentration deficit interferes with work performance. SCAT5 symptom severity score 42 (moderate). Week 4: Persistent symptoms despite conservative management, now meeting criteria for post-concussion syndrome. MoCA remains 23/30. Patient unable to work full-time. Week 8: Following vestibular rehabilitation and sub-threshold exercise protocol, symptoms improved to mild severity (SCAT5 score 18). Returned to work 50% capacity with accommodations."
Imaging correlation is documented even when normal: "Head CT obtained [DATE] demonstrates no acute intracranial hemorrhage, mass effect, or skull fracture. The absence of structural abnormality on CT does not exclude concussion, as this injury primarily affects neurometabolic function and axonal integrity not visible on standard imaging. The patient's clinical presentation including documented mechanism, immediate symptom onset, and objective examination abnormalities confirm the diagnosis of mild traumatic brain injury."
Causation statements are clearly articulated: "Within a reasonable degree of medical certainty, this patient's traumatic brain injury including post-concussion syndrome is directly and proximately caused by the motor vehicle collision of [DATE]. The temporal relationship (immediate symptom onset), documented mechanism consistent with concussion, objective findings on standardized testing, and typical symptom progression support causation. The patient had no prior history of head injury, cognitive impairment, or similar symptoms per review of prior medical records obtained from [PRIOR PROVIDERS]. The current condition represents new injury directly attributable to the accident."
Functional limitations are documented with specificity supporting economic damages claims: "Patient's concussion creates measurable functional impairments: (1) Cognitive: Cannot perform work tasks requiring sustained attention, multitasking, or complex problem-solving for more than 20-30 minutes before cognitive fatigue forces breaks. Processing speed reduced to 60% of age-matched norms per ImPACT testing. (2) Physical: Cannot exercise at pre-injury intensity due to exertional headache and dizziness. (3) Social: Cannot tolerate loud restaurants, social gatherings, or bright environments due to sensory sensitivity. (4) Sleep: Requires 10-12 hours sleep nightly vs. pre-injury 7-8 hours, limiting productive hours. These limitations have forced reduced work hours (40→20 hours weekly) with corresponding income loss of approximately $30,000 annually."
Treatment necessity documentation justifies past and future medical expenses: "Patient requires ongoing vestibular rehabilitation (12 sessions completed, 8 additional sessions recommended), neuropsychological cognitive rehabilitation (10 sessions), and possible pharmacological management with headache prophylaxis. Conservative estimated future medical costs: vestibular therapy $1,200, cognitive rehabilitation $1,500, medications $600 annually, annual follow-up evaluations $400, total $3,700 annually for estimated 1-2 years = $5,500-7,400 future medical expenses. Additionally, patient faces 10-20% increased risk of developing chronic headache disorder, early-onset dementia risk elevation with TBI history, and potential need for ongoing cognitive support if persistent deficits remain after one year."
Permanent impairment ratings for concussions reaching maximum medical improvement with residual deficits use AMA Guides: "Patient has reached MMI 12 months post-injury with residual deficits including mild persistent headache (2-3 days weekly), attention/concentration mildly below normative data, and exercise-induced symptom exacerbation limiting high-intensity activity. Using AMA Guides to Evaluation of Permanent Impairment, 6th Edition, Chapter 13 (Central and Peripheral Nervous System), patient has Class 1 impairment (5-8% whole person impairment) based on objective evidence of brain injury with mild functional limitations."
Expert witness testimony explaining concussion pathophysiology, symptom legitimacy despite normal imaging, and long-term prognosis helps juries understand this "invisible injury." Our physicians have extensive experience testifying in depositions and trials regarding traumatic brain injury causation, treatment, and outcomes.
- Detailed mechanism documentation correlating biomechanics with concussion pathophysiology
- Standardized symptom assessments (SCAT5) providing objective quantification
- Serial examinations documenting symptom evolution and treatment response
- Imaging correlation with explanation that normal CT doesn't exclude concussion
- Causation opinions stated within reasonable medical certainty
- Functional limitations documented with economic impact (work capacity loss)
- Treatment necessity justification for past and future medical expenses
- Permanent impairment ratings using AMA Guides at maximum medical improvement
- Expert witness testimony for depositions and trial
- Coordination with life care planners for catastrophic TBI cases
While most concussions are managed on an outpatient basis through our clinic, certain signs and symptoms indicate potentially life-threatening complications including intracranial hemorrhage, cerebral edema, or brain herniation requiring emergency neurosurgical evaluation. Patient and family education about these red flags is critical for preventing catastrophic outcomes.
Decreasing level of consciousness is the most concerning warning sign: if the patient becomes increasingly drowsy, difficult to arouse, or unresponsive after initially being awake and conversant, this suggests evolving intracranial mass effect from hemorrhage or edema. Epidural hematomas classically present with initial loss of consciousness at impact, a "lucid interval" lasting minutes to hours where the patient appears relatively normal, then rapid deterioration as the hematoma enlarges. This pattern requires immediate CT and often emergency craniotomy. We instruct families to check on patients every 2-3 hours during the first 24 hours, ensuring they can be awakened and respond appropriately.
Seizure activity including generalized tonic-clonic seizures (full-body convulsions) or focal seizures (localized shaking, staring spells, altered awareness) indicates cortical irritation from contusion, hemorrhage, or edema. Post-traumatic seizures occur in 5-10% of moderate to severe TBI but are rare in mild concussion. Any seizure warrants emergency evaluation with CT imaging and EEG, as anticonvulsant therapy may be needed and seizures can indicate surgical lesions.
Severe or worsening headache despite medication, particularly if described as "the worst headache of my life," suggests intracranial hemorrhage with rising intracranial pressure. While headache is expected in concussion, progressive worsening or headache of extraordinary severity (patient rating 10/10) mandates CT evaluation. Thunderclap headache (sudden maximal intensity) raises concern for subarachnoid hemorrhage, particularly if associated with nuchal rigidity (stiff neck).
Repeated vomiting (>2 episodes) beyond the initial hours post-injury suggests elevated intracranial pressure. While isolated vomiting once or twice in the immediate aftermath of concussion is common and benign, persistent or recurrent vomiting hours later is concerning. Projectile vomiting (forceful ejection without preceding nausea) is particularly worrisome for elevated ICP.
Focal neurological deficits including unilateral weakness or numbness in arm or leg, facial droop or asymmetry, slurred speech, visual field defects (loss of vision in specific areas), dilated pupil or pupillary asymmetry (anisocoria), and abnormal eye movements all suggest focal brain injury from hemorrhage or contusion affecting specific brain regions. These findings mandate immediate CT and neurosurgical consultation.
Altered mental status beyond initial confusion is concerning: if the patient becomes agitated, combative, or exhibits personality changes dramatically different from baseline, this suggests frontal lobe injury or elevated ICP. Conversely, profound lethargy where the patient shows no interest in surroundings and responds only to painful stimuli indicates severe injury. Persistent confusion beyond the first 2-3 hours, particularly if worsening rather than improving, warrants imaging.
Glasgow Coma Scale (GCS) provides standardized assessment: eyes opening (spontaneous=4, to voice=3, to pain=2, none=1), verbal response (oriented=5, confused=4, inappropriate words=3, incomprehensible sounds=2, none=1), motor response (obeys commands=6, localizes pain=5, withdraws from pain=4, abnormal flexion=3, abnormal extension=2, none=1). GCS <15 indicates need for CT imaging; GCS <13 mandates emergency department evaluation; GCS ≤8 indicates severe TBI requiring ICU admission and often intubation.
Draining fluid from ears or nose (CSF leak indicating skull fracture), clear or blood-tinged drainage particularly if it forms a "halo sign" on gauze (blood center with clear ring), Battle's sign (bruising behind ears appearing 1-2 days post-injury suggesting basilar skull fracture), or raccoon eyes (periorbital ecchymosis suggesting anterior skull base fracture) all indicate skull fracture requiring immediate evaluation. While not all skull fractures require surgery, they increase risk of intracranial injury.
Anticoagulation use including warfarin, direct oral anticoagulants (DOACs like apixaban, rivaroxaban), or antiplatelet agents (Plavix, aspirin) increases hemorrhage risk, warranting lower threshold for CT imaging. These patients should proceed to emergency department for evaluation even with apparently minor head trauma.
When any red flag symptom develops, we direct patients immediately to emergency departments with 24/7 neurosurgical capabilities: Memorial Hermann Southeast Hospital (Houston), Houston Methodist Baytown Hospital, Clear Lake Regional Medical Center, or Ben Taub Hospital (Harris Health System). We provide direct communication with emergency physicians regarding our clinical findings and concerns. After emergency stabilization and neurosurgical management if needed, patients return to our clinic for ongoing post-acute care and rehabilitation coordination.
- Decreasing level of consciousness - increasing drowsiness or difficulty arousing - CALL 911
- Seizure activity - convulsions, shaking, staring spells - EMERGENCY
- Severe or worsening headache unrelieved by medication - possible hemorrhage
- Repeated vomiting (>2 episodes) hours after injury - elevated ICP
- Focal neurological deficits - weakness, numbness, facial droop, vision loss
- Unequal pupils or dilated pupil - suggests mass effect or herniation
- Profound confusion or agitation worsening rather than improving
- Drainage of clear fluid from nose or ears - CSF leak, skull fracture
- Battle's sign or raccoon eyes - skull fracture indicators
- Glasgow Coma Scale <15 - requires immediate CT imaging
- Loss of consciousness >30 seconds - warrants emergency evaluation
- Patients on blood thinners with any head impact - lower threshold for ER
While many accidents causing concussions are unavoidable, evidence-based prevention strategies reduce injury risk and severity. Understanding these measures benefits patients recovering from concussion (preventing repeat injury during vulnerable period) and the general public.
Vehicle safety measures proven to reduce TBI include proper seatbelt use (reducing head impact risk by 60% in frontal crashes), airbag functionality (ensuring airbags aren't deactivated and occupants maintain proper distance from steering wheel), proper headrest positioning (top of headrest level with top of head, 2-3 inches from skull, reducing whiplash and associated concussion), appropriate car seat selection and installation for children (rear-facing until age 2, forward-facing with harness until age 4, booster until properly fitting seatbelt), and avoiding distracted driving (texting, phone use, eating while driving increases collision risk exponentially).
Defensive driving practices reduce accident risk: maintaining safe following distance (3-second rule minimum), scanning environment for potential hazards, avoiding aggressive driving behaviors, adjusting speed for conditions, and expecting unexpected actions from other drivers. In Pasadena's high-traffic areas including Highway 225, I-45, and Fairmont Parkway, heightened vigilance during rush hours, around industrial facilities with large truck traffic, and at major intersections reduces crash probability.
Fall prevention in home and workplace environments includes good lighting (especially stairways and bathrooms), removing tripping hazards (loose rugs, clutter, electrical cords), installing handrails on stairs, using non-slip mats in bathrooms and kitchens, prompt cleanup of spills, proper footwear with good traction, and assistive devices (canes, walkers) for those with balance or mobility impairment. Workplace fall prevention includes proper scaffolding, guardrails, personal fall arrest systems for work at heights, and slip-resistant flooring in areas prone to moisture.
Post-concussion precautions during recovery are critical for preventing second impact syndrome: absolute avoidance of contact sports and high-risk activities (skiing, skateboarding, horseback riding) until symptom-free and cleared by physician, no driving in acute phase (first 24-48 hours minimum) and cautious limited driving until reaction time normalizes, avoiding alcohol which impairs recovery and increases re-injury risk through impaired judgment and balance, using caution in environments with fall risk (crowds, uneven surfaces, dim lighting), and informing family members and coworkers about injury so they can provide monitoring and assistance. Patients with history of concussion should consider avoiding future contact sport participation given cumulative injury risks, particularly if this concussion was their second or third.
Workplace safety in Pasadena's industrial sector includes hard hat use (reduces skull fracture and severe TBI but doesn't fully prevent concussion), situational awareness around heavy equipment and moving machinery, proper lockout/tagout procedures preventing unexpected equipment start-up, confined space safety protocols, and prompt reporting of unsafe conditions. Employers should provide concussion education to workers and supervisors, establish protocols for removing injured workers from duty and ensuring medical evaluation before return to work, and avoid pressuring workers to continue working while symptomatic.
Recognition of subtle concussion symptoms allows early treatment improving outcomes: many accident victims don't realize they've sustained concussion, attributing symptoms to "stress" or "being shaken up." Education about concussion symptoms empowers patients to seek care promptly. We encourage all patients involved in significant accidents with head trauma mechanism—even without direct head impact—to undergo concussion screening, as early diagnosis within 24-48 hours is associated with faster recovery and reduced PCS rates.
Post-recovery, patients should maintain brain health through cognitively stimulating activities, physical exercise supporting cerebrovascular health, Mediterranean diet rich in antioxidants and omega-3 fatty acids, management of vascular risk factors (hypertension, diabetes, hyperlipidemia), adequate sleep (7-9 hours nightly), stress management, and avoidance of smoking and excessive alcohol. These measures support neuroplasticity and cognitive reserve, maximizing long-term brain health after TBI.
Seek Emergency Care Immediately If You Experience:
- Decreasing level of consciousness or difficulty awakening patient
- Seizure activity (convulsions, shaking, staring spells)
- Severe worsening headache unrelieved by medication (worst of life)
- Repeated vomiting (>2 episodes) hours after injury
- Focal weakness, numbness, facial droop, or vision loss
- Unequal or dilated pupils
- Clear fluid draining from nose or ears (CSF leak)
- Profound confusion, agitation, or personality change
- Glasgow Coma Scale <15 (any altered consciousness)
- Loss of consciousness >30 seconds
- Battle's sign (bruising behind ears) or raccoon eyes
- Patients on blood thinners with any head trauma
Call 911 or go to the nearest emergency room immediately
Need Treatment for Your Injuries?
Don't wait for your injuries to worsen. Get same-day evaluation and treatment from our accident injury specialists. We accept Letter of Protection—$0 out of pocket until your case settles.
Joint & Shoulder Injuries

Shoulder and joint injuries represent some of the most complex and debilitating trauma resulting from motor vehicle accidents, workplace incidents, and slip-and-fall events. The shoulder joint, the body's most mobile articulation, sacrifices stability for range of motion, making it particularly vulnerable to dislocation, rotator cuff tears, and labral injuries. Similarly, knee joints endure tremendous forces during accidents, suffering ACL tears, meniscal damage, and ligament sprains. AccidentDoc Pasadena's board-certified physicians specialize in comprehensive evaluation and treatment of all joint injuries, from acute trauma through complete functional restoration, serving Pasadena's industrial workforce with expertise in construction injuries, refinery accidents, and motor vehicle trauma.
The shoulder complex represents the most intricate joint system in the human body, comprising four distinct articulations: the glenohumeral joint (ball-and-socket), acromioclavicular joint (AC joint connecting clavicle to acromion), sternoclavicular joint (clavicle to sternum), and scapulothoracic articulation (scapula gliding on rib cage). The glenohumeral joint achieves remarkable mobility—180° of forward flexion, 180° of abduction, and 90° of external rotation—through a shallow glenoid socket articulating with the large humeral head. This inherent instability necessitates robust soft tissue support.
The rotator cuff consists of four muscles with tendons converging on the humeral head: supraspinatus (abduction initiation, most commonly torn), infraspinatus (external rotation), teres minor (external rotation and adduction), and subscapularis (internal rotation). These muscles function synergistically to compress the humeral head into the glenoid socket (concavity-compression mechanism) and counteract deltoid's superior pull during arm elevation. The supraspinatus tendon passes through the subacromial space, a narrow corridor between the humeral head and acromion, predisposing it to impingement and degenerative tearing.
The glenoid labrum is a fibrocartilaginous rim deepening the glenoid socket by approximately 50%, enhancing stability. Superior labrum anterior-posterior (SLAP) tears occur when sudden traction or compression forces disrupt this structure, common in dashboard bracing during frontal collisions or catching oneself during falls. The long head of biceps tendon originates at the superior labrum, explaining why SLAP tears often present with anterior shoulder pain and bicipital groove tenderness.
Shoulder ligaments provide static stability: the superior, middle, and inferior glenohumeral ligaments resist anterior and inferior translation at various arm positions. The coracohumeral ligament resists inferior subluxation. High-energy trauma can tear these ligaments, causing instability patterns requiring surgical reconstruction.
The knee joint, the body's largest articulation, comprises the tibiofemoral joint (femoral condyles on tibial plateau) and patellofemoral joint (kneecap tracking on femur). Cruciate ligaments provide anteroposterior stability: the anterior cruciate ligament (ACL) prevents anterior tibial translation and internal rotation, most commonly torn during dashboard impacts, twisting injuries, or hyperextension. The posterior cruciate ligament (PCL) prevents posterior tibial translation, classically injured in dashboard knee when the tibia is driven posteriorly. Collateral ligaments resist varus-valgus stress: medial collateral ligament (MCL) prevents valgus (knee bowing inward), lateral collateral ligament (LCL) prevents varus (knee bowing outward).
Menisci are C-shaped fibrocartilage structures (medial and lateral) serving as shock absorbers, load distributors, and stability enhancers. They increase contact area between femoral condyles and tibial plateau by 50-70%, reducing peak contact pressures. Meniscal tears result from rotational forces with the knee flexed and weight-bearing, or from direct compression in accidents. The medial meniscus, firmly attached to the joint capsule and MCL, is less mobile and more frequently torn than the lateral meniscus.
Understanding this complex anatomy guides diagnostic and treatment approaches. Shoulder injuries often involve multiple structures simultaneously—rotator cuff tears commonly coexist with labral pathology and AC joint sprains. Similarly, knee injuries frequently combine ligament and meniscal damage, requiring comprehensive evaluation rather than single-structure focus.
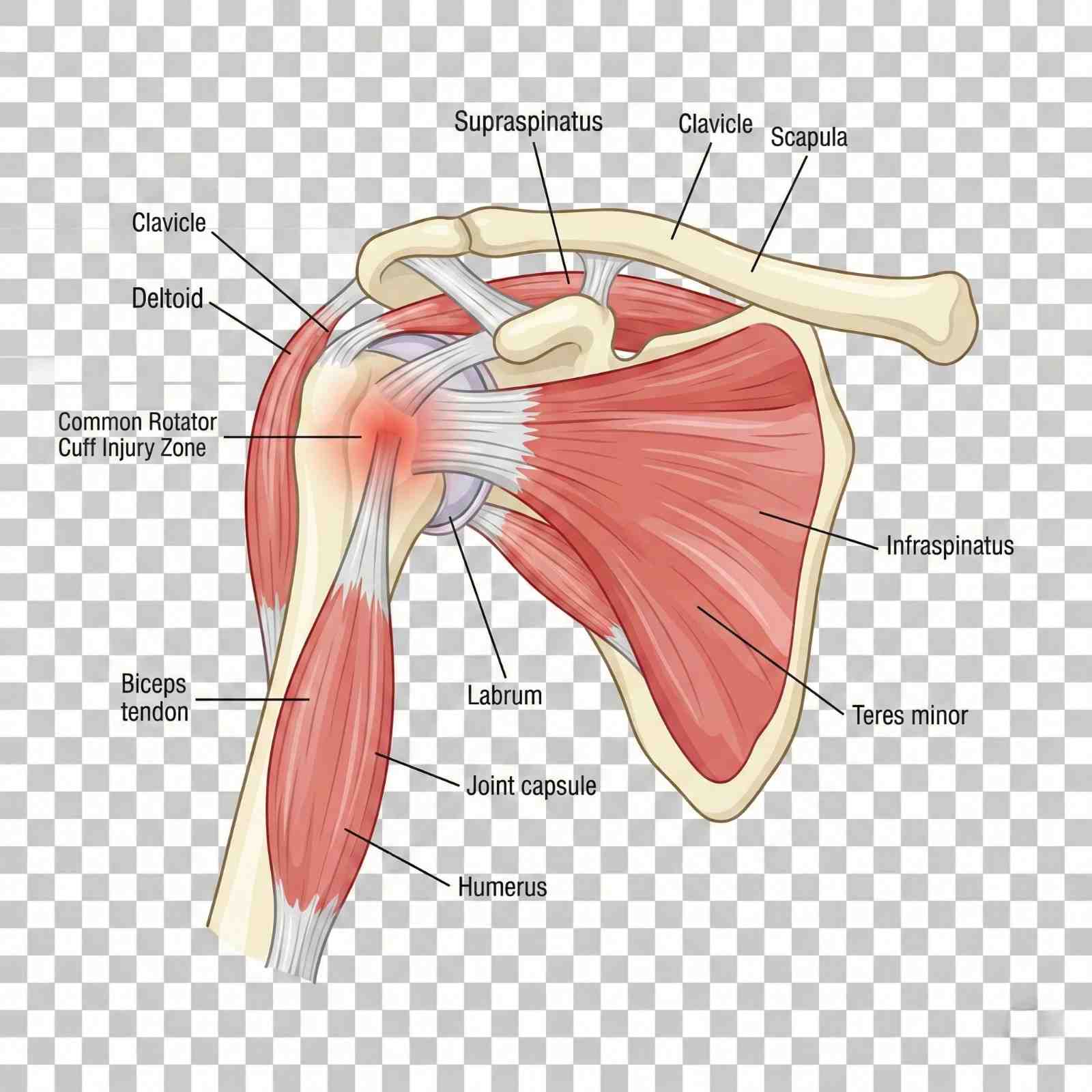
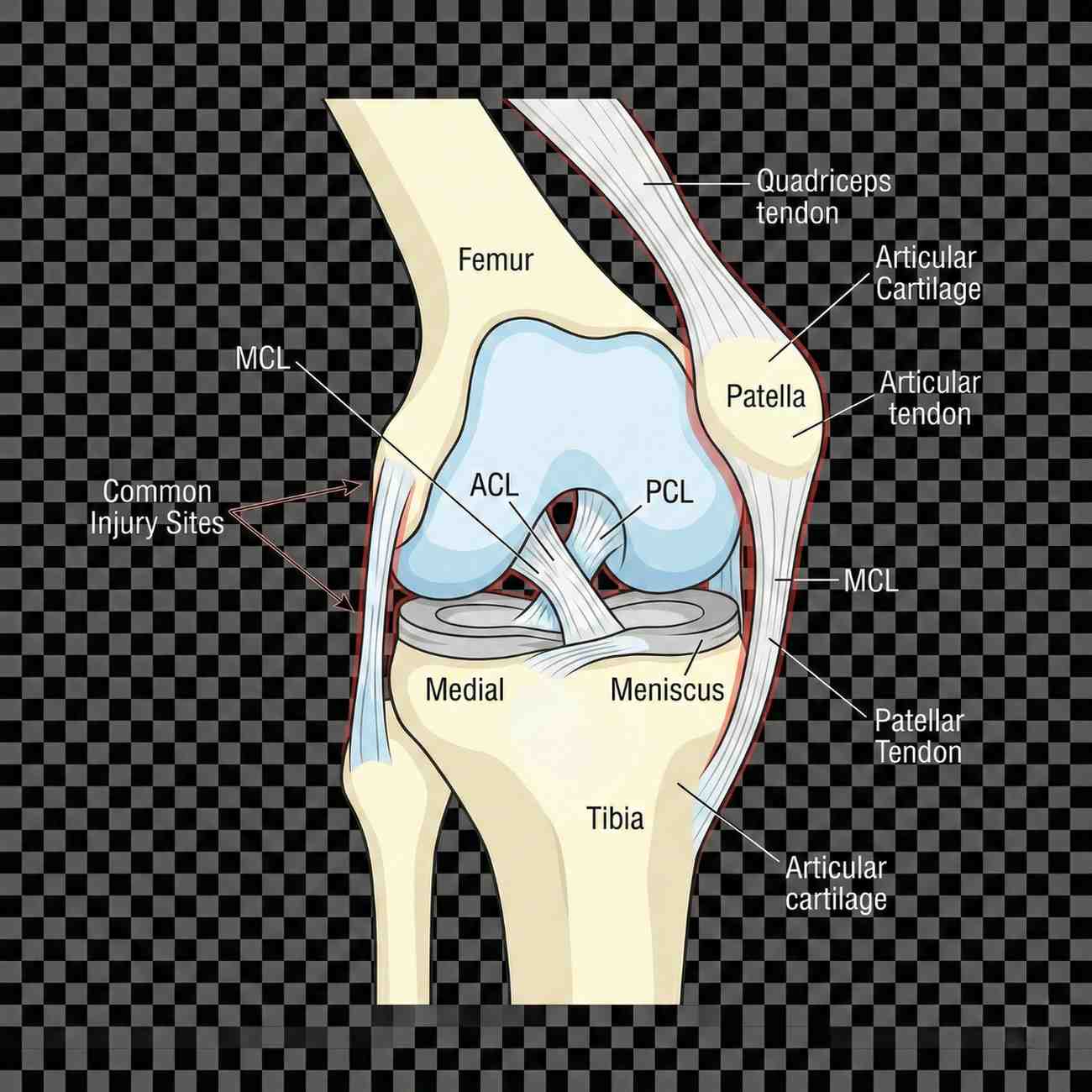
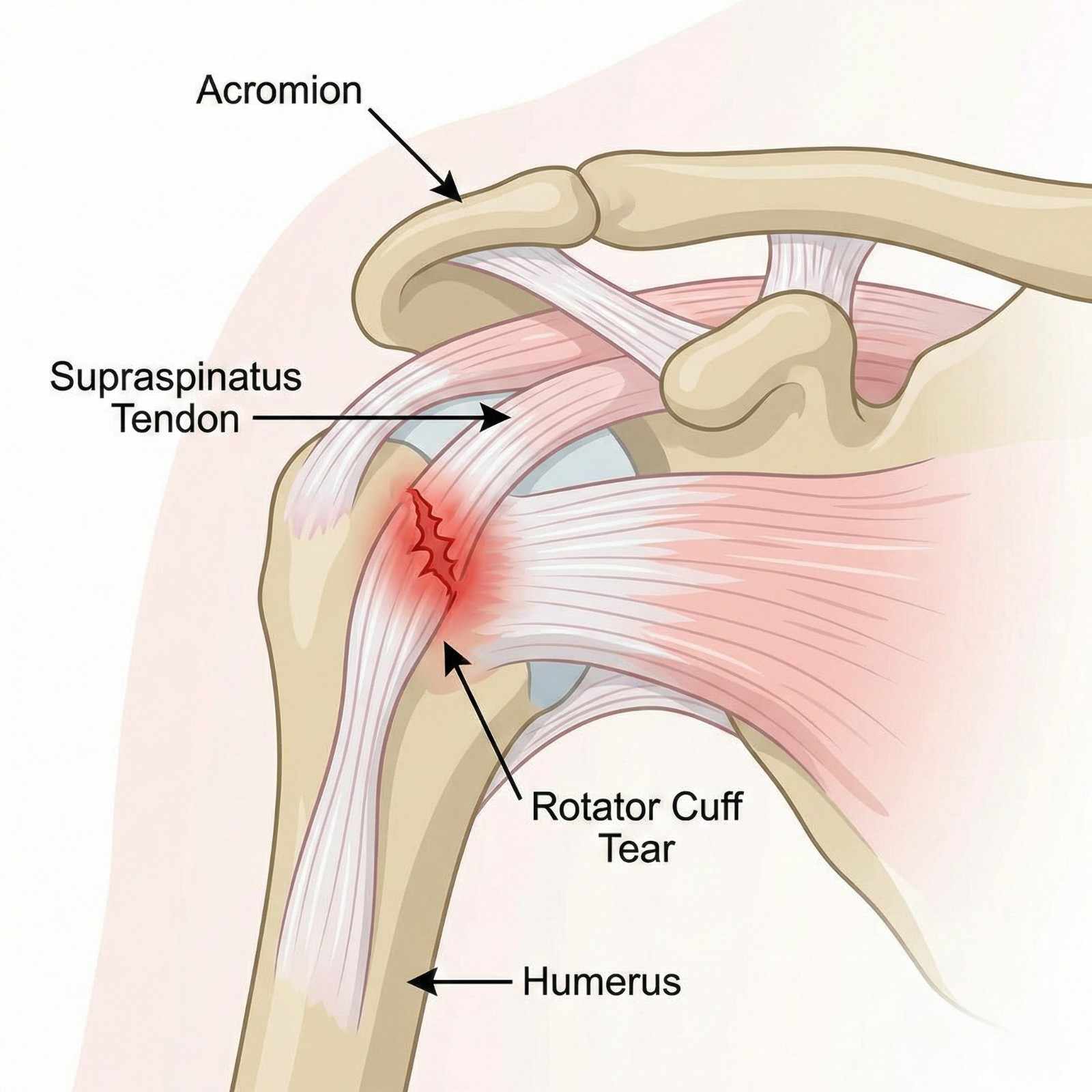
Joint injuries present with variable symptom patterns depending on structures injured, injury mechanism, and timing since trauma. Recognizing these presentations guides differential diagnosis and treatment planning.
Shoulder injuries typically manifest with anterior, lateral, or posterior pain depending on structures involved. Rotator cuff tears produce lateral shoulder pain radiating into the deltoid region, worse with overhead activities, reaching behind the back, or sleeping on the affected side. Night pain is characteristic—patients often report inability to sleep on the injured shoulder. Weakness with arm elevation, particularly abduction between 60-120° (painful arc), suggests supraspinatus involvement. Complete tears produce profound weakness—patients cannot initiate abduction or maintain arm elevation against gravity (positive drop arm test).
Shoulder dislocations cause severe acute pain, visible deformity with the arm held in slight abduction and external rotation, and reluctance to move the shoulder. Anterior dislocations (95% of cases) result from arm abduction with external rotation and extension, classic during motor vehicle accidents when bracing against dashboard or during falls on outstretched hand. The humeral head displaces anteriorly, creating a "squared-off" shoulder appearance compared to the opposite side. Associated axillary nerve injury occurs in 10-40% of cases, producing deltoid weakness and numbness over the lateral upper arm—this must be documented before and after reduction attempts.
AC joint separations produce point tenderness and often visible deformity at the top of the shoulder where the clavicle meets the acromion. Grade 1 sprains cause tenderness without visible deformity. Grade 2 injuries show mild elevation of the distal clavicle compared to the opposite shoulder. Grade 3-6 separations demonstrate obvious clavicle elevation ("piano key sign"—pressing down on the prominent clavicle causes it to spring back up). Pain worsens with cross-body adduction (bringing arm across chest) and overhead activities.
Labral tears, particularly SLAP lesions, cause deep anterior shoulder pain, often described as catching or clicking with overhead motions. Patients may report feeling that the shoulder "gives way" or "goes dead" during activities. Pain radiating into the biceps region is common. SLAP tears are notoriously difficult to diagnose clinically and often require MRI arthrog raphy for confirmation.
Knee injuries present distinct patterns. ACL tears typically occur during non-contact twisting injuries or dashboard impacts. Patients often report hearing or feeling a "pop" at injury, followed by immediate swelling (hemarthrosis developing within hours rather than days suggests ACL tear). The knee feels unstable or "gives way" during cutting or pivoting movements. Chronic ACL deficiency causes recurrent instability episodes and risk of secondary meniscal and cartilage damage.
MCL sprains cause medial knee pain and tenderness along the ligament course. Grade 1 sprains produce pain with valgus stress but maintain stability. Grade 2 tears show increased laxity with valgus stress but maintain a firm endpoint. Grade 3 complete tears demonstrate gross instability with no firm endpoint. Isolated MCL injuries have good healing potential with conservative treatment, but combined ACL-MCL injuries may require surgical reconstruction.
Meniscal tears cause mechanical symptoms: catching, locking (inability to fully extend the knee), or giving way. Pain localizes to the medial or lateral joint line depending on which meniscus is torn. A "locked" knee unable to extend beyond 15-20° flexion suggests displaced meniscal fragment blocking full extension—this requires urgent orthopedic evaluation. Swelling typically develops gradually over 12-24 hours (synovitis from mechanical irritation) rather than immediately (distinguishing from ligament injuries with hemarthrosis).
Patellofemoral injuries range from patellar dislocation to chondral fractures. Patellar dislocations cause immediate lateral knee pain, often with visible deformity (patella displaced laterally). Many dislocations spontaneously reduce before medical evaluation. Patients report feeling the kneecap "slide out of place." Significant swelling and tenderness along the medial retinaculum (torn during lateral dislocation) are present. Recurrent patellar instability affects 15-50% of patients after initial dislocation.
Bursitis commonly develops after direct trauma. Prepatellar bursitis (housemaid's knee) from kneeling impacts causes anterior knee swelling directly over the kneecap. Olecranon bursitis from elbow impacts produces posterior elbow swelling. Trochanteric bursitis causes lateral hip pain worse with lying on that side. These inflammatory conditions require distinction from septic bursitis (infected bursa requiring aspiration and antibiotics).
Red flag symptoms requiring urgent evaluation include diminished pulses distal to injury (vascular compromise), progressive neurological deficits (nerve injury), fever with joint swelling (septic arthritis), severe pain disproportionate to exam findings with tense swelling (compartment syndrome), and open joint injuries with visible bone or articular cartilage (infection risk).
Accurate diagnosis of joint injuries requires systematic physical examination combined with strategic imaging studies. Clinical examination provides immediate diagnostic information, while imaging confirms clinical suspicions and identifies associated injuries not apparent on examination.
Shoulder examination begins with inspection: observe for deformity, atrophy, or asymmetry compared to the opposite side. Palpate bony landmarks—acromioclavicular joint, coracoid process, bicipital groove, and greater tuberosity—identifying point tenderness. Range of motion testing quantifies functional limitations: forward flexion (normal 180°), abduction (normal 180°), external rotation with arm at side (normal 60-90°), and internal rotation assessed by hand-behind-back reach (normal to mid-scapula level).
Specific provocative tests isolate injured structures. The Jobe test (empty can test) evaluates supraspinatus: patient abducts arms to 90° in scapular plane (30° forward of coronal plane), internally rotates shoulders (thumbs pointing down), and resists downward pressure—pain or weakness indicates supraspinatus pathology. External rotation strength testing targets infraspinatus and teres minor. The lift-off test examines subscapularis: patient places hand behind back and attempts to lift hand away from back against resistance.
Impingement tests reproduce pain from subacromial pathology. Neer's impingement sign: examiner forward flexes patient's arm to maximum elevation while preventing scapular rotation—pain suggests impingement. Hawkins-Kennedy test: arm flexed to 90° then internally rotated—pain indicates impingement.
Instability testing assesses ligamentous integrity. Apprehension test: patient supine, arm abducted 90° and externally rotated—apprehension or pain suggests anterior instability. Relocation test: posterior pressure on humeral head while in apprehension position relieves pain, confirming anterior instability. Sulcus sign: downward traction on the arm creates visible sulcus below acromion, indicating inferior instability.
Labral tests detect tears. O'Brien's test (active compression test): arm forward flexed 90°, adducted 10-15°, and internally rotated (thumb down); patient resists downward force—pain suggests labral pathology, particularly SLAP tears.
Knee examination evaluates ligamentous stability. Lachman test is most sensitive for ACL tears: knee flexed 20-30°, examiner stabilizes femur and applies anterior force to proximal tibia—excessive anterior translation with soft or absent endpoint indicates ACL tear. Anterior drawer test (knee flexed 90°) is less sensitive but more specific. Pivot shift test mimics giving-way sensation: knee extended then flexed while applying valgus and internal rotation forces—sudden reduction of subluxed tibia confirms ACL deficiency.
Valgus stress testing evaluates MCL: knee at 0° (tests MCL and capsule) and 30° flexion (isolates MCL)—increased laxity indicates injury severity. Varus stress tests LCL similarly. Posterior drawer test assesses PCL integrity.
Meniscal tests include McMurray's test: knee fully flexed, tibia internally rotated and knee extended while applying valgus stress (medial meniscus), or externally rotated with varus stress (lateral meniscus)—pain or clicking suggests meniscal tear. Thessaly test: patient stands on one leg, knee flexed 20°, and internally/externally rotates body—pain suggests meniscal pathology.
Imaging studies confirm clinical diagnoses. X-rays are first-line for all joint injuries: standard shoulder series includes AP, lateral (Y-view or scapular lateral), and axillary views identifying fractures, dislocations, and degenerative changes. AC joint views with and without weights quantify AC separation severity. Knee X-rays include AP, lateral, and sunrise (patellofemoral) views. Standing films assess alignment and joint space narrowing. Stress views may be obtained for ligament injuries.
MRI is gold standard for soft tissue injuries: rotator cuff tears (90% sensitivity/specificity), labral tears, ligament injuries, meniscal tears, and cartilage defects. MRI arthrography (contrast injected into joint) improves labral tear detection. Standard protocol MRI without contrast typically suffices for most injuries.
Ultrasound performed by experienced operators can diagnose rotator cuff tears with accuracy comparable to MRI. Advantages include lower cost, real-time dynamic assessment, and lack of contraindications. Limitations include operator dependence and inferior visualization of labrum and glenohumeral ligaments.
CT scans excel for bony detail: fracture characterization, alignment assessment, and surgical planning. CT arthrography can detect labral tears when MRI is contraindicated.
At AccidentDoc Pasadena, we provide in-office X-rays for immediate fracture assessment and arrange expedited MRI within 72 hours when soft tissue injuries require confirmation. This rapid diagnostic approach ensures treatment begins promptly, crucial for optimal outcomes and medico-legal documentation.
Joint injury treatment spans conservative management for mild-moderate injuries to surgical reconstruction for severe trauma, guided by injury severity, functional demands, and patient goals. Most joint injuries initially receive conservative treatment, progressing to surgery only when non-operative approaches fail or injury severity mandates surgical intervention.
Acute phase management (first 2 weeks) focuses on controlling pain and inflammation while protecting injured structures. RICE protocol (Rest, Ice, Compression, Elevation) remains foundational. Ice application 20 minutes every 2-3 hours during the first 48-72 hours reduces swelling and pain. Compression with elastic wraps or braces controls edema. Elevation above heart level utilizes gravity for fluid drainage.
Immobilization duration requires careful balance. Shoulder slings prevent painful motion and protect healing tissues but should be limited to 1-2 weeks maximum for most injuries (excluding fractures and surgical repairs) to prevent stiffness. Range of motion exercises begin early, even during immobilization periods, to maintain mobility. Complete immobilization causes rapid loss of motion—shoulder stiffness develops within days, particularly in patients over 40 years old.
Knee bracing provides stability for ligament injuries. Hinged knee braces allow controlled range of motion while restricting potentially harmful varus-valgus stress. ACL braces help prevent giving-way episodes in ACL-deficient knees for patients opting for non-operative management or awaiting surgery. Patellar stabilizing braces prevent lateral subluxation in patellofemoral instability.
Pharmacological management utilizes NSAIDs for anti-inflammatory and analgesic effects. Ibuprofen 400-600mg three times daily or naproxen 500mg twice daily provides adequate relief for most patients. Patients with cardiovascular risk factors, kidney disease, or gastrointestinal ulcer history may require alternatives. Acetaminophen 1000mg three-four times daily provides analgesia without anti-inflammatory effects. Topical NSAIDs (diclofenac gel) offer localized pain relief with minimal systemic absorption, useful for patients unable to tolerate oral NSAIDs. Short courses of oral corticosteroids (methylprednisolone dose pack) may be prescribed for severe inflammation.
Corticosteroid injections provide targeted anti-inflammatory therapy. Subacromial injections for rotator cuff tendinopathy combine corticosteroid with local anesthetic, providing both immediate pain relief and anti-inflammatory effects lasting weeks to months. AC joint injections treat AC joint arthritis and sprains. Knee injections address inflammatory arthritis, bursitis, or as temporizing treatment for degenerative changes. While effective for pain relief, corticosteroid injections do not heal torn tendons or ligaments and should be used judiciously—repeated injections can cause tendon weakening or cartilage damage.
Hyaluronic acid (viscosupplementation) injections for knee osteoarthritis provide lubrication and potential disease-modifying effects, though evidence remains controversial. A series of 3-5 injections given weekly may provide months of symptom relief.
Platelet-rich plasma (PRP) injections represent regenerative medicine approach: patient's blood is centrifuged to concentrate platelets containing growth factors, then injected into injured tissues. Evidence supports PRP for partial rotator cuff tears and knee osteoarthritis, though insurance coverage remains limited.
Physical therapy is cornerstone of conservative management. Therapists guide progressive strengthening, restore range of motion, improve proprioception, and correct biomechanical deficiencies contributing to injury. Shoulder therapy focuses on rotator cuff strengthening, scapular stabilization, and restoring normal shoulder mechanics. Knee therapy emphasizes quadriceps strengthening (particularly vastus medialis obliquus for patellar stability), hamstring strengthening, proprioceptive training, and return-to-sport drills for athletes.
Surgical indications for shoulder injuries include complete rotator cuff tears in active patients (surgery within 6 months optimizes outcomes before muscle atrophy and tendon retraction), recurrent shoulder dislocations (particularly in young patients with >90% recurrence risk), displaced fractures, and labral tears causing mechanical symptoms or instability unresponsive to conservative treatment. Arthroscopic techniques allow rotator cuff repair, labral repair, and AC joint reconstruction through small incisions with faster recovery than open procedures.
Knee surgical indications include ACL tears in active individuals or those with instability affecting daily activities (reconstruction typically using patellar tendon or hamstring autograft), displaced meniscal tears causing locking or persistent pain (arthroscopic partial meniscectomy or meniscal repair), and multi-ligament knee injuries. Isolated meniscal tears in patients over 40 with degenerative tears often respond to conservative management, avoiding surgery.
Recovery timelines vary by injury severity and treatment approach. Minor sprains and strains resolve in 4-8 weeks with conservative treatment. Moderate injuries requiring aggressive rehabilitation may need 3-4 months for return to full activities. Surgical reconstructions typically require 4-6 months for return to sports, with full strength restoration taking 9-12 months. At AccidentDoc Pasadena, we coordinate with orthopedic surgeons when surgical evaluation is indicated, ensuring seamless care transitions while maintaining continuity for non-operative management.
Joint injury recovery follows predictable phases, though individual timelines vary based on injury severity, age, comorbidities, and treatment adherence. Understanding expected progressions helps patients maintain realistic expectations and clinicians identify concerning deviations requiring intervention.
Acute inflammatory phase (days 0-7) involves hemostasis and initial inflammatory response. Tissues are fragile and susceptible to re-injury. Pain and swelling peak within 24-72 hours. Treatment focuses on protection (immobilization or bracing), pain control, and edema management. Gentle range of motion exercises begin immediately for most injuries to prevent stiffness, performed within pain-free ranges. Strengthening is contraindicated during this phase.
Proliferative phase (weeks 1-6) encompasses tissue repair. Fibroblasts produce collagen forming scar tissue bridging injured structures. This new tissue is weak and disorganized. Treatment emphasizes gradual mobilization, progressive range of motion exercises, and introduction of light strengthening. Joint mobilization techniques improve mechanics. Modalities including ultrasound and electrical stimulation may accelerate healing. Pain should decrease progressively—persistent or worsening pain suggests inadequate healing or complications.
Remodeling phase (weeks 6-12+) involves collagen reorganization along stress lines, increasing tensile strength. Treatment focuses on progressive strengthening, functional training, and return-to-activity protocols. For surgical reconstructions, tissue healing requires longer—tendon-to-bone healing (rotator cuff repair, ACL reconstruction) takes 3-4 months for secure biologic incorporation. Protected loading during this period prevents graft failure.
Shoulder rehabilitation protocols vary by injury. Rotator cuff tendinopathy without full-thickness tear: weeks 1-2 focus on pain control and gentle range of motion. Weeks 3-6 introduce scapular stabilization and rotator cuff strengthening using resistance bands. Weeks 7-12 progress to sport-specific training. Full return to overhead activities typically occurs at 3-4 months.
Post-operative rotator cuff repair requires more conservative progression due to tendon-to-bone healing requirements. Phase 1 (weeks 0-6): passive range of motion only (therapist moves arm, patient relaxed) with sling immobilization between exercises. Phase 2 (weeks 6-12): active-assisted then active range of motion begins. Phase 3 (weeks 12-20): progressive strengthening begins once healing confirmed on imaging. Phase 4 (months 5-9): advanced strengthening and return to unrestricted activities. Overhead athletes may require 9-12 months for full return to sport.
Shoulder dislocation rehabilitation: first-time dislocations in young patients have 90% recurrence risk without surgery, so early surgical stabilization is often recommended. Post-stabilization surgery protocol: weeks 0-6 immobilization in sling, pendulum exercises only. Weeks 6-12: progressive range of motion restoration. Months 3-4: strengthening begins. Months 5-6: return to non-contact sports. Months 6-9: return to contact sports with protective bracing.
ACL reconstruction rehabilitation: immediate post-operative phase (weeks 0-2) focuses on edema control, restoring full extension (crucial to prevent arthrofibrosis), and initiating quadriceps activation. Protected weight-bearing with crutches advances to full weight-bearing as tolerated. Weeks 2-6: restore full flexion, progress closed-chain strengthening, maintain extension. Months 2-3: progressive strengthening, proprioceptive training, initiate straight-line jogging. Months 3-4: advance running program, sport-specific drills. Months 5-6: functional testing (hop tests, strength testing) guides return-to-sport decisions—return when achieving >90% limb symmetry on objective testing. Full return typically at 6-9 months for recreational athletes, 9-12 months for competitive athletes.
Meniscal tear rehabilitation depends on treatment. Meniscectomy (partial removal) allows rapid progression: immediate weight-bearing, full range of motion as tolerated, return to sports at 4-8 weeks once strength restored. Meniscal repair requires slower progression to protect healing: 6 weeks partial weight-bearing, restricted motion, then gradual advancement. Full return to sports at 4-6 months post-repair.
Complications affecting recovery include arthrofibrosis (abnormal scar causing stiffness), particularly after shoulder surgery or prolonged immobilization—aggressive physical therapy and occasionally surgical lysis of adhesions may be required. Complex regional pain syndrome (CRPS, formerly reflex sympathetic dystrophy) causes disproportionate pain, allodynia, vasomotor changes, and progressive dysfunction—requires specialized pain management. Re-injury from premature return to activity sets recovery back weeks to months.
Return-to-work considerations depend on occupational demands. Sedentary desk work may resume in 1-2 weeks for most injuries. Light-duty work with lifting restrictions up to 10-20 lbs may be possible at 4-6 weeks. Heavy manual labor, construction, or warehouse work typically requires 8-12 weeks minimum, longer for surgical repairs. Work restrictions must balance functional recovery with financial necessity—we work closely with employers to facilitate modified duty when possible, preventing prolonged work absence.
Return-to-sport decisions require objective criteria, not arbitrary timelines. Athletes must demonstrate full pain-free range of motion, >85-90% strength compared to opposite side, sport-specific functional capacity, and psychological readiness. Functional tests including hop tests (single-leg hop, crossover hop, triple hop for distance) and cutting maneuvers assess readiness. Premature return risks re-injury with potentially worse outcomes than original injury.
Comprehensive documentation is essential for joint injury claims, as insurance companies frequently dispute causation, necessity of treatment, and permanency of impairments. AccidentDoc Pasadena provides detailed medical-legal documentation specifically designed to support litigation and workers' compensation proceedings.
Injury mechanism documentation establishes causation through biomechanical correlation: "Patient sustained right shoulder injury on [DATE] during motor vehicle collision when struck from left side by vehicle traveling estimated 40 mph. The lateral impact created sudden valgus and external rotation force on the braced right arm as patient gripped steering wheel, producing mechanism consistent with rotator cuff tear and labral injury. This specific injury mechanism is biomechanically sufficient to cause documented pathology." Detailed mechanism description correlates accident forces with tissue damage patterns, rebutting insurance arguments that injuries pre-existed or arose from degenerative processes.
Initial evaluation documentation establishes temporal relationship and baseline severity: "Patient presented [X days] post-accident reporting immediate onset right shoulder pain and inability to lift arm above shoulder level. Prior to accident, patient worked as [OCCUPATION] performing [SPECIFIC DUTIES] without shoulder limitations—no prior shoulder injuries or treatments per review of prior medical records obtained from [PROVIDERS]. Physical examination reveals severe limitation of active range of motion—forward flexion 80° (normal 180°), abduction 70° (normal 180°), external rotation 20° (normal 90°). Significant weakness with resisted abduction (2/5 strength). Positive impingement signs, positive drop arm test. These findings are acute, causally related to documented trauma, and represent new injury not present pre-accident."
Diagnostic imaging correlation provides objective evidence: "MRI performed [DATE] demonstrates full-thickness tear of supraspinatus tendon measuring 2.1 cm in anteroposterior dimension with 1.5 cm retraction of tendon edge, indicating complete rupture. Associated findings include moderate muscle atrophy and fatty infiltration (Goutallier grade 2) indicating chronicity of tear. However, clinical correlation with recent trauma and acute symptom onset indicates acute-on-chronic pathology—pre-existing degenerative tendon suffered complete rupture during accident. The acute traumatic component is the predominant cause of current disability and treatment necessity." This language acknowledges imaging findings of degeneration while establishing acute trauma as causative factor, addressing insurance company arguments about pre-existing conditions.
Treatment documentation justifies medical necessity: "Conservative management initiated including subacromial corticosteroid injection ([DATE]), physical therapy (20 sessions from [DATE] to [DATE]), and oral NSAIDs. Despite 4 months of aggressive non-operative treatment, patient demonstrates persistent pain (VAS 7/10), functional limitation (unable to perform overhead work duties), and objective evidence of complete rotator cuff tear. Surgical consultation obtained [DATE]—orthopedic surgeon recommends arthroscopic rotator cuff repair. Surgery is medically necessary to restore function and prevent progressive rotator cuff arthropathy. Without repair, patient faces permanent disability affecting occupational and personal activities."
Surgical documentation details procedures performed: "Patient underwent arthroscopic rotator cuff repair on [DATE] performed by Dr. [SURGEON NAME]. Operative report confirms full-thickness tear of supraspinatus and partial-thickness tear of infraspinatus. Surgical findings consistent with traumatic etiology—tear margins showed acute appearance without significant degenerative fraying. Repair performed using [TECHNIQUE]. Post-operative rehabilitation has progressed through [CURRENT PHASE]. Expected recovery timeline is 6-9 months for return to full duty work."
Functional limitations quantify disability: "Current functional deficits include inability to lift objects above shoulder level (maximum safe lift 10 lbs at waist level), inability to reach overhead, inability to sleep on injured side, and inability to perform [SPECIFIC JOB DUTIES]. These limitations directly result from accident-caused shoulder injury and persist despite treatment. Patient requires ongoing restrictions: no lifting >20 lbs, no overhead reaching, no repetitive use of injured arm until surgical repair healed—estimated [DATE]."
Causation opinions stated with medical certainty: "Within a reasonable degree of medical certainty, this patient's right shoulder rotator cuff tear, labral tear, and associated functional impairments are directly and proximately caused by the motor vehicle collision of [DATE]. The temporal relationship (injury onset coinciding with accident), documented mechanism consistent with injury pattern, absence of prior shoulder complaints or treatment, and objective confirmation on MRI all support causation. Alternative explanations including spontaneous degenerative tear are inconsistent with the clinical presentation."
Permanent impairment ratings when maximum medical improvement (MMI) reached: "Patient reached MMI on [DATE], 12 months post-surgery. Residual impairments include loss of range of motion (forward flexion 160° vs normal 180°, abduction 170° vs 180°), loss of strength (4+/5 vs 5/5 pre-injury), persistent pain with strenuous activities, and permanent work restrictions (no repetitive overhead reaching, maximum lift 30 lbs). Using AMA Guides to Evaluation of Permanent Impairment, 6th Edition, upper extremity impairment is [X]% which converts to [Y]% whole person impairment. This permanent impairment directly resulted from accident and affects patient's earning capacity and quality of life."
Future medical costs are documented: "Patient will require ongoing monitoring with orthopedic follow-up annually to assess for progressive degenerative changes in repaired shoulder. Future treatment needs may include periodic corticosteroid injections (estimated $500 each, up to 2 per year), revision surgery if repair fails (15-20% risk, cost $30,000-50,000), and possible shoulder replacement in 15-20 years if post-traumatic arthritis develops (cost $40,000-60,000). Conservative estimated lifetime future medical costs: $25,000-75,000."
Expert witness testimony explaining biomechanics, causation, and treatment rationale helps juries understand complex joint injuries. Our physicians have testified in Harris County courts regarding shoulder and knee injuries, rotator cuff pathology, surgical necessity, and permanency ratings.
Seek Emergency Care Immediately If You Experience:
- Diminished or absent pulses distal to injury (vascular compromise)
- Knee dislocation - 30-40% risk of popliteal artery injury requiring emergency vascular evaluation
- Severe pain out of proportion with tense swelling (compartment syndrome)
- Inability to perform straight leg raise with palpable gap (extensor mechanism rupture)
- Complete motor or sensory loss in nerve distribution (possible nerve transection)
- Locked knee unable to extend beyond 15-20° (displaced meniscal tear)
- Open joint injury or penetrating wound near joint (infection risk)
- Expanding hematoma or uncontrolled bleeding
- Fever with severe joint swelling, warmth, inability to move (septic arthritis)
- Progressive neurological deterioration despite treatment
- Fracture-dislocation visible on imaging (requires urgent reduction)
Call 911 or go to the nearest emergency room immediately
Work Injury & Repetitive Strain

Occupational injuries affect millions of American workers annually, with construction, warehouse, and industrial workers in the Pasadena-Harris County area facing particularly high risks due to the concentration of refineries, petrochemical plants, and manufacturing facilities along the Houston Ship Channel. Work-related musculoskeletal disorders (WMSDs) account for over 30% of all workers' compensation claims in Texas, encompassing acute traumatic injuries from workplace accidents and cumulative trauma disorders from repetitive motion, forceful exertion, and awkward postures. AccidentDoc Pasadena specializes in occupational medicine, providing comprehensive evaluation, treatment, and documentation for both workers' compensation claims and personal injury cases when claims are denied. Our board-certified physicians understand the unique medical-legal requirements of occupational injuries, offering same-day appointments to ensure injured workers receive prompt care while protecting their legal rights.
Occupational injuries encompass two distinct but often overlapping categories: acute traumatic injuries resulting from specific workplace incidents, and cumulative trauma disorders (CTDs) developing gradually from repetitive exposures to biomechanical stressors. Understanding this distinction is critical for proper diagnosis, treatment, and workers' compensation claim processing.
Acute traumatic injuries involve sudden, identifiable events causing immediate tissue damage. In construction settings, these include falls from scaffolding or ladders causing fractures and spinal injuries, being struck by falling objects or equipment resulting in contusions and orthopedic trauma, caught-between accidents involving machinery causing crush injuries, and overexertion injuries from lifting or moving heavy materials causing acute lumbar strain or disc herniation. In warehouse environments, forklift accidents, falling merchandise, and acute lifting injuries predominate. Refinery and petrochemical workers face unique hazards including chemical exposures, confined space accidents, falls from elevated structures, and high-energy trauma from equipment failures. These acute injuries produce immediate symptoms, clear temporal relationships to workplace incidents, and are generally straightforward to establish as work-related under Texas workers' compensation law.
Cumulative trauma disorders develop insidiously from repeated microtrauma exceeding tissue repair capacity. Each individual exposure may be subcritical for injury, but accumulated over weeks, months, or years, the cumulative effect produces symptomatic tissue damage. Common CTDs include carpal tunnel syndrome from repetitive hand motions with wrist flexion (assembly work, computer use, tool operation), lateral epicondylitis (tennis elbow) from repetitive forearm pronation-supination with gripping (tool use, material handling), medial epicondylitis (golfer's elbow) from repetitive wrist flexion and forearm pronation (lifting, hammering), rotator cuff tendinopathy from repetitive overhead reaching (electrical work, painting, construction), De Quervain's tenosynovitis affecting thumb tendons from repetitive grasping with ulnar deviation (packaging, assembly), and chronic lumbar strain from repetitive bending, lifting, and twisting (warehouse work, construction, healthcare).
Ergonomic risk factors quantified by occupational medicine research include: Force - the amount of muscular effort required (lifting >25 lbs repeatedly increases injury risk exponentially); Repetition - cycles per minute performing similar motions (>10 repetitions per minute of the same motion significantly elevates risk); Posture - deviation from neutral anatomical positions (sustained wrist flexion >30°, shoulder abduction >60°, lumbar flexion while lifting increases tissue stress); Duration - time spent in risk positions without rest (continuous exposure >2 hours without breaks); and Vibration - exposure to hand-arm or whole-body vibration (power tool use, heavy equipment operation).
The National Institute for Occupational Safety and Health (NIOSH) has established exposure limits for various occupational activities. The NIOSH lifting equation calculates recommended weight limits based on horizontal distance, vertical distance, asymmetry, coupling, and frequency—loads exceeding calculated limits place workers at high risk for lumbar injury. The ACGIH (American Conference of Governmental Industrial Hygienists) publishes threshold limit values (TLVs) for hand activity levels correlating repetition and force with distal upper extremity disorder risk.
In Pasadena's industrial corridor, workers face compound risk factors: 12-hour shifts reduce recovery time between exposures, physically demanding work in petrochemical facilities and construction sites involves high force requirements, and production pressures may limit adequate rest breaks. Our occupational medicine approach identifies specific workplace risk factors, correlates them with clinical findings, and provides detailed causation analysis supporting workers' compensation claims or personal injury litigation when claims are wrongfully denied.
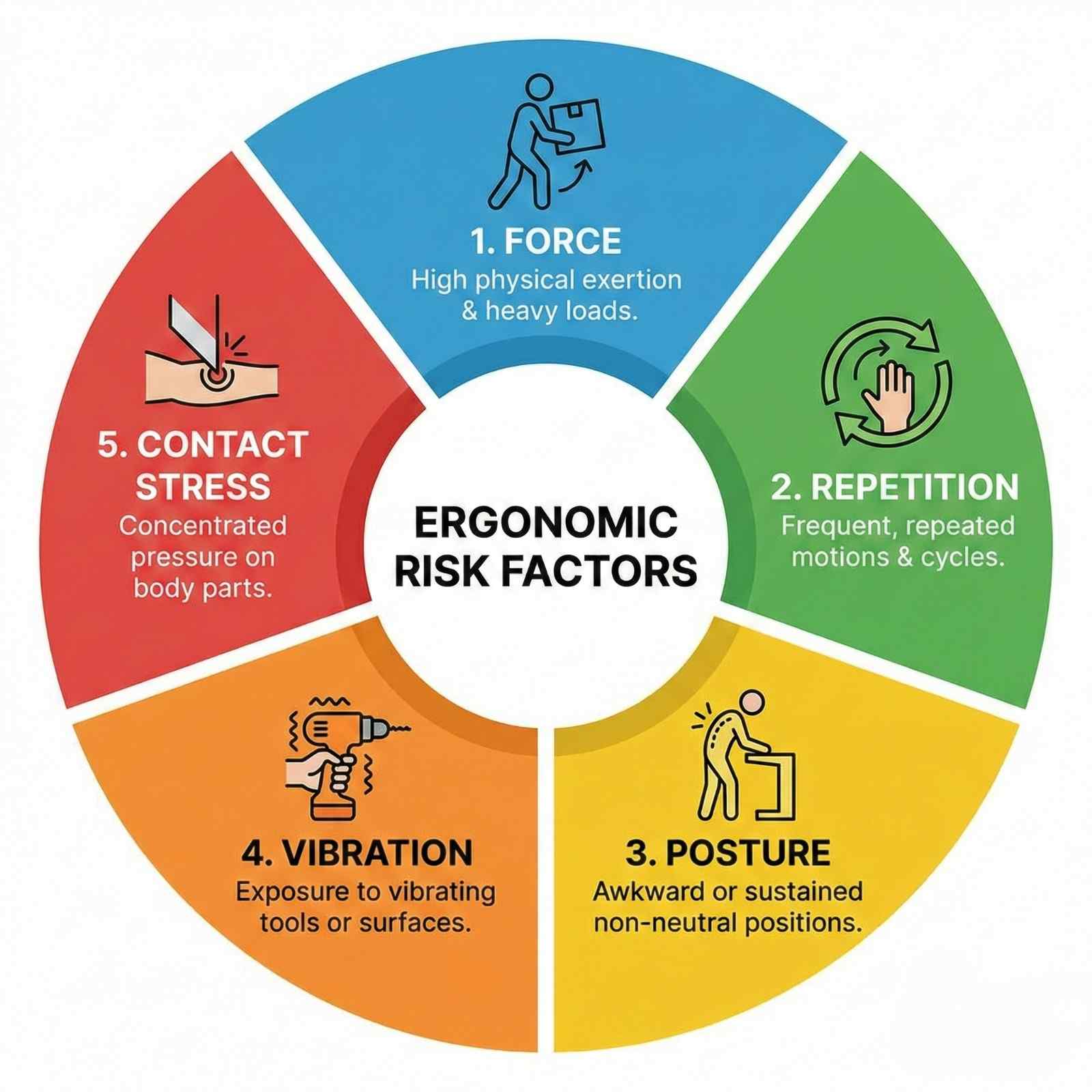
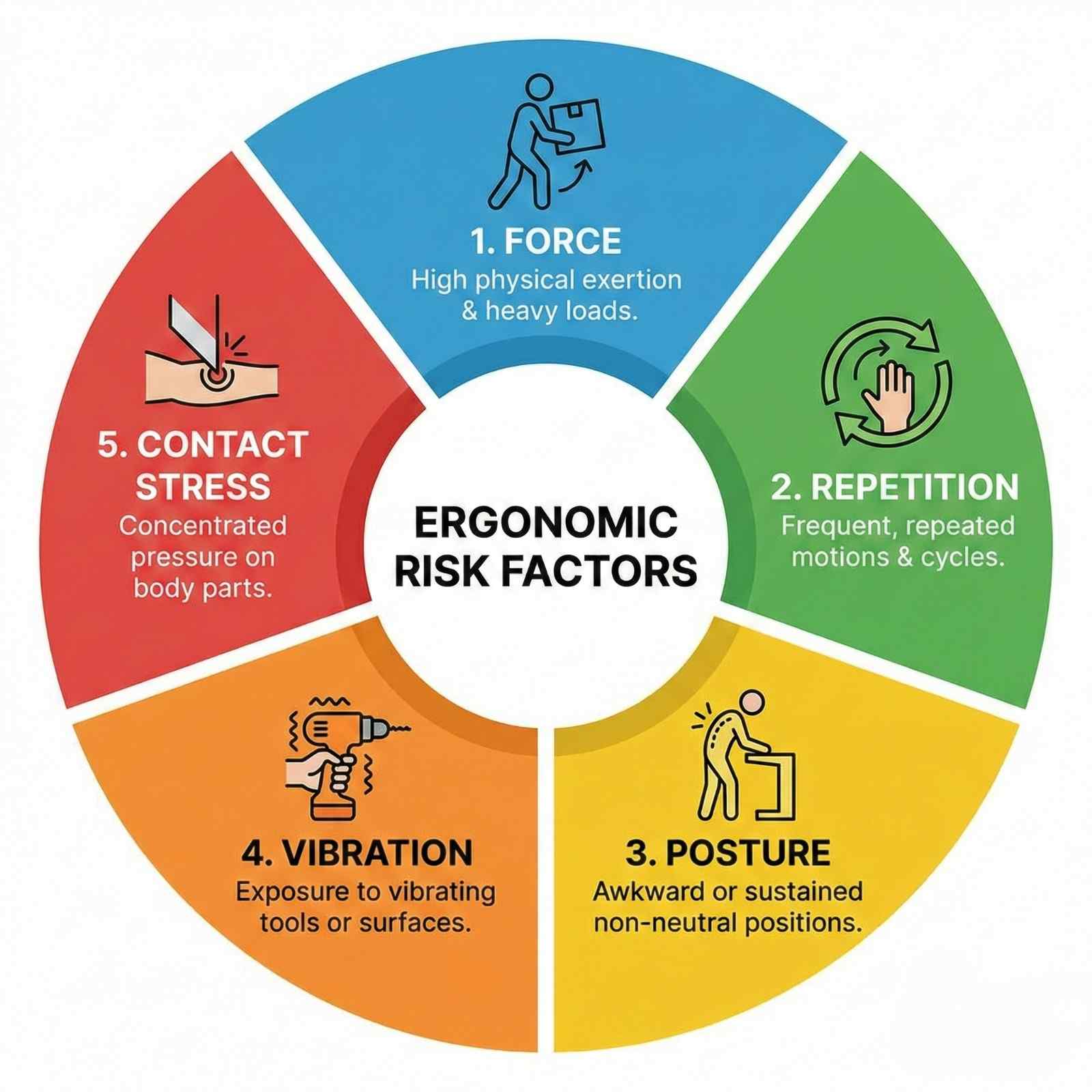
Occupational injury symptoms vary dramatically between acute traumatic injuries and cumulative trauma disorders, requiring different diagnostic approaches and treatment strategies.
Acute workplace injuries present with immediate, easily identified symptoms. Falls from heights produce sudden onset back pain, extremity pain from fractures, or head injury symptoms. Struck-by injuries cause localized pain, swelling, and bruising at impact sites. Lifting injuries typically manifest as acute low back pain with immediate onset during or within hours of lifting incident—"something snapped" or "felt something tear" are common descriptions. Caught-between injuries cause crushing trauma with severe localized pain, swelling, and often open wounds or obvious deformity.
The key diagnostic feature of acute injuries is clear temporal relationship: specific incident, immediate symptom onset, and identifiable injury mechanism. Documentation must capture: exact date and time of injury, detailed mechanism (how did it happen, what position was body in, what forces involved), immediate symptoms reported to supervisor, and any witnesses. Texas workers' compensation law requires injury reporting to employer within 30 days, though earlier reporting strengthens claims.
Cumulative trauma disorders develop insidiously, making recognition more challenging. Early symptoms include vague discomfort, achiness, or stiffness in affected regions during or after work activities. Many workers initially ignore these symptoms, attributing them to normal work fatigue or aging. As exposure continues, symptoms progress through predictable stages:
Stage 1 (Reversible): Aching and tiredness during work shifts, resolving overnight and on weekends. No functional limitations. Symptoms may persist several months. This stage is often dismissed by workers and supervisors but represents critical intervention opportunity—ergonomic modifications and early treatment can prevent progression.
Stage 2 (Reduced Work Capacity): Symptoms persist through nights and weekends. Work performance declines—reduced speed, accuracy, or endurance. Workers may develop compensatory strategies using different muscle groups or modifying techniques to avoid pain, potentially causing secondary injuries. Sleep disruption is common. Medical intervention becomes necessary. With treatment and work modifications, many patients stabilize at this stage, though complete resolution is less likely than Stage 1.
Stage 3 (Chronic/Permanent): Symptoms present at rest and during non-work activities. Unable to perform previously tolerated tasks. Significant functional limitations affecting both occupational and personal activities—difficulty with household chores, hobbies, self-care. Depression and anxiety frequently develop. Outcomes are generally poor; permanent work restrictions or disability often result. Early diagnosis and intervention are crucial to prevent reaching this stage.
Carpal tunnel syndrome (CTS), the most common work-related upper extremity disorder, presents with numbness and tingling in thumb, index, and middle fingers, worse at night. Patients often report waking at night shaking their hands to restore sensation. Daytime symptoms initially occur during provocative activities (gripping, typing, vibration exposure) but progress to constant symptoms. Thenar atrophy (wasting of thumb muscle at base of thumb) and profound weakness indicate severe, long-standing compression requiring urgent surgical decompression. Bilateral CTS suggests systemic factors (diabetes, hypothyroidism, pregnancy) or occupational exposure if symptoms correlate with work patterns.
Lateral epicondylitis (tennis elbow) causes lateral elbow pain radiating into forearm extensors. Pain worsens with gripping, tool use, and wrist extension against resistance. Simple activities like shaking hands, turning doorknobs, or lifting coffee cups become painful. Medial epicondylitis (golfer's elbow) causes medial elbow pain with wrist flexion and forearm pronation activities.
Rotator cuff tendinopathy from repetitive overhead work presents with gradual onset lateral shoulder pain, worse with overhead reaching, lifting, or sleeping on affected side. Morning stiffness improving with activity is characteristic. Progressive weakness indicates advancing from tendinopathy (inflammation) to partial-thickness tear (structural damage) to full-thickness tear (complete rupture).
Low back cumulative trauma manifests as generalized lumbar aching and stiffness after repetitive bending, lifting, or prolonged postures. Symptoms initially occur after work shifts, progressing to occur during work, then persist at rest. Radicular symptoms (leg pain, numbness, weakness) indicate nerve root involvement from disc herniation or spinal stenosis, requiring urgent evaluation. Red flags including bowel/bladder changes, saddle anesthesia, progressive weakness, or fever mandate emergency evaluation for cauda equina syndrome or infection.
De Quervain's tenosynovitis causes radial wrist pain and swelling over the thumb side of wrist, worse with thumb and wrist motion. Finkelstein's test is diagnostic: patient makes fist with thumb tucked inside fingers, then examiner ulnar deviates (bends wrist toward pinky side)—sharp pain over radial wrist confirms diagnosis.
Trigger finger causes catching or locking of affected finger during flexion-extension, often with palpable nodule in palm at base of affected finger. Initially intermittent, catching becomes constant without treatment. Patients may require using opposite hand to straighten locked finger.
Thoracic outlet syndrome from repetitive overhead work or carrying heavy loads causes arm pain, numbness, weakness, and sometimes color changes or swelling. Symptoms vary depending on whether compression affects nerves (numbness, tingling, weakness), arteries (coldness, color changes, diminished pulses), or veins (swelling, discoloration). Diagnosis is challenging, requiring EMG/NCS and sometimes vascular studies.
Chemical exposures common in Pasadena's petrochemical corridor cause additional symptoms. Dermatitis from irritants or allergens causes localized itching, redness, blisters. Respiratory symptoms from inhaled irritants include cough, wheezing, shortness of breath—may represent occupational asthma requiring pulmonary evaluation. Neurological symptoms including headache, dizziness, cognitive impairment, or peripheral neuropathy may result from neurotoxin exposures (solvents, heavy metals, organophosphates).
Documenting symptom progression is crucial for CTD claims. Workers should maintain symptom diaries recording when symptoms occur, what activities provoke them, severity ratings, and functional limitations. Medical providers must document temporal patterns, correlation with work activities, and aggravating/alleviating factors. Progressive worsening despite conservative treatment strengthens claims for advanced interventions or permanent restrictions.
Diagnosing occupational injuries requires clinical examination, strategic imaging, and often electrodiagnostic studies, combined with detailed occupational history establishing work-relatedness.
Occupational history is foundational: job title alone is insufficient—detailed understanding of actual tasks, postures, forces, and exposures is essential. Effective occupational history includes: specific tasks performed (percentage of time in each task), tools and equipment used, weights lifted (typical and maximum, frequency, technique), work postures (sitting, standing, bending, reaching overhead), cycle time (how many repetitions per minute/hour), shift length and break frequency, recent changes in work demands or processes, and use of personal protective equipment.
Job site analysis or ergonomic evaluation provides objective data. Some cases warrant job site visits with measurements of forces, repetition rates, postural demands, and workplace layout. Video recording work activities allows biomechanical analysis. These evaluations are particularly valuable for disputed CTD claims where causation is challenged.
Physical examination for upper extremity cumulative trauma focuses on identifying affected structures and provocative movements. Inspection notes muscle atrophy, swelling, or deformities. Palpation identifies tenderness along specific tendons, muscles, or nerve pathways. Range of motion testing quantifies limitations. Strength testing using manual muscle testing (0-5 scale) or dynamometry quantifies deficits. Provocative tests reproduce symptoms: Phalen's test (wrist flexion for 60 seconds reproduces CTS symptoms), Tinel's sign (tapping over median nerve at wrist produces tingling in median nerve distribution), Finkelstein's test (De Quervain's), resisted wrist extension (lateral epicondylitis), empty can test (rotator cuff).
Electrodiagnostic studies (EMG/NCS) are gold standard for diagnosing nerve compression syndromes and radiculopathies. Nerve conduction studies measure nerve signal transmission: prolonged distal latency, slowed conduction velocity, or reduced amplitude indicate nerve damage. EMG evaluates muscle electrical activity: abnormal spontaneous activity (fibrillations, positive sharp waves) indicates denervation from nerve injury. These studies objectively confirm and quantify nerve damage, critical for medical-legal documentation.
Carpal tunnel syndrome diagnosis requires median nerve conduction delay across wrist: median sensory latency >3.5ms or median motor latency >4.5ms is abnormal. Comparing median to ulnar nerve conduction in same hand improves sensitivity. Electromyography of thenar muscles shows denervation in severe cases. EMG/NCS correlation with clinical findings is essential—abnormal studies without symptoms may reflect subclinical changes or measurement error, while clinical CTS with normal studies (10-15% of cases) should still be treated based on clinical diagnosis.
Cervical or lumbar radiculopathy evaluation includes: MRI identifying nerve root compression from disc herniation, foraminal stenosis, or other pathology; EMG/NCS demonstrating specific nerve root involvement through paraspinal denervation potentials and decreased amplitude in corresponding myotome; and clinical correlation with dermatome (sensory) and myotome (motor) distribution matching imaging and electrodiagnostic findings.
Imaging studies guide diagnosis. X-rays identify bony abnormalities: fractures (acute injuries), degenerative changes (arthritis, bone spurs), and alignment problems. Ultrasound performed by experienced operators diagnoses rotator cuff tears, tendinopathy, and De Quervain's tenosynovitis dynamically and at lower cost than MRI. MRI is gold standard for soft tissue pathology: rotator cuff tears, labral tears, tendon tears, and disc herniations. CT scans excel for bony detail and surgical planning.
Laboratory testing excludes systemic conditions mimicking occupational injuries. Rheumatoid factor and anti-CCP antibodies evaluate rheumatoid arthritis. ESR and CRP assess systemic inflammation. Thyroid function (TSH) evaluates hypothyroidism causing CTS. Vitamin B12, hemoglobin A1c evaluate metabolic causes of peripheral neuropathy. Uric acid assesses gout. These tests are particularly important when bilateral symptoms, systemic symptoms, or atypical presentations suggest non-occupational etiologies.
Causation assessment integrates clinical findings with occupational exposure. Bradford Hill criteria provide framework: strength of association (high exposure correlates with high disease rates), consistency (multiple studies show same association), temporality (exposure precedes disease), dose-response relationship (increased exposure increases risk), biologic plausibility (mechanism makes scientific sense), and coherence (findings consistent across different study types). For individual cases, causation requires: documented workplace exposure to recognized risk factor, injury or condition consistent with that exposure, adequate latency (time between exposure onset and symptom development), temporal relationship (symptoms correlate with work patterns—worse during work, improve on vacation), and exclusion of non-occupational causes.
Work-relatedness documentation must address: specific ergonomic risk factors present in job (NIOSH lifting equation violations, high repetition rates, forceful exertions); comparison of patient's exposures to established occupational exposure limits; medical literature supporting that specific exposures cause diagnosed condition; and analysis of alternative explanations (pre-existing conditions, non-work activities, systemic diseases). This documentation is crucial for workers' compensation acceptance or personal injury claims when compensation is denied.
Functional capacity evaluation (FCE) objectively measures physical abilities: lifting capacity, carrying capacity, postural tolerances, and sustained work capacity. FCE results guide return-to-work decisions, establish permanent restrictions, and provide objective data for disability ratings. Physical and occupational therapists certified in FCE administration provide legally defensible evaluations.
Occupational injury treatment requires addressing both tissue pathology and causative ergonomic factors—treating symptoms without modifying workplace exposures results in symptom recurrence and treatment failure.
Acute traumatic injury management follows standard trauma protocols. Fractures require immobilization, reduction if displaced, and orthopedic referral for surgical fixation when indicated. Sprains and strains receive RICE therapy, NSAIDs, protected weight-bearing or immobilization, and progressive rehabilitation. Lacerations require wound care, tetanus prophylaxis, and sometimes surgical repair. Concussions follow return-to-work protocols similar to return-to-play in sports—cognitive rest followed by gradual return with symptom monitoring.
Cumulative trauma disorder treatment emphasizes early intervention. Stage 1 CTDs respond well to conservative measures: activity modification reducing provocative exposures, ergonomic interventions eliminating biomechanical risk factors, anti-inflammatory treatments including NSAIDs and ice, and splinting for wrist/hand conditions (wrist neutral splints for CTS, counterforce braces for epicondylitis). Many Stage 1 conditions resolve completely with these interventions, allowing continued work without restrictions.
Stage 2 CTDs require more aggressive conservative treatment: physical therapy combining manual therapy, therapeutic exercise, and modality treatments; corticosteroid injections for localized inflammatory conditions (carpal tunnel, trigger finger, epicondylitis, rotator cuff tendinopathy); work restrictions limiting provocative activities; and potential job modification or reassignment if current position cannot be safely performed despite accommodations. Treatment duration extends weeks to months. Response to treatment guides prognosis—persistent symptoms despite 3-6 months aggressive conservative care suggests surgical evaluation.
Stage 3 CTDs often require surgical intervention. Carpal tunnel release (open or endoscopic) decompresses median nerve. Trigger finger release incises constricting A1 pulley. Lateral epicondylitis debridement removes degenerative tendon tissue. Rotator cuff repair addresses tears. Early surgical intervention in Stage 3 improves outcomes compared to prolonged conservative attempts that allow progressive tissue damage.
Physical therapy is cornerstone of CTD treatment. Manual therapy including soft tissue mobilization, myofascial release, and joint mobilization addresses tissue restrictions and improves mechanics. Therapeutic exercise strengthens supporting musculature, improves endurance, and corrects biomechanical deficiencies. Postural training and body mechanics education prevent compensatory patterns. Work conditioning programs progressively increase work-relevant capacity, facilitating return to full duty.
Ergonomic interventions address root causes. Engineering controls modify workplace: adjustable workstations allowing neutral postures, mechanical assists reducing lifting forces (lift tables, hoists, forklifts), tool modifications reducing grip forces or vibration (powered tools replacing manual tools, vibration-dampening gloves), and workstation layout changes reducing reaching distances or awkward postures. Administrative controls modify work organization: job rotation limiting continuous exposure to single task, increased rest breaks allowing tissue recovery, work pace adjustments reducing repetition rates, and two-person lift policies for heavy loads. Personal protective equipment including anti-vibration gloves, wrist supports, and back belts provides last line of defense, though effectiveness varies.
Texas workers' compensation covers reasonable and necessary medical treatment. Injured workers have right to choose initial treating doctor (though insurance carriers may direct care to network providers after initial visit). Medical treatment guidelines in Texas Workers' Compensation Act establish evidence-based treatment protocols—preauthorization may be required for treatments outside guidelines. Disputes about treatment necessity, return-to-work readiness, or permanent impairment ratings can be resolved through insurance carrier appeals, Division of Workers' Compensation benefit review conferences, and contested case hearings.
When workers' compensation claims are denied (common for cumulative trauma where causation is disputed), injured workers may pursue personal injury claims against third parties or direct treatment payment. At AccidentDoc Pasadena, we offer Letter of Protection treatment for workers whose compensation claims are disputed—allowing treatment to proceed while causation litigation is resolved, with payment from settlement proceeds.
Injection therapies provide targeted treatment. Corticosteroid injections reduce inflammation in tendinopathy, bursitis, and nerve compression. Carpal tunnel injections provide temporary relief and help confirm diagnosis—significant improvement post-injection supports CTS diagnosis and predicts surgical success. Trigger finger injections often provide definitive cure, avoiding surgery. Platelet-rich plasma (PRP) injections for tendinopathy show promise in research, though evidence remains mixed and insurance coverage is limited. Prolotherapy (injection of irritant solution stimulating healing response) lacks strong evidence.
Surgical interventions for occupational injuries follow standard indications. Carpal tunnel release is indicated for severe symptoms, thenar atrophy, abnormal EMG/NCS, or symptoms unresponsive to 3-6 months conservative treatment. Endoscopic release allows faster recovery than open technique, though outcomes are equivalent long-term. Trigger finger release is simple outpatient procedure with excellent outcomes. Epicondylitis surgery (debridement of degenerative tendon tissue) is reserved for symptoms persisting >12 months despite conservative treatment. Rotator cuff repair follows guidelines discussed in joint injuries section.
Return-to-work coordination is critical. Modified duty allowing injured worker to remain employed during recovery prevents deconditioning, maintains income, and improves outcomes compared to complete work absence. Gradual return-to-work protocols start with light duty, progressively increasing demands as healing allows. Functional capacity evaluations objectively define safe work capacities, guiding restriction development. Treating physicians provide detailed restrictions: maximum lift weight, frequency of lifting, postural limitations, repetition limits, and duration restrictions. Employers must accommodate restrictions when possible—failure to provide reasonable accommodation may constitute workers' compensation retaliation or ADA violation.
Prevention is paramount. Pre-employment functional testing ensures workers have physical capacity for job demands. Early intervention programs encourage symptom reporting before injuries become severe—many employers have on-site occupational health clinics providing immediate evaluation and treatment. Ergonomic assessments identify hazardous jobs requiring modification. Safety training teaches proper lifting techniques, tool use, and hazard recognition.
Occupational injury recovery timelines vary dramatically between acute trauma and cumulative disorders, influenced by injury severity, age, comorbidities, job demands, and employer accommodation capabilities.
Acute injury recovery generally follows predictable timelines. Simple sprains and strains without complications resolve in 4-8 weeks with appropriate treatment. Moderate injuries requiring extended immobilization or limited surgical intervention need 8-16 weeks. Severe injuries with major surgery or complications may require 6-12 months. Fractures heal according to bone type and location—upper extremity fractures typically allow return to light duty at 6-8 weeks, full duty at 12-16 weeks. Lower extremity fractures affecting weight-bearing require longer disability—tibia fractures may need 12-24 weeks before unrestricted work.
Return-to-work after acute injury follows progressive phases: Phase 1 (weeks 0-2): Complete work restriction while acute symptoms managed, immobilization/protection of injured part. Phase 2 (weeks 2-6): Modified duty begins with significant restrictions—sedentary or light duty only, frequent position changes, no use of injured extremity for primary job functions. Phase 3 (weeks 6-12): Progressive return to full duty with gradually reduced restrictions as healing progresses and functional capacity improves. Phase 4 (week 12+): Unrestricted full duty work when healing complete, strength restored, and functional capacity meets job demands.
Cumulative trauma disorder recovery is less predictable. Stage 1 CTDs caught early may resolve completely in 4-8 weeks with ergonomic modifications and conservative treatment, allowing unrestricted return to work. Stage 2 CTDs typically require 3-6 months treatment, often necessitating permanent work restrictions or job modifications to prevent recurrence—many patients achieve symptom control allowing continued work but not complete cure. Stage 3 chronic CTDs have poor recovery prospects—even with surgery and aggressive rehabilitation, many patients require permanent significant restrictions or work disability.
Return-to-work after CTD treatment must address causative factors. Returning to identical job conditions without modifications guarantees symptom recurrence. Successful return requires: ergonomic modifications eliminating biomechanical risk factors, work restrictions matching functional capacity and preventing symptom exacerbation, graduated return-to-work increasing exposure progressively while monitoring symptom response, and long-term monitoring with periodic reassessment.
Work restrictions for CTDs are highly job-specific. Common restrictions include: lifting limitations (maximum weight, frequency, technique requirements—5-10 lbs occasionally vs frequently, floor-to-waist vs overhead), postural restrictions (minimize repetitive bending, overhead reaching, sustained awkward postures), repetition limits (vary tasks every 20-30 minutes, frequent microbreaks), tool use restrictions (avoid high-vibration tools, forceful gripping), and duration limits (4-6 hour shifts initially progressing to 8-10 hours as tolerated).
Modified duty job descriptions must be detailed and specific, addressing: primary job functions and percentage of time on each task, physical demands (lifting, carrying, pushing, pulling with specific weights and frequencies), environmental conditions, tools and equipment used, and postural requirements. This specificity prevents misunderstandings and allows treating physicians to determine if proposed modified duty is medically appropriate.
Carpal tunnel syndrome recovery post-surgery: weeks 0-2 post-release involve bandage and light activity restriction—typing and light grasping permitted, no heavy lifting. Weeks 2-6: progressive strengthening, return to normal daily activities. Months 2-3: return to full duty work for most jobs. Manual labor positions may require 3-4 months. Symptom improvement is often immediate post-surgery (relief of numbness), but strength and endurance return gradually. 90% of patients achieve good-to-excellent outcomes with carpal tunnel release.
Trigger finger recovery post-release is rapid: 2-3 weeks restricted use, then gradual return to activities. Full recovery typically by 6-8 weeks. Outcomes are excellent with low recurrence rates.
Rotator cuff repair recovery for occupational injuries: protective phase (0-6 weeks) with sling immobilization, passive range of motion only, no return to work. Progressive mobilization phase (6-12 weeks): active motion begins, light duty office work may resume. Strengthening phase (12-20 weeks): progressive resistance training, light-moderate duty work. Return to full duty (20-24 weeks): for non-manual labor. Heavy manual labor requires 6-9 months minimum.
Lumbar injury recovery varies by pathology. Acute lumbar strain without disc herniation or radiculopathy: 2-4 weeks complete or modified duty, then progressive return. Disc herniation with radiculopathy: 6-12 weeks conservative management before considering surgery. Post-discectomy: 4-6 weeks restricted duty, 8-12 weeks return to full duty for sedentary work, 12-24 weeks for heavy manual labor.
Maximum medical improvement (MMI) occurs when condition has stabilized and further improvement is not expected with additional treatment. For acute injuries, MMI typically occurs when healing is complete—3-6 months for most injuries. For CTDs and surgical repairs, MMI may take 12-24 months. Reaching MMI triggers permanent impairment rating.
Permanent impairment ratings quantify lasting functional deficits. Texas workers' compensation uses AMA Guides to the Evaluation of Permanent Impairment, 4th Edition (unlike most states using 6th Edition). Ratings consider: anatomic loss or loss of use, loss of range of motion, pain and sensory deficits, functional loss, and need for ongoing treatment. Upper extremity ratings convert to whole person impairment: shoulder 60%, elbow 70%, wrist 60%, hand 90%, thumb 40%. Impairment ratings determine compensation for permanent partial disability—workers receive weekly benefits for specified number of weeks based on rating.
Disputes about MMI, impairment ratings, or return-to-work capacity frequently occur. Independent medical examinations (IME) by insurance-selected doctors often conclude earlier MMI and lower ratings than treating physicians—creating adversarial situations. Designated doctor examinations by Division-selected neutral physicians resolve disputes, with designated doctor opinions given presumptive weight.
Vocational factors influence outcomes. Younger workers with transferable skills and higher education have better employment outcomes even with permanent restrictions. Older workers in manual labor positions with limited education face poor prospects when permanent significant restrictions prevent return to pre-injury work—vocational rehabilitation, job retraining, or permanent disability may result.
Psychological factors significantly impact recovery. Depression, anxiety, fear-avoidance behaviors, pain catastrophizing, and litigation stress worsen outcomes. Multidisciplinary treatment addressing psychological factors improves functional outcomes beyond physical treatments alone. Cognitive-behavioral therapy, acceptance and commitment therapy, and motivational interviewing show efficacy in chronic pain and work disability.
Secondary gain complicates some cases. Financial incentives (workers' compensation benefits, disability benefits, litigation settlements) may unconsciously influence symptom reporting and treatment response. Symptom magnification or malingering occurs but is far less common than insurance companies suggest. Most injured workers strongly desire return to productivity. Objective testing including FCE, repeat examination for consistency, and correlation of complaints with examination findings help identify exaggeration.
Comprehensive medical-legal documentation is critical for occupational injury claims, as workers' compensation disputes about causation, treatment necessity, work-relatedness, and permanent impairment are common. AccidentDoc Pasadena provides detailed documentation supporting both workers' compensation claims and personal injury litigation when claims are wrongfully denied.
Initial injury report documentation establishes temporal relationship and work-relatedness: "Patient presented [DATE], [X] days after workplace injury occurring [DATE] at [EMPLOYER] where patient works as [JOB TITLE]. Injury occurred when [DETAILED MECHANISM]: patient was [SPECIFIC TASK] when [SPECIFIC EVENT] resulting in [INJURY]. Injury was immediately reported to supervisor [NAME] on [DATE]. Patient has worked at [EMPLOYER] for [X] years in this position without prior injury to this body part. Past medical history per records review shows no prior treatment for [BODY PART] conditions."
For acute injuries, detailed mechanism documentation establishes causation and injury severity: "Patient works as warehouse associate performing order fulfillment. On [DATE] at approximately [TIME], patient was lifting 50-lb box of merchandise from floor to conveyor belt. Box unexpectedly shifted causing sudden twisting motion while in flexed position. Patient immediately experienced severe low back pain with radiation into right leg. Unable to continue work duties. Coworker [NAME] witnessed incident. Injury mechanism—sudden asymmetric loading with flexion and rotation—is biomechanically consistent with lumbar disc herniation."
For cumulative trauma disorders, causation documentation requires detailed exposure analysis: "Patient works as assembly line worker at [EMPLOYER] for 8 years. Job duties require repetitive forceful gripping of pneumatic screwdriver for 85% of 10-hour shifts, performing approximately 400 screw-driving operations per hour (6.7 per minute) with forceful grip requiring estimated 15-20 lbs grip force. Wrist maintained in flexed position 30-40° during tool operation. No microbreaks provided; 30-minute lunch and two 15-minute breaks during 10-hour shift. These exposures exceed ACGIH threshold limit values for hand activity level and constitute high-risk ergonomic factors for carpal tunnel syndrome development. Ergonomic assessment performed [DATE] by certified ergonomist [NAME] documented these exposures (report attached). Patient developed bilateral hand numbness and tingling approximately 2 years ago, progressively worsening over time. Right hand symptoms significantly worse than left, correlating with right-hand dominant tool use. Symptoms worse during work shifts, partially improving on weekends. No non-occupational exposures or systemic conditions (diabetes, hypothyroidism, rheumatoid arthritis) identified. Clinical examination and electrodiagnostic studies confirm bilateral carpal tunnel syndrome, with right greater than left corresponding to exposure pattern."
Examination documentation must quantify objective findings: "Physical examination reveals [SPECIFIC FINDINGS]: tenderness to palpation over [LOCATION], swelling measuring [X cm], ecchymosis [DESCRIPTION], deformity [DESCRIPTION]. Range of motion: [SPECIFIC DEGREES for each plane]. Strength testing: [SPECIFIC MUSCLE GROUPS with 0-5 grade]. Neurological examination: sensation [DERMATOME FINDINGS], reflexes [SPECIFIC REFLEXES with +/++/+++/++++]. Special tests: [TEST NAME] positive, [TEST NAME] negative. Functional limitations observed during examination: unable to [SPECIFIC ACTIVITY], compensatory movements when attempting [ACTIVITY]."
Diagnostic test correlation: "X-rays performed [DATE] demonstrate [SPECIFIC FINDINGS with measurements]. MRI performed [DATE] shows [DETAILED PATHOLOGY with location, size, severity]. EMG/NCS performed [DATE] by Dr. [NAME] reveals [SPECIFIC NERVE CONDUCTION ABNORMALITIES with latencies, velocities, amplitudes]. These objective findings confirm clinical diagnosis of [CONDITION] and establish severity as [MILD/MODERATE/SEVERE]."
Treatment documentation justifies medical necessity: "Treatment plan: (1) Work restrictions—no lifting >10 lbs, limited standing to 2 hours per shift, frequent position changes, no repetitive bending. (2) Physical therapy 3x weekly for 6 weeks focusing on [SPECIFIC INTERVENTIONS]. (3) NSAIDs—ibuprofen 600mg TID for 4 weeks. (4) Follow-up in 2 weeks. If symptoms persist despite conservative management, consider MRI and specialist referral. Treatment goals: reduce pain to allow function, restore strength and range of motion, prevent chronic disability, return to work capacity."
Progress note documentation tracks treatment response: "Patient returns for Week 4 follow-up. Compliance: attended 10/12 PT sessions, taking medications as prescribed, following restrictions (confirmed with employer). Subjective: pain decreased from 8/10 to 5/10, sleeping better. Objective: ROM improved—flexion increased 20°, strength 3/5 to 4-/5. Functional improvements: can now [SPECIFIC ACTIVITY]. Assessment: moderate improvement with conservative treatment. Plan: continue current treatment plan, progress PT intensity, follow-up in 4 weeks."
When treatment plateaus or fails: "Patient has received 6 months conservative management including 24 PT sessions, two corticosteroid injections, trial of multiple NSAIDs, and work restrictions. Despite this aggressive non-operative treatment, patient demonstrates persistent significant symptoms: pain 6/10, functional limitations preventing [JOB DUTIES], objective examination shows [PERSISTENT FINDINGS]. MRI confirms [STRUCTURAL PATHOLOGY]. Conservative treatment has failed to restore function. Surgical consultation with Dr. [ORTHOPEDIST] obtained [DATE]—recommends [SURGICAL PROCEDURE]. Surgery is medically necessary to address structural pathology and restore work capacity."
Causation statements for workers' compensation: "Within a reasonable degree of occupational medicine certainty, this patient's [CONDITION] is causally related to workplace exposures at [EMPLOYER]. Causation is established by: (1) Documented exposure to recognized ergonomic risk factors (detailed in occupational exposure analysis above) exceeding established threshold limits. (2) Temporal relationship—symptom onset correlating with work pattern. (3) Dose-response relationship—symptoms worse during high-exposure periods, partial improvement with reduced exposure (weekends/vacations). (4) Absence of alternative explanations—no systemic diseases, non-occupational exposures, or pre-existing conditions explaining symptoms. (5) Consistency with medical literature establishing [SPECIFIC EXPOSURES] cause [CONDITION]. (6) Objective confirmation on clinical examination and diagnostic testing. This injury arose out of and in the course of employment at [EMPLOYER]."
Work capacity evaluation: "Patient's current work capacity based on functional examination, objective testing, and clinical judgment: Maximum lift 15 lbs occasionally (5% of workday), 10 lbs frequently (33% of workday). No overhead reaching. No sustained awkward postures. No repetitive gripping >2 lbs force. No high-vibration tool use. Can sit continuously 30 minutes, stand 20 minutes, walk 15 minutes before position change required. These restrictions are permanent [or temporary pending further treatment/healing]. Current restrictions prevent performance of pre-injury job duties which require [SPECIFIC DEMANDS]. Modified duty or alternate position necessary."
Permanent impairment rating at MMI: "Patient reached Maximum Medical Improvement on [DATE], [X] months post-injury. Residual impairments include: loss of range of motion ([SPECIFIC MEASUREMENTS]), strength deficit ([SPECIFIC GRADES]), sensory deficits ([DISTRIBUTION]), functional limitations ([SPECIFIC ACTIVITIES]). Using AMA Guides to the Evaluation of Permanent Impairment, 4th Edition, Chapter [X], Table [X]: [CALCULATION METHOD] = [X]% upper extremity impairment which converts to [Y]% whole person impairment using Table [X]. Permanent restrictions: [SPECIFIC RESTRICTIONS]. These impairments directly result from work injury of [DATE] and are permanent."
When claims are denied and personal injury litigation is pursued: "Patient's workers' compensation claim was denied by carrier [CARRIER NAME] on [DATE] based on assertion injury is not work-related [or other stated reason]. I disagree with carrier's determination based on [SPECIFIC MEDICAL EVIDENCE contradicting denial basis]. Alternatively, if injury is determined to have resulted from third-party negligence or employer intentional conduct, patient pursues personal injury claim. My opinions regarding causation, treatment necessity, and permanent impairment are unchanged regardless of whether proceeding under workers' compensation or tort claim."
Seek Emergency Care Immediately If You Experience:
- Progressive hand weakness or rapidly developing thenar atrophy
- Bilateral leg symptoms with saddle anesthesia or bowel/bladder changes
- Progressive foot drop or leg weakness worsening daily
- Severe pain out of proportion to findings - possible CRPS
- Infection signs after injections or surgery - fever, redness, increasing pain
- Compartment syndrome after crush injury - severe pain with passive stretch
- Constant numbness or fixed weakness not improving over 4-8 weeks
- Chemical exposure with respiratory or neurological symptoms
Call 911 or go to the nearest emergency room immediately
Need Treatment for Your Injuries?
Don't wait for your injuries to worsen. Get same-day evaluation and treatment from our accident injury specialists. We accept Letter of Protection—$0 out of pocket until your case settles.

Whiplash is the most common injury resulting from car accidents, affecting over 3 million Americans annually. This cervical spine injury occurs when sudden deceleration causes the head to rapidly move forward and backward, straining the delicate muscles, ligaments, and vertebrae in the neck. At AccidentDoc Pasadena, our board-certified physicians specialize in comprehensive whiplash treatment, from initial diagnosis through complete recovery.
Whiplash is a complex soft tissue injury involving the cervical spine's intricate network of seven vertebrae (C1-C7), intervertebral discs, facet joints, muscles, ligaments, and nerve roots. The injury mechanism typically involves a hyperextension-hyperflexion sequence: during rear-end collisions, the torso is thrust forward by the seatback while the head momentarily remains stationary due to inertia. This creates an S-shaped curve in the cervical spine, straining the anterior longitudinal ligament and anterior neck muscles. Milliseconds later, the head snaps forward into hyperflexion, overstretching the posterior ligaments, facet joint capsules, and paraspinal muscles.
The forces involved can exceed 5G of acceleration, causing microscopic tears in muscle fibers, ligament strains, facet joint capsule injuries, and in severe cases, intervertebral disc damage or nerve root compression. The C5-C6 and C6-C7 spinal segments bear the greatest stress due to their location at the cervical spine's mobile center. Research published in the Journal of Orthopaedic & Sports Physical Therapy demonstrates that even low-speed collisions (5-10 mph) can generate sufficient force to cause whiplash, as the sudden acceleration-deceleration exceeds the neck's protective muscle contraction response time.
What makes whiplash particularly challenging is its biomechanical complexity. Unlike a simple muscle strain, whiplash often involves multiple tissue types simultaneously: muscle-tendon units, ligamentous structures, facet joint capsules, and sometimes disc integrity. The injury cascade doesn't stop at the moment of impact—inflammatory mediators released by damaged tissues can sensitize nerve endings, leading to chronic pain if left untreated. Our team at AccidentDoc Pasadena employs advanced diagnostic protocols to identify all involved structures, ensuring comprehensive treatment rather than symptomatic relief alone.
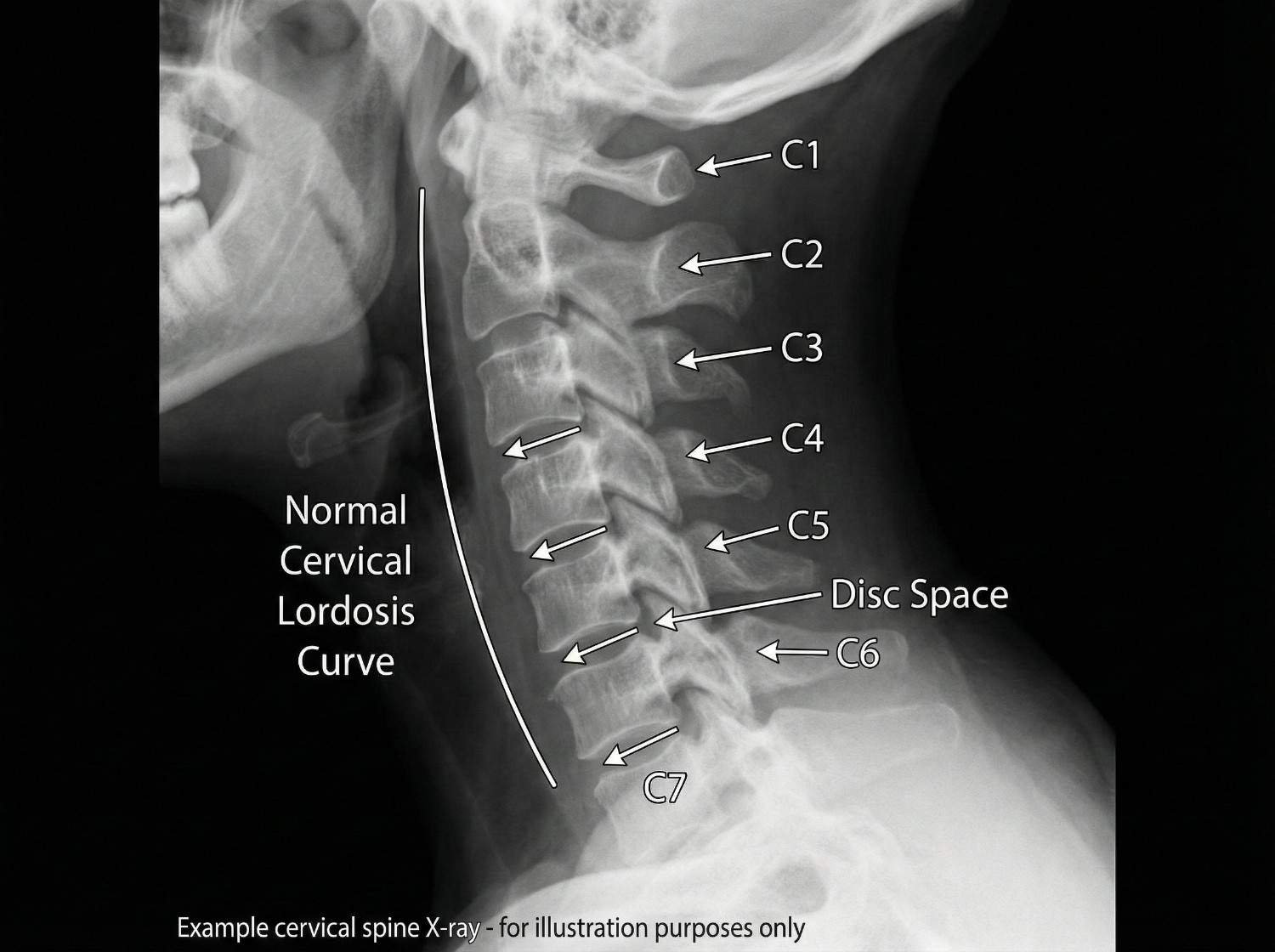
Rear-end collisions account for approximately 80% of all whiplash injuries, making them the leading cause by a substantial margin. These accidents generate the classic hyperextension-hyperflexion mechanism as the struck vehicle rapidly accelerates forward while the occupant's head lags behind. Even at seemingly minor speeds of 5-15 mph, the force differential between vehicle acceleration and head inertia creates significant cervical strain. Side-impact collisions represent the second most common cause, producing lateral whiplash where the head is thrown sideways, straining the scalene muscles and contralateral facet joints.
Frontal collisions, while often associated with more severe injuries, also cause whiplash through a hyperflexion-hyperextension sequence—the reverse of rear-end impacts. Here, the head initially snaps forward (hyperflexion) before rebounding backward (hyperextension). Pedestrian-vehicle collisions generate particularly severe whiplash as the unrestrained pedestrian experiences full-body acceleration without seatbelt protection, often resulting in rotational head movements that combine flexion, extension, and lateral forces simultaneously.
Less common but significant causes include slip-and-fall accidents where the head snaps backward upon impact, sports injuries involving helmet-to-helmet contact or sudden deceleration (football, hockey, rugby), and workplace accidents such as being struck by falling objects or equipment. Even aggressive amusement park rides with rapid acceleration-deceleration cycles have been documented as whiplash causes. The common denominator across all mechanisms is sudden, forceful neck movement that exceeds the cervical spine's physiological range of motion before protective muscle reflexes can activate.
In Pasadena and the greater Houston area, 18-wheeler accidents on Highway 225 and I-45 produce particularly severe whiplash injuries due to the massive size differential between commercial trucks and passenger vehicles. The forces generated in these collisions often result in Grade 2 or Grade 3 whiplash (moderate to severe) with associated complications like disc herniations or radiculopathy.
- Rear-end collisions (80% of cases) - classic hyperextension-hyperflexion
- Side-impact accidents - lateral whiplash with scalene muscle strain
- Frontal collisions - reverse mechanism with airbag forces
- Pedestrian accidents - rotational forces without restraint
- Slip-and-fall with head snap - hyperextension dominant
- 18-wheeler accidents - high-force impacts with severe tissue damage
Whiplash symptoms follow a characteristic temporal pattern that clinicians use to assess injury severity and predict outcomes. Immediate symptoms (0-6 hours post-injury) include neck stiffness, reduced cervical range of motion particularly in rotation and extension, muscle spasms palpable in the paraspinal muscles, and localized pain at the injury site. These acute symptoms reflect the initial inflammatory response and protective muscle guarding. Many patients report feeling "fine" immediately after the accident, only to develop severe symptoms hours later as inflammatory mediators accumulate and muscle spasms intensify.
Delayed symptoms (24-72 hours post-injury) are hallmark features of whiplash and include cervicogenic headaches originating from the occipital region and radiating forward, upper back pain between the shoulder blades (thoracic paraspinal muscle involvement), shoulder pain from muscle strain and referral patterns, dizziness or vertigo from cervical proprioceptor dysfunction, TMJ pain from jaw clenching during impact, and cognitive difficulties like concentration problems or mental fog. This delayed onset occurs because tissue inflammation peaks 24-48 hours after injury, and microscopic muscle tears don't produce pain until inflammatory swelling develops.
Chronic symptoms (persisting beyond 3 months) develop in approximately 50% of whiplash patients without proper treatment and indicate transition to chronic whiplash-associated disorder (WAD). These include persistent neck pain with activity-related flares, radicular symptoms like arm numbness, tingling, or weakness indicating nerve root compression from disc herniation or foraminal stenosis, chronic headaches often refractory to over-the-counter medications, reduced cervical mobility with measurable range of motion deficits, sleep disturbances from pain-related arousals, and psychological symptoms including anxiety about driving or chronic pain-related depression.
The Quebec Task Force Classification System grades whiplash severity from I (neck pain without objective findings) to IV (neck pain with fracture or dislocation). Grade II injuries (neck pain with musculoskeletal signs) represent the majority of cases we treat at AccidentDoc Pasadena. Early intervention within the first 72 hours significantly improves outcomes, which is why we offer same-day appointments for accident victims.

| Symptom | Timing / Description |
|---|---|
| Neck stiffness and pain | Immediate (0-6 hours) |
| Reduced range of motion | Immediate (0-6 hours) |
| Cervicogenic headaches | Delayed (24-72 hours) |
| Shoulder/upper back pain | Delayed (24-72 hours) |
| Arm numbness/weakness | Delayed or Chronic |
| Dizziness or vertigo | Delayed (24-72 hours) |
| TMJ pain | Delayed (24-72 hours) |
| Cognitive difficulties | Delayed or Chronic |
| Chronic pain with flares | Chronic (>3 months) |
| Sleep disturbances | Chronic (>3 months) |
Accurate whiplash diagnosis requires a systematic approach combining clinical examination with appropriate imaging studies. Our evaluation begins with a detailed medical history documenting accident mechanism, time to symptom onset, symptom progression, and any neurological symptoms. This information guides the physical examination and imaging selection.
Physical examination assesses multiple cervical spine parameters: active and passive range of motion measurement in six planes (flexion, extension, right/left rotation, right/left lateral flexion) using inclinometry or goniometry for objective documentation. We palpate all cervical vertebrae (C1-C7) for point tenderness, assess paraspinal muscle tone and spasm severity, and examine facet joint tenderness with pressure over the lateral masses. Neurological testing includes deep tendon reflexes (biceps C5, brachioradialis C6, triceps C7), sensory examination in all dermatomes, and manual muscle testing for myotomal weakness. Spurling's test (cervical compression with rotation and extension) reproduces radicular symptoms if nerve root compression exists.
Imaging studies are selected based on clinical presentation: Standard cervical X-rays (AP, lateral, open-mouth odontoid) are initial studies to rule out fractures, assess vertebral alignment, measure cervical lordosis, and evaluate disc space heights. While X-rays don't visualize soft tissues, they identify bony abnormalities and instability. MRI (magnetic resonance imaging) is the gold standard for soft tissue evaluation, revealing disc herniations, ligament tears (especially the alar and transverse ligaments at C1-C2), facet joint effusions indicating capsule injury, spinal cord signal changes, and nerve root compression. We order MRI when neurological symptoms exist, severe pain persists beyond 4-6 weeks, or clinical examination suggests disc or ligament injury.
CT scanning provides superior bony detail and is reserved for suspected fractures not visible on X-ray, especially C1-C2 injuries or facet fractures. Electrodiagnostic studies (EMG/NCS - electromyography/nerve conduction studies) performed 3-4 weeks post-injury can confirm radiculopathy when MRI findings are equivocal, differentiating nerve root injury from peripheral nerve entrapment.
Functional capacity evaluations objectively measure how whiplash affects daily activities, providing documentation for personal injury claims and return-to-work decisions. This comprehensive diagnostic approach ensures we identify all injury components, enabling targeted treatment rather than generic neck pain management.
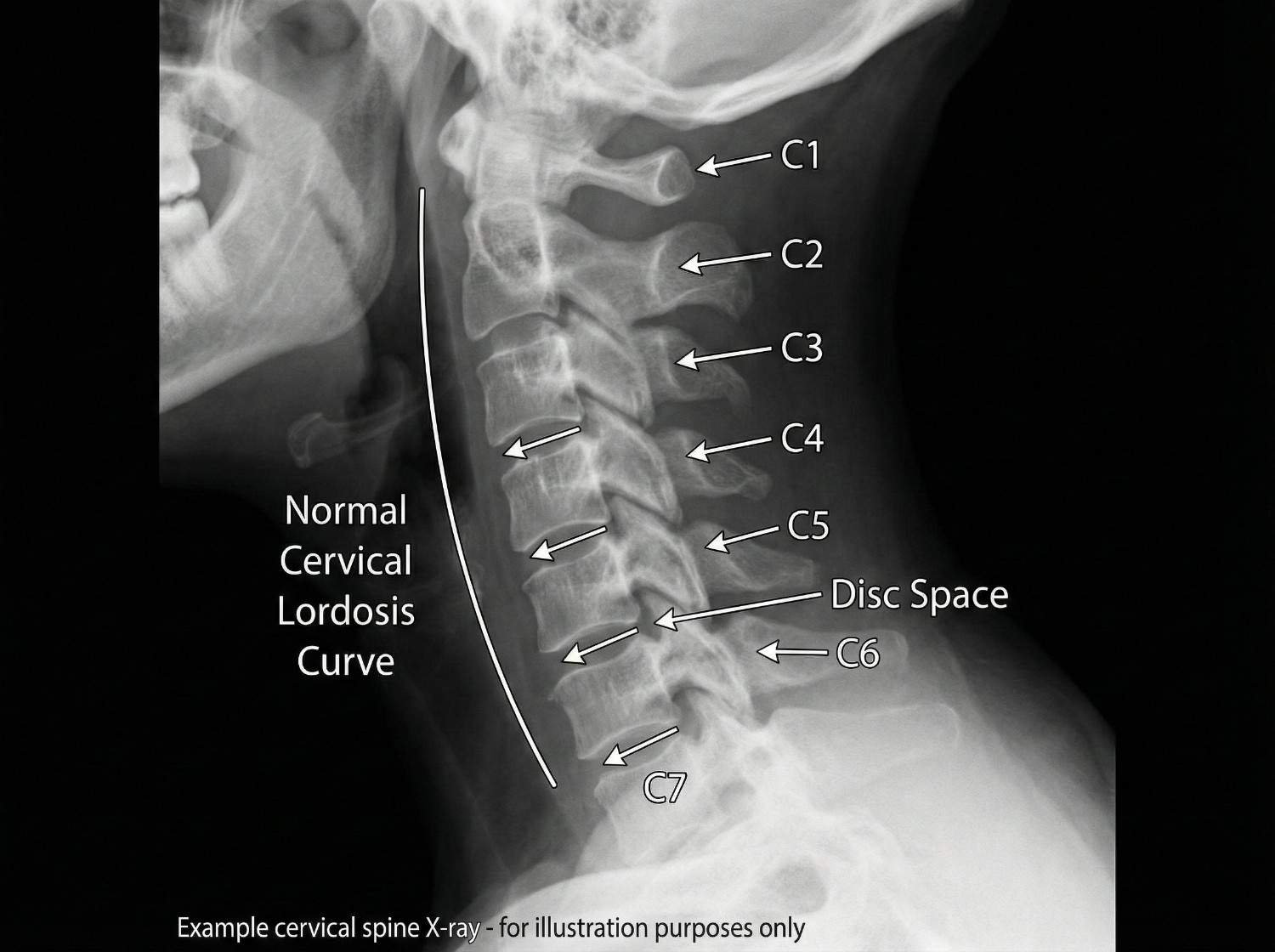

AccidentDoc Pasadena employs evidence-based treatment protocols progressing through four phases based on injury severity and patient response. All treatment is available through Letter of Protection, meaning $0 out-of-pocket cost until your case settles.
Phase 1 (Acute: Days 1-14) focuses on pain control and inflammation reduction. We prescribe NSAIDs (nonsteroidal anti-inflammatory drugs) like ibuprofen or naproxen to reduce inflammation and pain. Muscle relaxants such as cyclobenzaprine or tizanidine address muscle spasms. Ice application (15-20 minutes every 2-3 hours) reduces inflammation in the first 48-72 hours, then alternating ice/heat improves muscle relaxation. Soft cervical collars are used judiciously for 3-5 days maximum, as prolonged use causes muscle deconditioning. We emphasize active recovery over immobilization, encouraging gentle range of motion within pain tolerance.
Phase 2 (Subacute: Weeks 2-8) introduces active rehabilitation. Physical therapy includes cervical stretching exercises (chin tucks, corner stretches), progressive strengthening of deep neck flexors and stabilizers, postural training to correct forward head posture common in whiplash patients, and manual therapy including soft tissue mobilization. Chiropractic care with gentle cervical adjustments restores normal joint mobility, particularly at C5-C6 and C6-C7 where restriction commonly occurs. We use flexion-distraction techniques and activator methods rather than high-velocity rotational manipulation in acute whiplash. Massage therapy addresses myofascial trigger points in upper trapezius, levator scapulae, and suboccipital muscles that develop secondary to initial injury.
Phase 3 (Intermediate: Weeks 8-16) employs interventional procedures for patients not achieving adequate relief from conservative care. Trigger point injections deliver local anesthetic and sometimes corticosteroid to hyperactive muscle knots, providing immediate pain relief and allowing progression of physical therapy. Facet joint injections target the cervical zygapophyseal joints with fluoroscopically-guided anesthetic and steroid, diagnostic and therapeutic for facet-mediated pain. Medial branch blocks anesthetize the nerves supplying facet joints; positive response (>80% pain relief) predicts success with radiofrequency ablation for long-term pain control. Epidural steroid injections address cervical radiculopathy from disc herniation or foraminal stenosis, delivering anti-inflammatory medication directly to the inflamed nerve root.
Phase 4 (Surgical: Rarely Needed) is reserved for severe cases with progressive neurological deficits, confirmed structural pathology (large disc herniation compressing spinal cord or nerve root), or failure of 6+ months of comprehensive conservative care. Anterior cervical discectomy and fusion (ACDF) removes herniated disc material and fuses adjacent vertebrae, reliably decompressing neural structures. Artificial disc replacement preserves motion at the surgical level, potentially reducing adjacent segment degeneration. Surgical intervention is appropriate for less than 5% of whiplash patients; our goal is always maximum recovery through non-surgical means.
Our treatment selection is individualized based on Quebec Task Force Classification, presence of radiculopathy, patient functional goals, and response to initial interventions. We provide comprehensive documentation for your attorney including causation analysis, treatment plans, and prognosis statements.


Acute Phase (Days 1-14)
1-2 weeksPain control, inflammation reduction, gentle mobility. NSAIDs, muscle relaxants, ice/heat therapy, soft collar (3-5 days max). Active recovery emphasis.
Subacute Phase (Weeks 2-8)
2-8 weeksActive rehabilitation with physical therapy, chiropractic adjustments, massage therapy. Progressive strengthening, range of motion restoration, postural correction.
Intermediate Phase (Weeks 8-16)
8-16 weeksInterventional procedures for persistent pain. Trigger point injections, facet joint injections, medial branch blocks, epidural steroid injections.
Surgical Phase (If Needed)
Case dependentReserved for progressive neurological deficits or failed conservative care. ACDF or artificial disc replacement. Less than 5% of cases.
Whiplash recovery follows predictable patterns correlated with injury severity, though individual variability exists based on age, pre-existing conditions, accident biomechanics, and treatment compliance. Understanding expected recovery timelines helps patients maintain realistic expectations and adhere to treatment protocols.
Grade 1 whiplash (neck pain without objective musculoskeletal signs) typically resolves in 6-12 weeks with conservative care. These patients experience complete functional recovery and return to pre-injury activities without restrictions. Pain decreases progressively with occasional minor flares during physical therapy progression.
Grade 2 whiplash (neck pain with musculoskeletal signs like restricted range of motion or point tenderness) requires 3-6 months for substantial recovery. Most patients achieve 80-90% improvement by 3 months with appropriate treatment, with residual symptoms manageable through self-care. Return to work occurs at 4-8 weeks depending on job demands—sedentary work earlier than labor-intensive positions. Functional capacity evaluations at 8-12 weeks objectively document work capabilities.
Grade 3 whiplash (neck pain with neurological signs including radiculopathy or cord compression) demands 6-12+ months for recovery, with some patients experiencing permanent limitations. Neurological recovery progresses slower than musculoskeletal healing; nerve regeneration occurs at approximately 1mm per day. Patients with confirmed nerve root compression may require 4-6 months to regain normal strength and sensation even after successful treatment. A subset develops chronic whiplash-associated disorder (WAD) with persistent symptoms beyond 6 months, requiring ongoing pain management and functional restoration.
Factors predicting prolonged recovery include high initial pain intensity (VAS >6/10), rapid onset of symptoms (<24 hours), presence of radicular symptoms, older age (>40 years), female gender (smaller neck musculature provides less protection), pre-existing cervical degenerative changes, rear-end collision mechanism, and delayed treatment initiation (>72 hours post-injury). Conversely, early mobilization, compliance with physical therapy, psychological resilience, and prompt treatment access predict favorable outcomes.
Recovery milestones we monitor include pain reduction (50% improvement by 4-6 weeks), range of motion improvement (within 10% of normal by 8 weeks), functional capacity (return to daily activities by 8-12 weeks), and return to work (light duty by 4-6 weeks, full duty by 8-16 weeks for most occupations). Our treatment approach accelerates progress through these milestones while preventing chronic pain development through comprehensive care addressing all injury components.
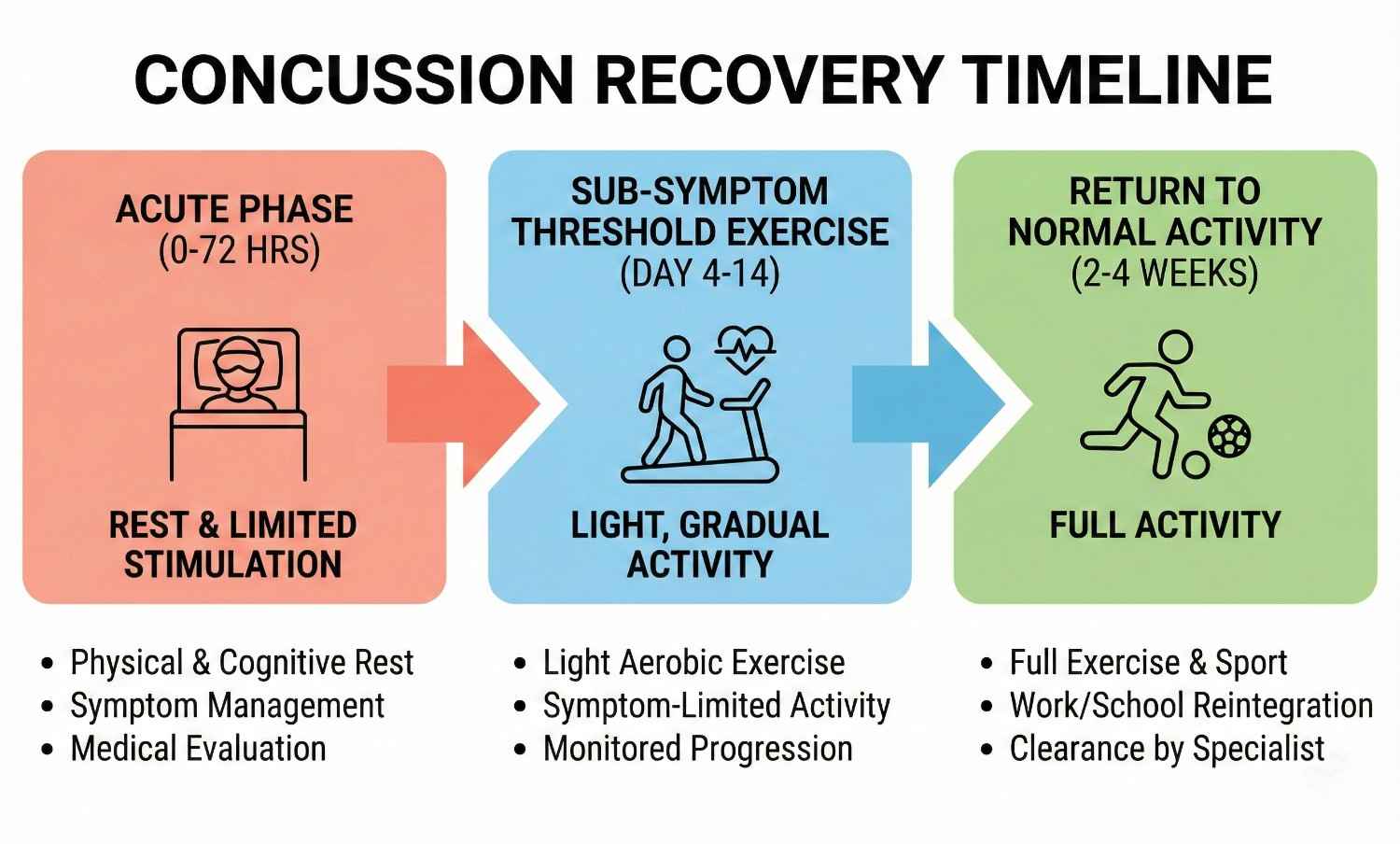
Comprehensive medical documentation is crucial for personal injury claims, insurance negotiations, and potential litigation. AccidentDoc Pasadena provides detailed documentation specifically designed for legal proceedings, going beyond standard medical records to establish causation, document disability, and support damages claims.
Our initial evaluation documents the accident mechanism in detail, correlating biomechanical forces with observed injuries. We note the specific collision type (rear-end, side-impact, frontal), estimated speed if known, whether the patient was aware of impending impact (bracing muscles provides some protection), seatbelt use, airbag deployment, vehicle damage, and whether the patient could drive away or required ambulance transport. This narrative establishes the temporal relationship between accident and injury onset, critical for proving causation.
Physical examination findings are documented with specificity: cervical range of motion measured in degrees using goniometry (normal: flexion 50°, extension 60°, rotation 80°, lateral flexion 45°), exact location of muscle tenderness and spasm, vertebral point tenderness at specific levels (e.g., "exquisite tenderness to palpation over C5 and C6 spinous processes"), neurological examination results including specific myotomes and dermatomes affected, and positive provocative tests with descriptions (e.g., "Spurling's test right side reproduced right arm radicular pain in C6 distribution").
Diagnostic imaging results are incorporated with clinical correlation: "MRI cervical spine dated [DATE] reveals C5-C6 disc herniation with rightward lateral component causing moderate right neural foraminal stenosis, consistent with patient's C6 radiculopathy characterized by right arm pain, biceps weakness, and diminished sensation over the radial forearm." This correlation between imaging findings and clinical presentation strengthens causation arguments.
Treatment plans document not just what we're doing but why: "Patient requires physical therapy 3x weekly for 8 weeks to restore normal cervical lordosis, improve deep neck flexor strength, and address myofascial trigger points. Failure to treat comprehensively risks chronic pain syndrome development." Progress notes document objective functional improvements: "Cervical rotation improved from 40° to 65° bilaterally. Patient now able to check blind spots while driving, previously impossible."
Causation statements explicitly link injuries to the accident: "It is my professional opinion within a reasonable degree of medical certainty that this patient's cervical spine injuries including C5-C6 disc herniation, cervical facet syndrome, and myofascial pain syndrome are directly and proximately caused by the motor vehicle collision of [DATE]. The documented mechanism (rear-end collision with sudden hyperextension-hyperflexion) is consistent with and sufficient to cause the observed injuries."
Disability ratings and restrictions are provided when maximum medical improvement (MMI) is reached: "Patient has reached MMI with 15% permanent partial impairment of the cervical spine per AMA Guides to the Evaluation of Permanent Impairment, 6th Edition. Permanent restrictions include: no overhead work, no lifting >25 lbs, frequent breaks from static postures, no work requiring sustained neck rotation."
Prognostic statements inform settlement negotiations: "Patient likely requires ongoing pain management including occasional trigger point injections and maintenance physical therapy. Future medical costs estimated at $2,500-3,500 annually. Risk of accelerated cervical degenerative changes (post-traumatic arthritis) is moderate to high, potentially requiring surgical intervention in 10-15 years."
We also provide expert witness testimony when needed, appearing for depositions or trial testimony to explain injuries, treatment, causation, and prognosis to attorneys, insurance adjusters, and juries. Our documentation is prepared with litigation in mind from day one, ensuring your attorney has the strongest possible medical evidence supporting your claim.
- Detailed accident mechanism documentation correlating forces with injuries
- Objective physical examination findings with measurements and specific locations
- Diagnostic imaging results with clinical correlation to symptoms
- Comprehensive treatment plans with medical necessity justification
- Causation statements linking injuries to accident within reasonable medical certainty
- Disability ratings using AMA Guides when at maximum medical improvement
- Work restrictions and functional capacity documentation
- Prognosis statements including future medical needs and costs
- Expert witness availability for depositions and trial testimony
While most whiplash injuries are managed on an outpatient basis through our clinic, certain symptoms indicate potentially serious complications requiring emergency department evaluation. Patients and family members should be educated to recognize these red flags and seek immediate care when present.
Neurological emergency signs include progressive arm numbness or weakness (suggests worsening nerve root compression or spinal cord injury), bilateral arm symptoms (indicates central spinal cord involvement rather than isolated nerve root), bowel or bladder dysfunction including urinary retention or incontinence (cauda equina syndrome or central cord syndrome), lower extremity weakness or numbness (cervical myelopathy from spinal cord compression), and difficulty with balance or coordination (posterior column involvement or vertebral artery injury).
Vascular emergency signs include severe headache with sudden onset reaching maximum intensity within seconds ("thunderclap headache" suggests vertebral artery dissection or subarachnoid hemorrhage), headache with vision changes such as double vision, visual field cuts, or transient blindness (posterior circulation stroke from vertebral artery injury), dizziness with dysphagia (difficulty swallowing), dysarthria (slurred speech), or facial numbness (brainstem stroke), and Horner's syndrome (ptosis, miosis, anhidrosis indicating sympathetic chain disruption from carotid or vertebral artery dissection).
Infectious warning signs include fever >101°F with neck pain and stiffness (meningitis, though rare after trauma), increasing pain despite treatment with constitutional symptoms like fever and night sweats (discitis or epidural abscess, typically developing weeks after penetrating injury or iatrogenic seeding).
Structural instability signs include severe pain with any neck movement suggesting instability, palpable cervical deformity or step-off (fracture-dislocation), and severe pain that is completely unrelenting despite all conservative measures (possible occult fracture).
When any of these red flag symptoms develop, we instruct patients to proceed immediately to the emergency department, preferably one with neurosurgery capabilities. Memorial Hermann Southeast Hospital, Houston Methodist Baytown Hospital, and Clear Lake Regional Medical Center all have neurosurgical coverage and advanced imaging available 24/7. After emergency stabilization and treatment, patients return to our care for ongoing management coordinated with the emergency intervention.
- Progressive arm numbness, weakness, or bilateral arm symptoms (nerve/cord injury)
- Bowel or bladder dysfunction - urinary retention or incontinence (cauda equina)
- Lower extremity weakness or numbness (cervical myelopathy)
- Sudden severe "thunderclap" headache (vertebral artery dissection)
- Headache with vision changes, double vision, or visual field defects (stroke)
- Dizziness with swallowing difficulty, slurred speech, or facial numbness (brainstem)
- Horner's syndrome - drooping eyelid, small pupil, no sweating on one side (arterial injury)
- Fever >101°F with neck stiffness (infection)
- Severe unrelenting pain despite all treatments (possible fracture)
- Difficulty with balance or coordination (posterior column or cerebellar involvement)
While many accidents are unavoidable, certain strategies reduce whiplash risk and severity. Proper headrest positioning is critical: the headrest should be adjusted so its top is level with the top of your head, positioned 2-3 inches from the back of your skull. This minimizes head travel distance during rear-end impacts. Studies show optimal headrest position reduces whiplash risk by up to 40%.
Maintaining good posture while driving—sitting upright with ears aligned over shoulders rather than forward head posture—provides better cervical spine alignment to withstand impact forces. Strengthening neck muscles through targeted exercises creates muscular protection. Awareness of surroundings and anticipating potential collisions allows protective muscle bracing, though this requires seeing the impending impact.
Post-injury self-care accelerates recovery: maintain gentle activity rather than prolonged immobilization, perform prescribed home exercises consistently, apply ice/heat as directed (ice for acute flares, heat for chronic stiffness), practice good sleep posture using cervical contour pillows, avoid prolonged static postures like computer work without breaks, and attend all scheduled therapy appointments. Ergonomic workstation setup prevents symptom exacerbation in office workers: monitor at eye level, keyboard positioned to keep elbows at 90°, lumbar support, and frequent posture changes every 30 minutes. These strategies combined with our comprehensive treatment approach optimize recovery and prevent chronic disability.
Seek Emergency Care Immediately If You Experience:
- Progressive arm numbness, weakness, or bilateral arm symptoms
- Bowel or bladder dysfunction (urinary retention or incontinence)
- Sudden severe "thunderclap" headache with vision changes
- Dizziness with difficulty swallowing or slurred speech
- Fever >101°F with neck stiffness
- Horner's syndrome (drooping eyelid, small pupil, facial asymmetry)
- Lower extremity weakness or difficulty walking
- Severe unrelenting pain despite all treatment measures
Call 911 or go to the nearest emergency room immediately

Lower back pain affects 80% of Americans at some point in their lives, with car accidents, workplace injuries, and slip-and-falls being leading causes of acute spinal trauma. The lumbar spine bears tremendous compressive and rotational forces during accidents, making it vulnerable to disc herniations, facet joint injuries, and muscular strains. AccidentDoc Pasadena's physicians employ comprehensive diagnostic and treatment protocols to address both acute injury and prevent chronic disability.
The lumbar spine consists of five vertebrae (L1-L5) plus the sacrum (S1), bearing the body's full weight during standing, walking, and lifting. Each motion segment includes the vertebral body, intervertebral disc, paired facet joints, ligamentous structures (anterior and posterior longitudinal ligaments, ligamentum flavum, interspinous and supraspinous ligaments), and surrounding musculature (erector spinae, multifidus, transversospinalis). The spinal canal houses the conus medullaris (spinal cord ending at L1-L2) and cauda equina (nerve roots L2-S5), with nerve roots exiting through neural foramina at each level.
Intervertebral discs are the spine's primary shock absorbers, consisting of a gelatinous nucleus pulposus surrounded by the tough annulus fibrosus. During compression forces typical of car accidents—particularly rear-end collisions where the torso is thrown into the seatback—the nucleus pulposus experiences tremendous pressure. If annular fibers are weakened by age-related degeneration or suddenly overloaded, the nucleus can herniate through the annular tear, typically in a posterolateral direction where annular fibers are thinnest and posterior longitudinal ligament support is minimal.
Facet joints are true synovial joints located posteriorly at each spinal level, guiding and limiting spinal motion. They are richly innervated by medial branch nerves and can generate significant pain when injured through capsular tears, cartilage damage, or inflammation. Rotational injuries during side-impact collisions or slip-and-falls particularly stress facet joints, as they limit rotational motion in the lumbar spine.
The L4-L5 and L5-S1 motion segments experience the greatest biomechanical stress due to their position at the lumbosacral junction, where the lumbar spine meets the relatively immobile sacrum. Approximately 95% of lumbar disc herniations occur at these two levels. The L5 nerve root (exiting at L4-L5) and S1 nerve root (exiting at L5-S1) are most commonly compressed, producing characteristic sciatica patterns: L5 radiculopathy causes dorsiflexion weakness (foot drop), lateral leg and dorsal foot numbness, and pain radiating down the posterior thigh and lateral leg. S1 radiculopathy causes plantarflexion weakness (difficulty standing on toes), posterior leg and plantar foot numbness, and pain radiating down the posterior leg to the heel.
Musculoligamentous injuries occur when sudden forces exceed tissue tolerances: multifidus and erector spinae muscles undergo eccentric overload during sudden deceleration, producing tears ranging from microscopic fiber disruption to complete muscle rupture. Ligamentous injuries involve the posterior ligamentous complex (supraspinous ligament, interspinous ligament, ligamentum flavum) and can create subtle spinal instability not always visible on static imaging.
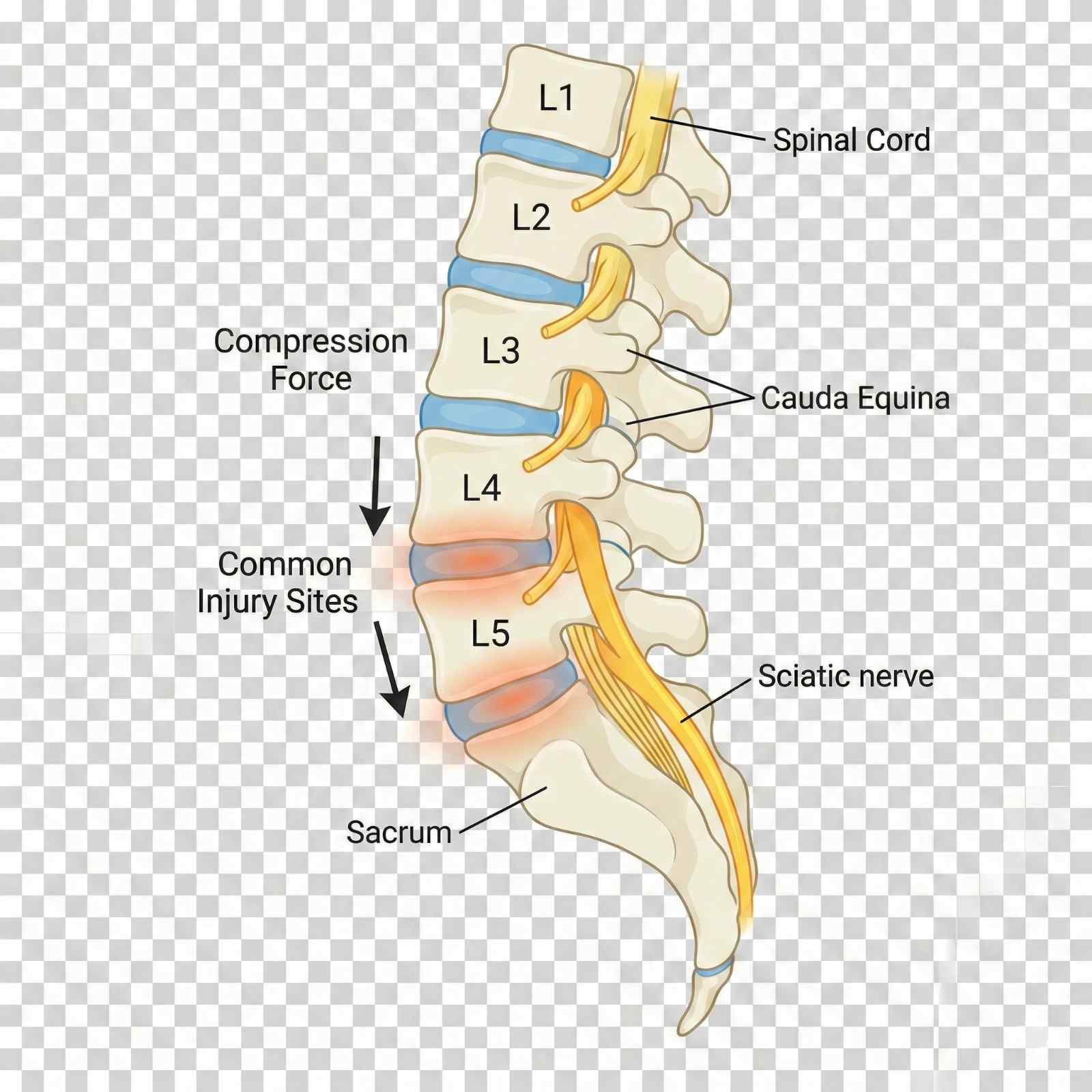
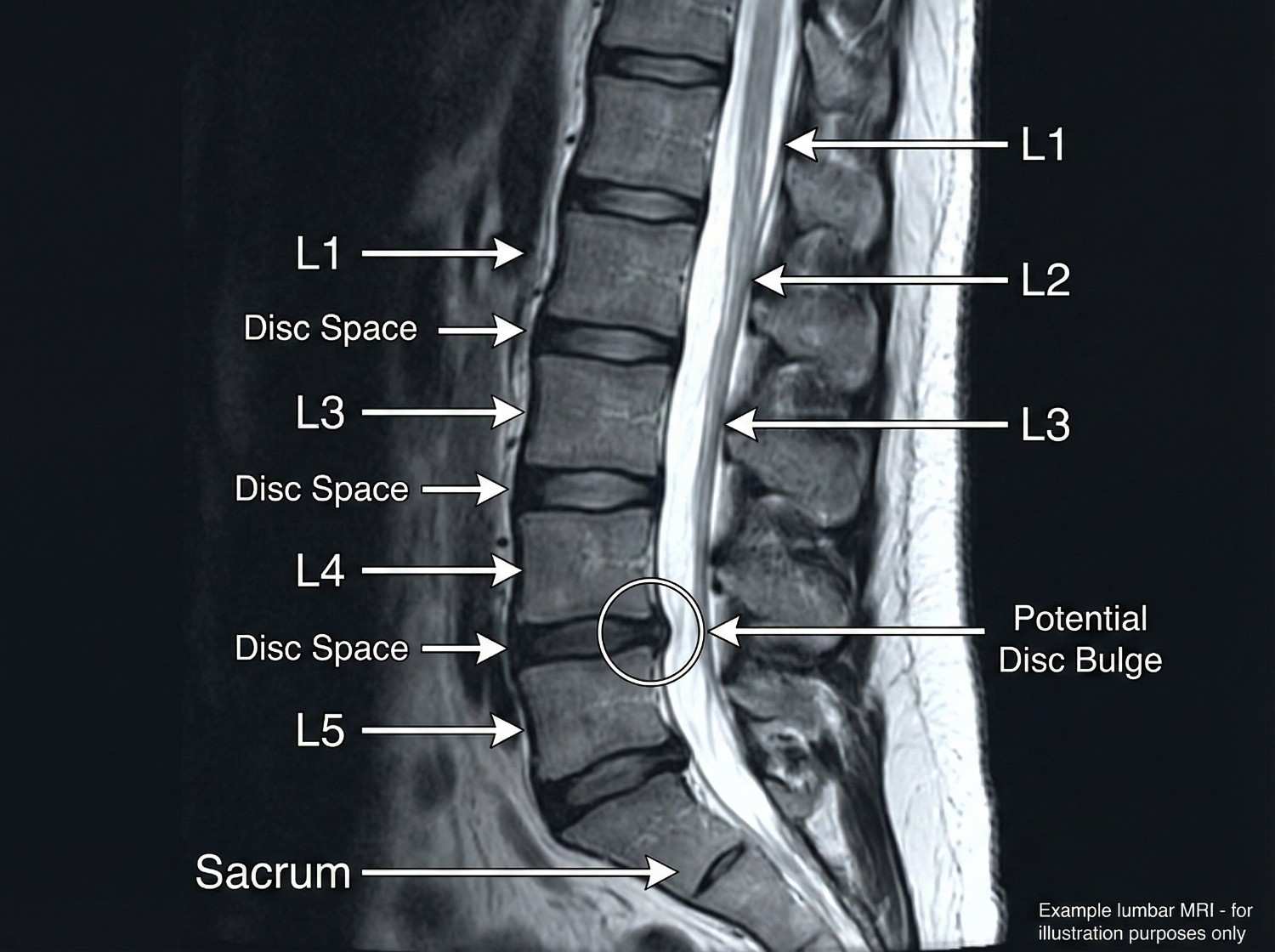
Compressive loading from rear-end and frontal collisions represents the most common mechanism of lumbar injury in motor vehicle accidents. When the vehicle suddenly decelerates, the torso continues forward until restrained by the seatbelt, creating compressive and flexion forces on the lumbar spine. These forces can exceed 3,000 Newtons, sufficient to cause annular tears and disc herniations. The L4-L5 disc, positioned at the apex of lumbar lordosis, experiences maximal stress and is most frequently injured.
Lifting injuries in workplace settings account for substantial lumbar spine trauma, particularly in warehouse, construction, and healthcare workers. Improper lifting mechanics—bending at the waist rather than knees, twisting while lifting, or sudden unexpected loads—create asymmetric compressive and rotational forces exceeding disc and ligament tolerances. The Occupational Safety and Health Administration (OSHA) estimates that overexertion injuries, primarily lumbar strain and disc injuries, cost American businesses $15.1 billion annually in workers' compensation claims.
Slip-and-fall accidents generate unique injury patterns depending on landing position: landing on the buttocks creates axial loading through the sacrum, potentially causing sacral fractures, L5-S1 disc injury, or compression fractures in osteoporotic vertebrae. Landing on the side produces lateral compression and rotational forces, injuring facet joints and causing transverse process fractures. The sudden unexpected nature of falls prevents protective muscle activation, allowing full force transmission to skeletal structures.
Repetitive bending, twisting, and lifting in occupations like construction, refinery work, and warehouse operations causes cumulative trauma to lumbar discs. Each loading cycle causes microscopic annular fiber tears; when accumulated over months to years, these coalesce into macroscopic defects allowing nuclear herniation. Even without a specific acute event, workers develop symptomatic disc herniations that are compensable under Texas workers' compensation law as cumulative trauma injuries.
In Pasadena's industrial corridor along Highway 225, refinery and petrochemical workers experience unique mechanisms including falls from height, being struck by falling equipment or materials, and crush injuries from machinery. These high-energy mechanisms often cause multiple-level injuries, fractures, and combined bone-soft tissue trauma requiring comprehensive multidisciplinary care.
- Motor vehicle accidents (rear-end and frontal) - compression and flexion forces
- Lifting injuries with improper mechanics - twisting, bending, unexpected loads
- Slip-and-fall on buttocks - axial loading through sacrum to L5-S1
- Repetitive occupational bending and lifting - cumulative disc trauma
- Falls from height - high-energy compression and fracture risk
- Industrial accidents - crush injuries, being struck by objects
- 18-wheeler accidents - severe multi-level injuries from high forces
Lumbar spine injury symptoms range from localized mechanical back pain to severe radiculopathy with neurological deficits, depending on involved structures. Understanding this symptom spectrum guides diagnostic workup and treatment selection.
Mechanical low back pain from muscular strain and facet joint injury manifests as localized lumbar discomfort, often described as deep aching or sharp with movement. Pain worsens with extension (bending backward, overhead reaching) in facet-mediated pain, and with flexion (forward bending, sitting) in discogenic pain. Muscle spasm is palpable as firm, tender bands in the paraspinal muscles, representing protective guarding. Range of motion is restricted, particularly in the direction stressing injured structures. Mechanical pain typically remains localized to the back and buttocks without leg radiation.
Sciatica, the hallmark of nerve root compression, presents as sharp, burning, or electric pain radiating from the lower back down the posterior or lateral thigh, through the calf, and into the foot. The pain distribution follows specific dermatomal patterns: L5 radiculopathy produces lateral leg and dorsal foot pain, while S1 radiculopathy causes posterior leg and plantar foot pain. Patients often describe the pain as "shooting" or "like an electric shock," distinctly different from muscular aching. The pain intensity often exceeds back pain, and patients report that leg pain is their primary complaint.
Neurological symptoms accompany more severe nerve compression: numbness or paresthesias (tingling) in dermatomal distributions, weakness in specific muscle groups (L5: foot dorsiflexion and toe extension; S1: plantarflexion and toe flexion), and reduced or absent deep tendon reflexes (L5: medial hamstring; S1: Achilles). These neurological deficits indicate need for prompt MRI and potentially urgent intervention if progressive.
Cauda equina syndrome represents a surgical emergency requiring immediate decompression, characterized by bilateral leg symptoms, saddle anesthesia (numbness in the perineal region), bowel or bladder dysfunction (urinary retention most common initially, followed by overflow incontinence), and progressive bilateral leg weakness. Though rare (occurring in 1-2% of large disc herniations), cauda equina syndrome risk necessitates education of all patients with severe sciatica about warning signs.
Delayed symptom onset is common in lumbar injuries: patients may feel "fine" immediately after accidents, only to develop severe pain 24-48 hours later as inflammation peaks. This delayed onset doesn't invalidate causation—it reflects the natural inflammatory timeline following soft tissue injury.
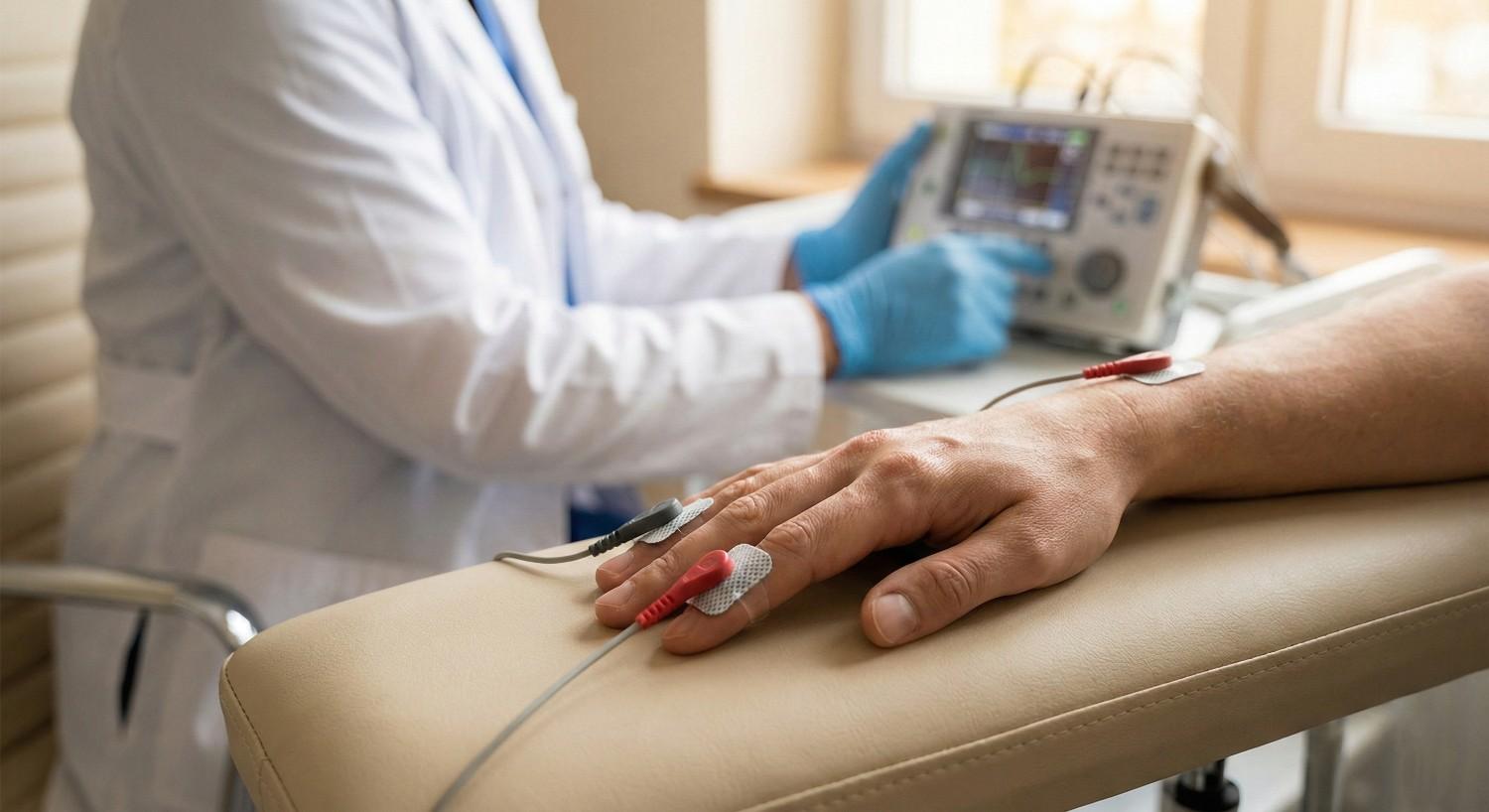
| Symptom | Timing / Description |
|---|---|
| Localized low back pain | Immediate to Delayed |
| Pain with forward bending | Immediate to Delayed |
| Pain with backward bending | Immediate to Delayed |
| Sciatica (leg pain) | Delayed (24-72 hours) |
| Leg numbness/tingling | Delayed to Chronic |
| Foot drop (L5) | Delayed to Chronic |
| Difficulty standing on toes (S1) | Delayed to Chronic |
| Reduced reflexes | Delayed to Chronic |
| Bilateral leg symptoms | Emergency |
| Bowel/bladder dysfunction | Emergency |
Comprehensive diagnostic evaluation combines clinical assessment with targeted imaging to identify all injured structures and guide treatment decisions. Our systematic approach ensures accurate diagnosis while avoiding unnecessary testing.
Clinical examination begins with observing gait, posture, and spinal contour—loss of normal lumbar lordosis suggests muscle spasm and protective guarding. Active range of motion testing quantifies functional limitations: forward flexion (normal: fingers to floor or within 10cm), extension (normal: 25-30°), lateral flexion (normal: 25-30° each side), and rotation (normal: 30-45° each direction, though limited in lumbar spine). We use goniometry or inclinometry for objective documentation supporting disability ratings.
Palpation identifies point tenderness over spinous processes (suggesting fracture, ligament injury, or facet pathology), paraspinal muscle spasm and trigger points, and sacroiliac joint tenderness (commonly injured in falls on buttocks). Percussion over spinous processes elicits pain in vertebral fractures. Straight leg raise test (SLR) is the gold standard provocative maneuver for lumbar radiculopathy: with the patient supine, we slowly raise the extended leg; pain radiating below the knee between 30-70° of elevation indicates nerve root tension, highly specific for disc herniation when the pain is reproduced in the contralateral leg (crossed SLR). Femoral nerve stretch test (patient prone, knee flexed, hip extended) reproduces anterior thigh pain in upper lumbar radiculopathy (L2-L4).
Neurological examination systematically assesses motor function (manual muscle testing of hip flexors L2, quadriceps L3/L4, ankle dorsiflexion L5, ankle plantarflexion S1), sensory function (light touch and pinprick in all dermatomes), and reflexes (patellar L4, medial hamstring L5, Achilles S1). Documentation notes specific findings: "4/5 strength ankle dorsiflexion right, 2+ Achilles reflex left vs 0 right, sensory deficit plantar foot S1 distribution right—consistent with S1 radiculopathy."
Imaging selection follows evidence-based guidelines: Lumbar X-rays (AP and lateral views) are initial studies to assess alignment, measure disc space heights (narrowing suggests degeneration), identify fractures or spondylolisthesis (vertebral slippage), and evaluate for degenerative changes. Flexion-extension views assess spinal stability when ligamentous injury is suspected. X-rays have limited utility for soft tissue evaluation but are valuable for initial screening.
MRI lumbar spine without contrast is the definitive study for disc herniations, nerve root compression, spinal stenosis, ligamentous injuries, and bone marrow edema indicating fractures. We order MRI when radicular symptoms exist, neurological deficits are present, severe pain persists beyond 4-6 weeks of conservative care, or red flag symptoms suggest serious pathology (cauda equina, infection, malignancy). MRI findings are correlated with clinical presentation—incidental disc bulges without nerve compression don't explain radicular symptoms, while a right posterolateral disc herniation compressing the right S1 nerve root perfectly explains right S1 radiculopathy.
CT scanning provides superior bony detail for fractures, pars defects (spondylolysis), and bony stenosis, but lacks MRI's soft tissue resolution. CT myelography (CT after intrathecal contrast injection) is reserved for patients unable to undergo MRI (pacemakers, certain metal implants) when soft tissue visualization is necessary.
Electrodiagnostic studies (EMG/NCS) performed 3-4 weeks post-injury detect physiological nerve injury even when MRI shows anatomical compression. Abnormal findings include fibrillation potentials and positive sharp waves (denervation), reduced motor unit recruitment (weakness), and slowed nerve conduction velocities. EMG differentiates radiculopathy from peripheral nerve entrapments (peroneal nerve palsy mimics L5 radiculopathy) and polyneuropathy.
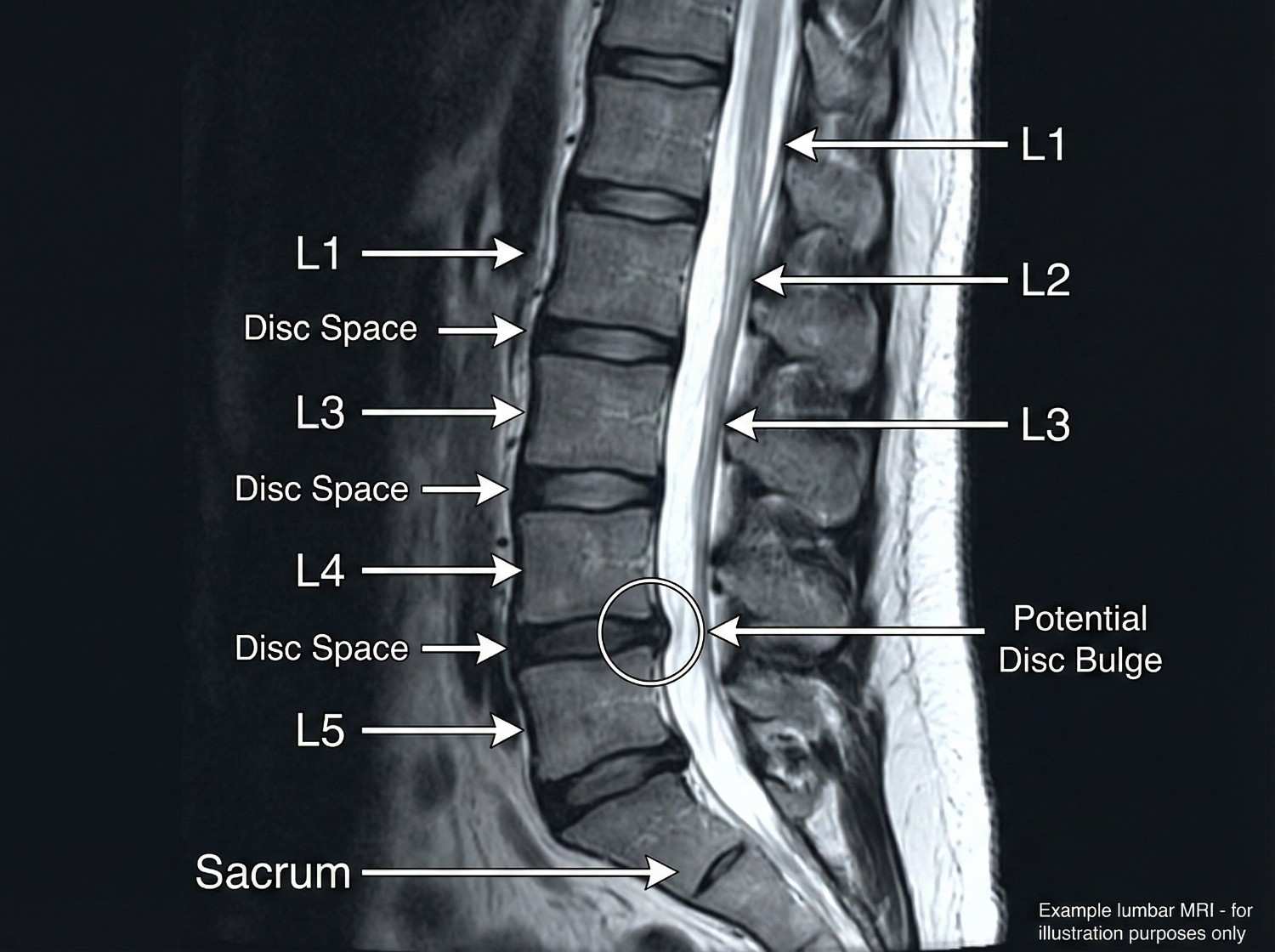
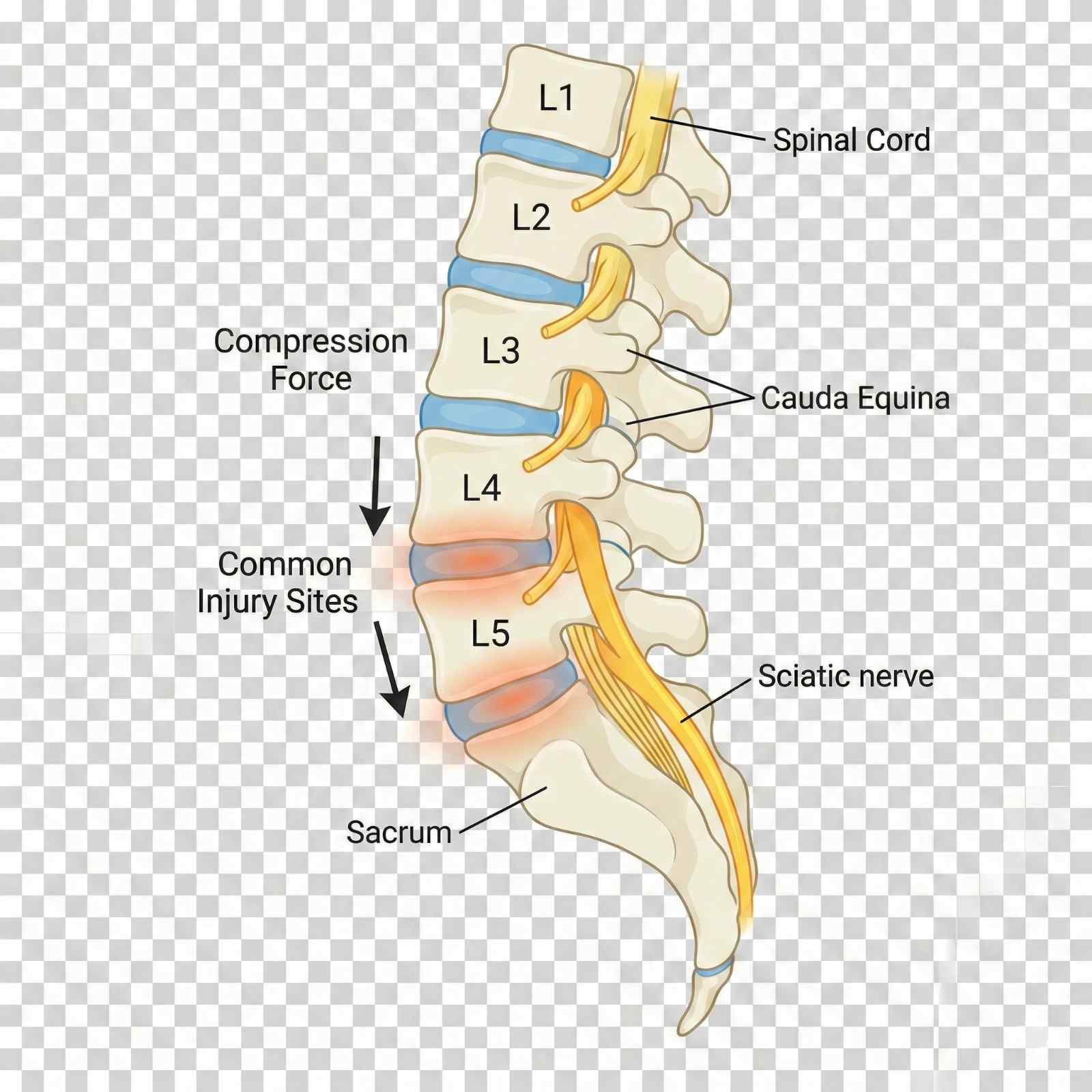
Our evidence-based treatment protocols progress through phases based on injury severity, patient response, and functional goals. All care is available through Letter of Protection with $0 out-of-pocket cost.
Phase 1 (Acute: Days 1-10) emphasizes controlled activity, not bed rest. Research demonstrates that prolonged bed rest delays recovery and increases chronic pain risk; we recommend limiting bed rest to 2-3 days maximum. Activity modification avoids pain-provoking movements (heavy lifting, prolonged sitting, twisting) while maintaining general activity. Ice application (20 minutes every 2-3 hours) reduces inflammation in the first 48 hours, then alternating ice/heat provides symptomatic relief. Medication includes NSAIDs (ibuprofen 800mg TID or naproxen 500mg BID) for inflammation, muscle relaxants (cyclobenzaprine 5-10mg at bedtime, tizanidine 4mg TID) for muscle spasm, and neuropathic pain medications (gabapentin, pregabalin) for radiculopathy. Short-course oral corticosteroids (methylprednisolone dose pack) provide potent anti-inflammatory effect for severe radiculopathy.
Phase 2 (Subacute: Weeks 2-8) introduces active rehabilitation. Physical therapy employs multiple modalities: McKenzie method (repeated extension exercises) centralizes pain from the leg back to the central spine, indicating favorable prognosis; core stabilization strengthens transversus abdominis, multifidus, and other deep stabilizers that protect the spine; manual therapy including soft tissue mobilization and joint mobilization improves mobility; and functional training retrains proper movement patterns for daily activities and work tasks. A typical protocol involves 2-3 sessions weekly for 6-8 weeks.
Chiropractic care utilizes flexion-distraction technique (Cox technique) which gently stretches the lumbar spine, creating negative intradiscal pressure that may reduce disc herniations while mobilizing facet joints. High-velocity low-amplitude (HVLA) adjustments restore normal joint motion in restricted segments. Side-posture manipulation is employed cautiously in acute disc herniation, prioritizing flexion-distraction initially. Treatment frequency typically starts at 3x weekly, tapering to 2x then 1x weekly as symptoms improve.
Massage therapy addresses secondary myofascial dysfunction: gluteus medius, piriformis, quadratus lumborum, and erector spinae often develop trigger points and hypertonicity secondary to primary lumbar pathology. Deep tissue massage, myofascial release, and trigger point therapy reduce muscle pain and improve flexibility, allowing more effective participation in strengthening exercises.
Phase 3 (Intermediate: Weeks 8-16) employs interventional procedures when conservative care provides inadequate relief. Epidural steroid injections are the gold standard for radiculopathy from disc herniation. Performed under fluoroscopic guidance, we deliver corticosteroid and local anesthetic directly to the inflamed nerve root via transforaminal (most specific, targets individual nerve root), interlaminar (midline approach, broader coverage), or caudal (through sacral hiatus, good for multi-level or S1 pathology) approaches. Success rates range from 50-70% for significant pain reduction lasting 3+ months, with best results in acute radiculopathy (<3 months duration) from contained disc herniations.
Facet joint injections target the zygapophyseal joints with fluoroscopically-guided injection of anesthetic and corticosteroid, both diagnostic (>80% pain relief confirms facet-mediated pain) and therapeutic. Medial branch blocks anesthetize the nerves innervating facet joints; patients achieving >80% pain relief for the duration of local anesthetic action are candidates for radiofrequency ablation. Radiofrequency ablation (RFA) uses thermal energy to create controlled lesions in medial branch nerves, providing 6-12 months of pain relief with repeatability. RFA is particularly effective for chronic facet-mediated pain unresponsive to conservative care.
Trigger point injections deliver local anesthetic (and sometimes corticosteroid) to hyperactive muscle trigger points in paraspinal, gluteal, and piriformis muscles, providing immediate pain relief and allowing advancement of physical therapy. Sacroiliac joint injections address SI joint dysfunction common after falls on buttocks or asymmetric loading patterns.
Phase 4 (Surgical: When Conservative Care Fails) is considered after 6+ months of comprehensive non-surgical treatment without adequate improvement, or sooner if progressive neurological deficits, cauda equina syndrome, or severe functional impairment exist. Microdiscectomy is the gold standard for disc herniation with radiculopathy, involving microscopic removal of herniated disc material compressing the nerve root. Success rates exceed 85-90% for leg pain relief, though back pain improves less reliably. Laminectomy removes bone (lamina) to decompress spinal canal stenosis causing neurogenic claudication. Spinal fusion stabilizes painful motion segments using bone graft and instrumentation (pedicle screws and rods), appropriate for spondylolisthesis, instability, or severe degenerative disc disease after failed conservative care.


Acute Phase (Days 1-10)
1-10 daysControlled activity (bed rest <3 days), ice/heat, NSAIDs, muscle relaxants, neuropathic pain medication. Activity modification avoiding pain triggers.
Subacute Phase (Weeks 2-8)
2-8 weeksPhysical therapy (McKenzie method, core stabilization), chiropractic (flexion-distraction, HVLA), massage therapy for myofascial pain. 2-3x weekly.
Intermediate Phase (Weeks 8-16)
8-16 weeksInterventional procedures: epidural steroid injections, facet injections, medial branch blocks, radiofrequency ablation, trigger point injections.
Surgical Phase (If Needed)
Case dependentMicrodiscectomy for disc herniation, laminectomy for stenosis, fusion for instability. After 6+ months conservative care or if progressive neurological deficits.
Lumbar spine injury recovery varies significantly based on specific pathology, severity, patient age, baseline fitness, and psychosocial factors including job satisfaction and litigation status. Understanding expected timelines helps maintain realistic expectations.
Lumbar muscle strain (no radiculopathy, no disc herniation) typically resolves in 6-8 weeks with conservative care. Most patients achieve 80% improvement by 4 weeks, with residual discomfort managed through home exercise and occasional NSAIDs. Return to sedentary work occurs at 2-3 weeks with activity modification; return to heavy labor at 6-8 weeks with gradual job conditioning.
Lumbar disc herniation with radiculopathy follows a longer course: natural history studies show that 60-70% of patients improve significantly with non-surgical care over 3-6 months. Initial severe leg pain typically improves first (within 4-8 weeks), followed by neurological recovery (strength, sensation) over 2-4 months. Approximately 10-15% of patients undergo surgery due to either failure of conservative care (persistent severe pain and disability) or progressive neurological deficits. Post-surgical recovery from microdiscectomy typically allows return to light work at 4-6 weeks, heavy work at 3 months, with continued improvement to one year.
Chronic low back pain (>3 months duration) requires multifaceted treatment addressing physical deconditioning, pain psychology, and functional restoration. Functional restoration programs combining intensive physical therapy, cognitive-behavioral therapy, and work conditioning produce superior outcomes compared to passive treatment modalities, with 65-75% of patients returning to pre-injury work status within 6 months of program completion.
Spinal fusion recovery is prolonged: bony fusion consolidation requires 6-12 months, though functional recovery allows desk work at 6-8 weeks, light physical work at 3-4 months, and unrestricted activity at 6-9 months post-surgery. Fusion at one level increases adjacent segment stress by approximately 30-40%, potentially accelerating degeneration at adjacent levels with 20-30% of patients developing adjacent segment disease within 10 years.
Factors predicting prolonged recovery include high initial pain intensity, widespread pain beyond primary injury site, catastrophic thinking and fear-avoidance beliefs, job dissatisfaction or workplace conflict, pending litigation (though treatment shouldn't be delayed), smoking (impairs tissue healing), obesity (increases mechanical spine loading), and pre-existing degenerative changes. Conversely, positive prognostic factors include rapid initial improvement (>30% pain reduction in first 2 weeks), good treatment compliance, strong social support, satisfying job with supportive employer, non-smoking status, and healthy body weight.
We monitor specific functional milestones: walking tolerance (goal: 30+ minutes continuous), sitting tolerance (goal: 45-60 minutes before requiring position change), lifting capacity (progressively increasing from 5 lbs to job-specific requirements), and pain-free sleep. Functional capacity evaluations performed at 8-12 weeks objectively document work capabilities and restrictions, invaluable for workers' compensation and personal injury cases.

Comprehensive documentation for lumbar spine injuries requires correlation of mechanism, clinical findings, imaging results, and functional limitations. Our reports are specifically designed for legal proceedings, insurance negotiations, and workers' compensation claims.
Mechanism documentation establishes causation: "Patient sustained lumbar spine injury on [DATE] when struck from behind while stopped at traffic light on Red Bluff Road. The sudden deceleration and compressive loading of the lumbar spine in seated position is biomechanically consistent with and sufficient to cause the observed L5-S1 disc herniation." For workers' compensation cases: "Cumulative trauma from repetitive lifting of 50-75 lb boxes while employed as warehouse associate for [EMPLOYER] from 2020-2024 caused progressive annular deterioration and eventual L4-L5 disc herniation becoming symptomatic on [DATE]."
Physical examination findings are documented with quantification: "Lumbar forward flexion limited to 40° (normal 90°), extension 10° (normal 25°), right lateral flexion 15° (normal 25°). Positive straight leg raise test right side reproducing S1 radiculopathy at 35° elevation. Absent right Achilles reflex, 4/5 plantarflexion strength right, sensory deficit plantar foot S1 distribution. Positive facet loading test L4-L5 and L5-S1 bilaterally."
Imaging correlation strengthens causation arguments: "MRI lumbar spine dated [DATE] demonstrates large right posterolateral disc herniation at L5-S1 with moderate to severe right neural foraminal stenosis and displacement of the right S1 nerve root. These findings directly correlate with and explain the patient's clinical presentation of right S1 radiculopathy characterized by posterior leg pain radiating to heel, plantar foot numbness, reduced plantarflexion strength, and absent Achilles reflex."
Treatment documentation emphasizes medical necessity: "Patient requires epidural steroid injection at L5-S1 to reduce neural inflammation and facilitate participation in physical therapy. Conservative measures including 8 weeks of physical therapy, chiropractic care, and medication management have provided only partial relief (30% improvement per VAS). Without interventional treatment, patient faces high risk of chronic pain syndrome development and possible surgical necessity."
Causation opinions are stated clearly: "Within a reasonable degree of medical probability, this patient's L5-S1 disc herniation and resultant S1 radiculopathy are directly and proximately caused by the motor vehicle collision of [DATE]. The documented mechanism (sudden deceleration with compressive loading) is biomechanically consistent with disc herniation. The temporal relationship (symptoms developing within 24 hours of accident) supports causation. The patient had no prior history of lumbar radiculopathy or disc herniation, with prior medical records documenting only occasional mechanical back pain responsive to over-the-counter medication. The current condition represents new injury directly attributable to the accident."
Disability ratings using AMA Guides to Evaluation of Permanent Impairment, 6th Edition, are provided at maximum medical improvement: "Patient has reached MMI 14 months post-injury after conservative care and one-level microdiscectomy. Residual findings include: 25% loss of lumbar range of motion, persistent 4+/5 ankle plantarflexion weakness right, diminished S1 dermatomal sensation. Using DRE (Diagnosis-Related Estimate) Category III (radiculopathy with objective findings), patient has 13% whole person impairment." Permanent restrictions guide return-to-work planning: "Permanent restrictions include: lifting limited to occasional 25 lbs, frequent 15 lbs; no repetitive bending or twisting; no prolonged static postures (sitting/standing >45 minutes without position change); no work requiring prolonged driving; no climbing ladders or scaffolds."
Future medical needs and costs are estimated: "Patient will require ongoing pain management including episodic physical therapy (estimated 8-12 sessions annually), periodic epidural injections (1-2 annually), medication management, and possible additional surgery if adjacent segment degeneration develops (20-30% risk over 10 years, estimated cost $75,000-100,000)."
Life care planning for catastrophic injuries documents all future medical, therapeutic, and supportive care needs with associated costs over the patient's remaining lifetime, supporting economic damages claims in personal injury litigation.
- Mechanism documentation establishing biomechanical causation
- Quantified physical examination with range of motion measurements
- Imaging findings correlated with clinical presentation
- Treatment plans with medical necessity justification
- Causation opinions stated within reasonable medical probability
- Disability ratings per AMA Guides at maximum medical improvement
- Permanent work restrictions for return-to-work and vocational assessment
- Future medical needs and costs for life care planning
- Expert witness testimony availability for depositions and trial
Certain lumbar spine injury presentations indicate surgical emergencies or serious underlying pathology requiring immediate advanced care. Patient education about these red flags is critical for preventing permanent disability.
Cauda equina syndrome is a neurosurgical emergency caused by massive central disc herniation or other space-occupying lesion compressing multiple nerve roots of the cauda equina. Classic presentation includes bilateral leg pain and weakness (distinguishing it from typical unilateral radiculopathy), saddle anesthesia (numbness in the perineal region, inner thighs, and buttocks—areas that would contact a saddle), and bowel/bladder dysfunction initially presenting as urinary retention (inability to void despite full bladder sensation), progressing to overflow incontinence and fecal incontinence. Sexual dysfunction is also common. Cauda equina requires emergency MRI and surgical decompression within 24-48 hours; delays beyond 48 hours are associated with significantly increased rates of permanent bowel/bladder dysfunction and sexual impairment. Any patient presenting with bilateral leg symptoms and saddle symptoms should proceed immediately to an emergency department with neurosurgical coverage.
Progressive motor weakness, particularly rapid progression or weakness affecting multiple myotomes bilaterally, suggests either cauda equina syndrome or conus medullaris syndrome (injury to the spinal cord terminus at L1-L2). Isolated foot drop (L5) developing or worsening despite treatment warrants urgent MRI and possible surgical consultation, as prolonged nerve compression beyond 6-8 weeks reduces likelihood of neurological recovery even after successful decompression.
Bowel or bladder changes including urinary retention (most sensitive early sign of cauda equina), new onset urinary incontinence, fecal incontinence, or loss of rectal tone (assessed by digital rectal examination in emergency department) all mandate emergency evaluation. Patients should be instructed that difficulty initiating urination or decreased awareness of bladder fullness warrants immediate ER evaluation.
Fever with back pain raises concern for spinal infection including discitis (disc space infection), osteomyelitis (vertebral body infection), or epidural abscess. Risk factors include diabetes, immunosuppression, IV drug use, recent spine procedure/injection, or penetrating injury. Spinal infections can progress rapidly to neurological compromise and sepsis; immediate evaluation with MRI and laboratory studies (white blood cell count, erythrocyte sedimentation rate, C-reactive protein, blood cultures) is essential.
Nocturnal pain worse than daytime pain, particularly pain that awakens the patient from sleep and is not relieved by any position, raises concern for neoplasm (primary spinal tumor or metastatic disease). Constitutional symptoms including unexplained weight loss, fever, night sweats, or history of cancer increase suspicion. These patients require prompt MRI to evaluate for pathologic fracture, epidural tumor, or metastatic disease.
Significant trauma, especially in elderly patients or those with known osteoporosis, risks vertebral compression fractures. Acute severe back pain after fall, motor vehicle accident, or other trauma warrants X-rays initially; MRI is added if neurological symptoms develop or if fracture involves the posterior vertebral body (risk of retropulsed fragments compressing neural elements).
When any red flag symptom develops, we direct patients to emergency departments with neurosurgical capabilities: Memorial Hermann Southeast, Houston Methodist Baytown, Clear Lake Regional Medical Center, or Ben Taub Hospital for indigent patients. After emergency stabilization, patients return to our clinic for coordinated ongoing care.
- Cauda equina syndrome - bilateral leg pain/weakness, saddle anesthesia, urinary retention - SURGICAL EMERGENCY
- Progressive motor weakness, especially bilateral or multi-level
- Bowel or bladder dysfunction - incontinence or retention
- Fever with back pain - suggests infection (discitis, epidural abscess)
- Nocturnal pain worse than daytime - concern for neoplasm
- Unexplained weight loss, night sweats - systemic disease
- Significant trauma in elderly/osteoporotic patients - fracture risk
- Pain unrelieved by any position or intervention - severe pathology
- Bilateral leg numbness or weakness - central compression
- Loss of rectal tone or anal sphincter control - cauda equina
While many lumbar injuries result from unavoidable accidents, risk reduction strategies and proper ergonomics minimize injury severity and prevent chronic disability. Proper lifting mechanics are fundamental: always bend at knees rather than waist, keep load close to body (increasing lever arm by holding load away from body exponentially increases lumbar compression forces), avoid twisting while lifting (rotational forces maximally stress annulus fibrosus), and test load weight before committing to the lift. OSHA recommends limiting repetitive lifting to 51 lbs maximum for most workers, with lower limits (25 lbs) for frequent lifting.
Workplace ergonomics modifications include adjustable-height workstations allowing sit-stand alternation for office workers, anti-fatigue mats for workers in static standing positions, mechanical lifting aids (forklifts, pallet jacks, hoists) for material handling, team lifts for loads exceeding individual safe lifting limits, and job rotation to vary physical demands and prevent cumulative trauma. Core strengthening through targeted exercises creates muscular protection: transversus abdominis and multifidus provide spinal stability, while erector spinae, quadratus lumborum, and hip muscles contribute to load distribution. A basic core program includes planks, bird-dogs, dead bugs, and bridges performed 3-4x weekly.
Maintaining healthy body weight reduces chronic lumbar loading—each pound of excess abdominal weight creates amplified force on lumbar discs due to leverage effects. Smoking cessation improves disc nutrition (nicotine impairs blood flow to intervertebral discs) and enhances healing capacity. Post-injury, adherence to prescribed rehabilitation exercises prevents recurrence and chronic disability. Workplace accommodation through light duty assignments during recovery allows earlier return to work while respecting healing tissue limitations, reducing overall disability duration.
Seek Emergency Care Immediately If You Experience:
- Bilateral leg pain, weakness, or numbness (cauda equina syndrome)
- Saddle anesthesia - numbness in perineal area, inner thighs, buttocks
- Urinary retention, inability to void, or new incontinence
- Fecal incontinence or loss of bowel control
- Progressive motor weakness despite treatment
- Fever >101°F with back pain (possible infection)
- Nocturnal pain worse than daytime pain (possible tumor)
- Unexplained weight loss with back pain
- Significant trauma in elderly patients (fracture risk)
Call 911 or go to the nearest emergency room immediately

Soft tissue injuries encompassing muscles, tendons, and ligaments account for over 70% of all accident-related injuries. These injuries range from minor strains resolving in weeks to severe ruptures requiring surgical repair. Despite often lacking dramatic imaging findings, soft tissue injuries can cause substantial pain, functional impairment, and long-term disability. AccidentDoc Pasadena provides comprehensive evaluation and treatment of all soft tissue injury grades.
Soft tissues include all non-bony, non-neural structures: skeletal muscles that generate movement, tendons connecting muscles to bones, ligaments connecting bones to each other, and fascia providing structural support and force transmission. Understanding the grading system for soft tissue injuries guides treatment selection and prognosis.
Muscle injuries are classified by severity: Grade 1 (Mild Strain) involves microscopic muscle fiber tears with minimal loss of strength and function. Pain develops gradually and is typically manageable with over-the-counter medication. Swelling is minimal, and ecchymosis (bruising) is often absent. Patients maintain >80% of normal strength. Recovery typically occurs within 2-3 weeks with conservative care.
Grade 2 (Moderate Strain/Partial Tear) involves significant muscle fiber disruption with measurable loss of strength and function. A palpable defect or divot may be felt at the injury site. Pain is moderate to severe, especially with muscle activation. Swelling appears within 24-48 hours, and ecchymosis develops 2-5 days post-injury as blood dissects through tissue planes. Patients retain 50-80% of normal strength. Recovery requires 6-12 weeks including rehabilitation.
Grade 3 (Severe Strain/Complete Rupture) involves full-thickness muscle or musculotendinous junction tear with complete loss of function. A visible or palpable defect exists, often with bunching of the retracted muscle belly. Initial pain may be severe but can paradoxically decrease as torn nerve endings separate. Massive ecchymosis develops. Patients have <50% of normal strength or complete inability to contract the muscle. These injuries often require surgical repair, particularly in critical muscles like Achilles tendon, patellar tendon, or rotator cuff, with 3-6 month recovery.
Tendon injuries follow similar grading: Grade 1 (tendinopathy) involves inflammatory changes and microscopic fiber disruption without gross tear. Grade 2 (partial tear) involves significant fiber disruption with preserved continuity. Grade 3 (complete rupture) is full-thickness tear with loss of continuity, causing complete functional loss and requiring surgical repair in most locations.
Ligament sprains use the same three-grade classification: Grade 1 involves microscopic tears with preserved stability (stress testing shows normal joint stability). Grade 2 involves partial tear with mild-to-moderate laxity on stress testing but preserved endpoint. Grade 3 involves complete tear with marked laxity and absent endpoint, often requiring surgical reconstruction.
Contusions (bruises) result from direct trauma causing muscle crushing, capillary rupture, and hematoma formation without fiber tearing. They range from mild (minor pain, small hematoma) to severe (large intramuscular hematoma causing compartment-like pressure and possible myositis ossificans—heterotopic bone formation in muscle). Seatbelt contusions across the shoulder, chest, and abdomen are classic accident injuries, sometimes associated with underlying organ injury (liver or spleen in severe cases).
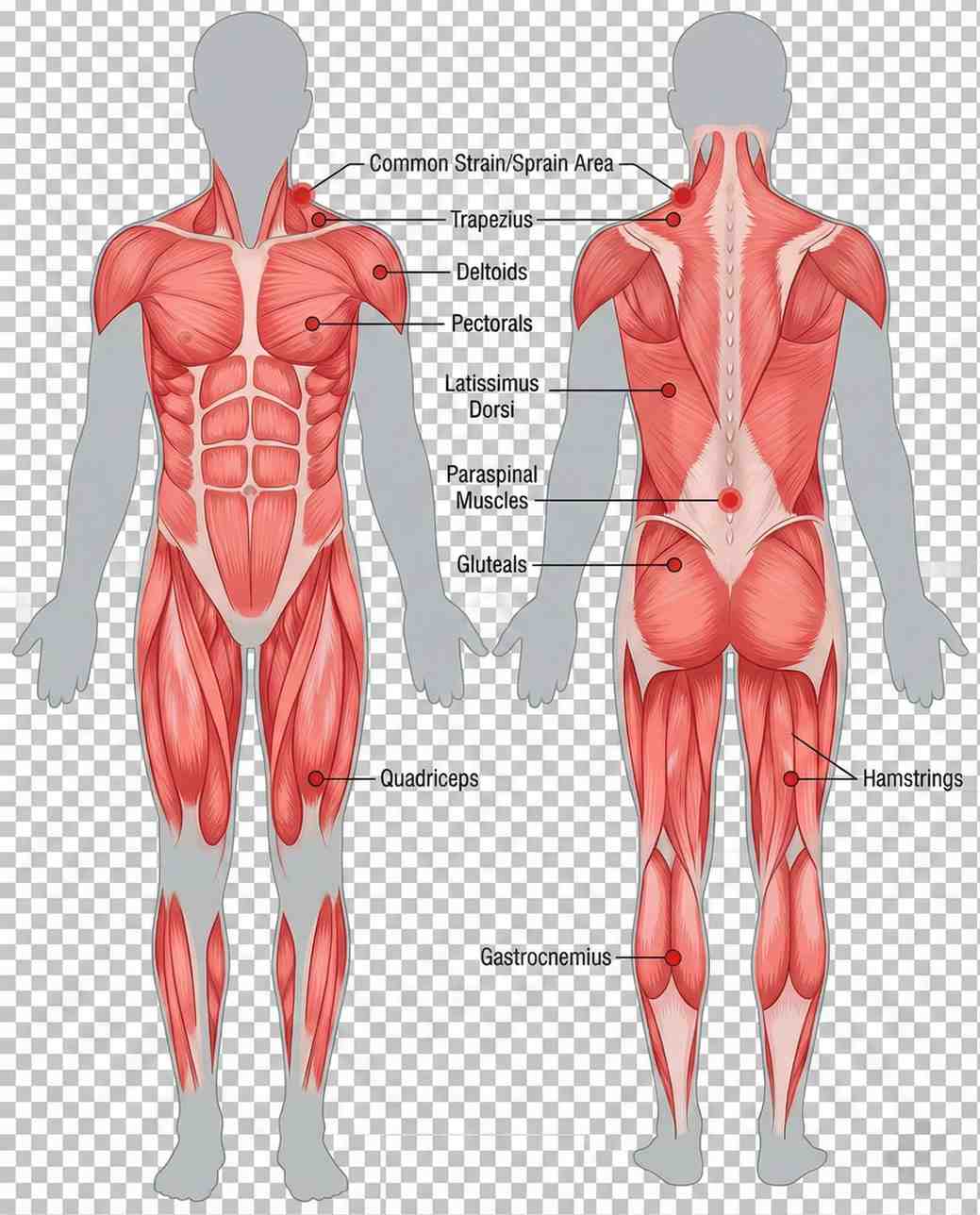

Soft tissue injuries result from multiple mechanisms in accident scenarios. Seatbelt trauma represents a unique injury pattern where the three-point restraint system loads soft tissues in a diagonal band across the chest, shoulder, and abdomen during sudden deceleration. The shoulder belt crosses the pectoralis major muscle, anterior deltoid, and trapezius, potentially causing strains or contusions. Chest wall contusions can extend to rib fractures or costochondral separation in severe impacts. Abdominal seatbelt injuries include rectus abdominis and oblique muscle strains, with severe cases causing bowel or mesenteric injury (seatbelt syndrome). The characteristic diagonal bruise pattern appearing 24-48 hours post-accident is pathognomonic for seatbelt loading.
Airbag deployment generates unique injuries through rapid inflation (deploying at 200+ mph). Upper extremity injuries occur when hands are positioned on the steering wheel in improper positions (10-and-2 versus recommended 9-and-3), with airbag impact causing wrist extension injuries, forearm contusions, and finger dislocations. Facial and chest contusions result from airbag contact, occasionally causing ocular injuries if eyeglasses shatter. Chemical burns from airbag propellant (sodium azide) can occur, presenting as erythematous rash on contact areas.
Dashboard and interior impacts cause location-specific injuries: knee impact against dashboard produces quadriceps contusions, patellar injuries, and posterior cruciate ligament tears (dashboard knee). Shoulder impact against door frames causes rotator cuff strains and contusions. Hip and thigh contusions occur from center console or door panel impacts. These injuries often present with massive ecchymosis developing over 3-5 days.
Slip-and-fall accidents generate injuries based on landing position and protective reflexes: landing on an outstretched hand (FOOSH injury) causes wrist and forearm soft tissue injuries plus possible fractures. Lateral falls produce hip, shoulder, and lateral thigh contusions. Catching oneself during a fall creates eccentric muscle loading (muscle lengthening under tension), particularly affecting quadriceps, hamstrings, and rotator cuff, leading to Grade 2 strains.
Workplace accidents including repetitive motion create overuse injuries: rotator cuff tendinopathy in overhead workers (painters, electricians, construction), lateral epicondylitis (tennis elbow) in tool users requiring repetitive wrist extension (carpentry, assembly work), and medial epicondylitis (golfer's elbow) in gripping activities. These cumulative trauma injuries are compensable under Texas workers' compensation when work activities are the major contributing cause.
Direct trauma from being struck by objects, equipment, or during falls creates contusions with potential complications including compartment syndrome (elevated pressure within fascial compartments compromising perfusion) requiring emergency fasciotomy, traumatic rhabdomyolysis (muscle breakdown releasing myoglobin causing acute kidney injury), and myositis ossificans (heterotopic bone formation in healing muscle hematoma).
- Seatbelt trauma - diagonal chest/shoulder contusions, abdominal strains
- Airbag deployment - upper extremity contusions, wrist extension injuries
- Dashboard/interior impacts - knee contusions, quadriceps strains, shoulder injuries
- Slip-and-fall - FOOSH injuries, hip contusions, eccentric muscle loading
- Workplace repetitive motion - rotator cuff tendinopathy, epicondylitis
- Direct trauma - struck by objects causing contusions and possible compartment syndrome
- Sports-type injuries during accidents - sudden acceleration/deceleration strains
Soft tissue injury symptoms follow a characteristic temporal pattern useful for diagnosis and patient education. Immediate symptoms (0-6 hours) include pain at the injury site, often described as sharp or aching, worsening with movement or palpation. Muscle spasm or cramping develops as protective splinting. Swelling is typically minimal immediately post-injury unless significant vascular disruption occurred. Range of motion is reduced due to pain and protective guarding. Strength is decreased if muscle fibers are torn, though initial adrenaline and pain-mediated guarding can mask true weakness.
Delayed symptoms (24-72 hours) often exceed initial symptoms as inflammatory cascade peaks. Swelling becomes apparent as capillary permeability increases and inflammatory mediators accumulate. Ecchymosis (bruising) appears, typically 2-5 days post-injury, as extravasated blood dissects through tissue planes and breaks down. Bruise color evolution follows a predictable pattern: red-purple initially (oxyhemoglobin), blue-purple days 1-3 (deoxyhemoglobin), green days 4-6 (biliverdin), yellow-brown days 7+ (bilirubin and hemosiderin). Stiffness peaks in morning or after prolonged static postures as inflammatory exudate accumulates during immobility.
Functional limitations depend on injury location and severity: shoulder injuries impair overhead reaching, dressing, and hair grooming. Elbow and forearm injuries affect lifting, carrying, and keyboard use. Hip and quadriceps injuries impair stair climbing, rising from chairs, and squatting. Hamstring injuries affect walking speed, running, and bending. Seemingly minor soft tissue injuries can cause substantial functional impairment and work disability, particularly in labor-intensive occupations.
Chronic symptoms develop when acute injuries aren't properly rehabilitated: persistent weakness from inadequate strengthening allows compensatory movement patterns stressing other structures. Adhesions and scar tissue formation in healing muscle limits flexibility and creates pain with stretching. Tendinopathy develops from inadequately healed tendon undergoing repetitive loading before tissue remodeling completes. Chronic pain syndromes including myofascial pain with trigger points can perpetuate pain months to years after initial injury.
Physical examination reveals specific findings: palpable muscle spasm or taut bands, point tenderness at the injury site, possible palpable defect or gap in Grade 2-3 injuries, ecchymosis with characteristic distribution, reduced active range of motion (patient-initiated movement) out of proportion to passive range of motion (examiner moves limb—less limited as muscle activation not required), pain with resisted testing of specific muscle groups, and strength deficit quantified using manual muscle testing graded 0-5 (0=no contraction, 1=flicker, 2=movement with gravity eliminated, 3=movement against gravity only, 4=movement against some resistance, 5=normal strength).

| Symptom | Timing / Description |
|---|---|
| Pain at injury site | Immediate (0-6 hours) |
| Muscle spasm/cramping | Immediate (0-6 hours) |
| Reduced range of motion | Immediate (0-6 hours) |
| Decreased strength | Immediate (0-6 hours) |
| Swelling | Delayed (24-48 hours) |
| Ecchymosis (bruising) | Delayed (2-5 days) |
| Morning stiffness | Delayed (24-72 hours) |
| Functional limitations | Immediate to Chronic |
| Persistent weakness | Chronic (>6 weeks) |
| Trigger points | Chronic (>3 months) |
Soft tissue injury diagnosis relies heavily on clinical examination, with imaging serving a confirmatory role or ruling out associated bony injuries. Our systematic approach ensures accurate diagnosis and guides treatment selection.
Clinical examination begins with inspection noting ecchymosis distribution (diagonal across chest suggests seatbelt, localized suggests direct impact), swelling patterns, and visible deformities. Palpation identifies point tenderness, muscle spasm or taut bands, palpable defects or gaps suggesting complete tears, and temperature changes (warmth suggests active inflammation). Active and passive range of motion testing differentiates muscular limitation (active more limited than passive) from joint capsule restriction (both equally limited). Resisted strength testing isolates specific muscle groups: manual resistance applied while patient contracts muscle reproduces pain in injured muscle/tendon and reveals strength deficits graded 0-5.
Special tests target specific structures: for shoulder injuries, we perform empty can test (supraspinatus), drop arm test (supraspinatus tear), Hawkins-Kennedy test (impingement), and Speed's test (biceps tendon). For knee, we assess Lachman and anterior drawer (ACL), posterior drawer (PCL), varus and valgus stress (collateral ligaments), and McMurray's test (meniscus). For ankle, anterior drawer and talar tilt assess ligament integrity. Positive tests combined with mechanism and clinical presentation establish diagnosis.
Imaging selection follows clinical indication: Plain X-rays are initial imaging for any injury involving joint or bone proximity, ruling out fractures, dislocations, and foreign bodies. X-rays don't visualize soft tissue injuries directly but show secondary signs like joint effusion or soft tissue swelling. Ottawa rules guide ankle and knee X-ray necessity, reducing unnecessary imaging.
Ultrasound is excellent for superficial soft tissue evaluation including rotator cuff tears, Achilles tendon ruptures, patellar tendon tears, muscle tears with hematoma, and joint effusions. Ultrasound is real-time, allows dynamic assessment (imaging during movement), and is cost-effective. Limitations include operator dependence and limited depth penetration (not useful for deep structures like hip rotator cuff).
MRI provides definitive soft tissue imaging with superior contrast resolution, visualizing muscle tears, tendon tears (complete vs partial), ligament injuries, cartilage damage, bone marrow edema, and joint effusions. MRI is ordered when clinical examination suggests Grade 2 or 3 injury, surgical intervention is considered, or diagnosis remains unclear after examination and X-ray. For medico-legal cases, MRI provides objective documentation of injury severity.
CT scanning is reserved for complex fractures or when MRI is contraindicated (pacemaker, certain metal implants). CT arthrography (CT after intra-articular contrast injection) can evaluate cartilage and ligaments when MRI unavailable. Electrodiagnostic studies (EMG/NCS) are rarely needed for pure soft tissue injuries but can identify associated nerve injuries (brachial plexus injury with shoulder trauma, radial nerve injury with humeral fracture, peroneal nerve injury with knee dislocation).

Soft tissue injury treatment progresses through phases targeting inflammation reduction, pain control, tissue healing, and functional restoration. Our evidence-based protocols optimize recovery while preventing chronic dysfunction.
Phase 1 (Acute: Days 1-7) implements RICE protocol: Rest means activity modification avoiding pain-provoking movements, not complete immobilization which delays recovery. "Relative rest" maintains general activity while protecting injured tissue. Ice application (15-20 minutes every 2-3 hours) for first 48-72 hours reduces inflammation and pain through vasoconstriction and decreased metabolic rate. Compression with elastic bandages reduces swelling by preventing fluid accumulation—avoid excessive tightness compromising circulation. Elevation above heart level uses gravity to facilitate venous and lymphatic drainage.
Medication includes NSAIDs (ibuprofen 800mg TID or naproxen 500mg BID) for anti-inflammatory effect, though some evidence suggests NSAIDs may slightly impair early tendon healing—balance symptom relief against theoretical healing concerns. Acetaminophen provides analgesia without anti-inflammatory effect. Muscle relaxants (cyclobenzaprine, tizanidine) address secondary muscle spasm. Immobilization is used judiciously: slings for shoulder injuries during first 1-2 weeks, walking boots for ankle injuries, knee braces for ligament sprains—but prolonged immobilization (>2 weeks) causes muscle atrophy and joint stiffness, delaying recovery.
Phase 2 (Subacute: Weeks 1-6) introduces progressive rehabilitation. Physical therapy begins with gentle range of motion exercises, progressing from passive (therapist moves limb) to active-assisted (patient initiates movement with assistance) to active (patient performs independently). Early controlled motion prevents adhesions and maintains joint nutrition. Strengthening starts with isometric exercises (muscle contraction without joint movement), progressing to isotonic (movement through range with constant resistance) and finally isokinetic (movement at constant speed with variable resistance). Progressive resistance training rebuilds strength: initial loads at 50% of injured side strength, gradually increasing as tolerated. The contralateral limb often trains at higher resistance to maintain fitness and provide neuromuscular input via cross-education effect.
Manual therapy including soft tissue mobilization (massage techniques targeting specific tissues), myofascial release (sustained pressure releasing fascial restrictions), and trigger point therapy addresses secondary myofascial dysfunction. Therapeutic modalities include ultrasound therapy (high-frequency sound waves producing deep tissue heating, promoting blood flow and collagen extensibility), electrical stimulation (TENS for pain modulation, NMES for muscle re-education and preventing atrophy), and iontophoresis (using electrical current to drive anti-inflammatory medication transdermally).
Phase 3 (Intermediate: Weeks 6-12) emphasizes functional restoration. Sport/work-specific training incorporates movements and demands of patient's activities: plyometric exercises for athletes (explosive movements training muscle-tendon unit to store and release elastic energy), work simulation for injured workers (lifting, carrying, reaching tasks at progressively increasing loads), and activity-specific drills. Proprioceptive training on balance boards, foam pads, or single-leg stance improves neuromuscular control, reducing re-injury risk by up to 50% in ankle sprains.
Injection therapies for refractory cases include corticosteroid injections for inflamed tendons (though limited evidence for efficacy and concerns about tendon weakening—used selectively), PRP (platelet-rich plasma) showing promise for chronic tendinopathy and partial tendon tears by delivering growth factors promoting healing, and prolotherapy (injection of dextrose or other proliferants) theoretically stimulating healing response though evidence is mixed.
Phase 4 (Surgical: Rarely Needed) is reserved for complete ruptures of critical structures: rotator cuff complete tears in active patients (arthroscopic repair), Achilles tendon ruptures (open or percutaneous repair—surgery reduces re-rupture rates from 15% to <5% compared to conservative care), patellar tendon ruptures (primary surgical repair required for restoration of extensor mechanism), and severe ligament injuries like combined ACL/MCL tears. Post-surgical rehabilitation follows similar progressive loading principles but with timeline modifications protecting surgical repair during early healing (6-12 weeks protected motion, 3-6 months return to full activity).


Acute Phase (Days 1-7)
1-7 daysRICE protocol - Rest (relative), Ice (first 48-72h), Compression, Elevation. NSAIDs, activity modification. Brief immobilization if needed (1-2 weeks max).
Subacute Phase (Weeks 1-6)
1-6 weeksProgressive rehabilitation - range of motion (passive→active), progressive strengthening (isometric→isotonic→isokinetic), manual therapy, therapeutic modalities.
Intermediate Phase (Weeks 6-12)
6-12 weeksFunctional restoration - sport/work-specific training, plyometrics, proprioceptive training, PRP or injections if refractory. Return to activity progression.
Surgical Phase (If Needed)
Case dependentComplete ruptures of critical structures - rotator cuff, Achilles, patellar tendon, severe ligament tears. Followed by 3-6 month rehabilitation.
Soft tissue injury recovery varies by grade, location, and patient factors. Understanding expected timelines manages expectations and guides return-to-activity decisions.
Grade 1 (mild) strains typically resolve in 2-4 weeks with conservative care. Most patients achieve full pain-free function and return to pre-injury activities without restrictions by 3-4 weeks. Athletes can often continue training with modifications during recovery.
Grade 2 (moderate) strains require 6-12 weeks for substantial recovery. Pain decreases progressively but may persist at low levels for 2-3 months. Return to light duty work occurs at 4-6 weeks; return to heavy labor or competitive athletics at 8-12 weeks. Comprehensive rehabilitation is essential—inadequately rehabilitated Grade 2 injuries frequently progress to chronic tendinopathy or recurrent strains.
Grade 3 (severe/complete) tears demand 3-6 months for recovery, often including surgery. Post-surgical timelines vary by location: Achilles tendon repair allows weight-bearing in walking boot at 6-8 weeks, return to jogging at 4 months, return to sports at 6-9 months. Rotator cuff repair follows similar timeline: passive motion only for 6 weeks (protecting repair), active motion 6-12 weeks, strengthening 12+ weeks, return to overhead sports at 6-9 months. Surgical success rates are excellent when performed acutely but decline with delay—chronic tears develop muscle atrophy and fatty infiltration decreasing repair success and functional outcomes.
Contusions (bruises) without hematoma resolve in 2-4 weeks. Large intramuscular hematomas require 6-12 weeks, occasionally longer if myositis ossificans develops (heterotopic bone formation in 9-20% of large contusions, particularly in quadriceps). Myositis ossificans appears as firm mass palpable within muscle 3-6 weeks post-injury; X-rays show calcification. Treatment is conservative (NSAIDs, gentle stretching, avoid aggressive massage which may worsen) with gradual resolution over 6-12 months. Surgical excision is rarely needed for symptomatic cases after maturation.
Factors affecting recovery include age (younger patients heal faster), injury severity (higher grade = longer recovery), location (well-vascularized muscles heal faster than tendons and ligaments with limited blood supply), prior injuries (previously injured tissues more prone to recurrence), and rehabilitation compliance (consistent therapy adherence improves outcomes significantly). Smoking impairs healing through vasoconstriction and should be strongly discouraged.
Return-to-work criteria include pain-free or near-pain-free daily activities, strength ≥80% of contralateral side for light duty, ≥90% for moderate duty, ≥95% for heavy labor, ability to perform essential job functions without exacerbating injury, and clearance by treating physician. Functional capacity evaluations objectively document capabilities supporting return-to-work decisions.
Return-to-sport criteria are more stringent: full pain-free range of motion, strength ≥90% of contralateral side (>95% preferred), sports-specific functional testing passed (agility drills, jumping, cutting), and athlete psychologically ready. Premature return risks recurrent injury, often more severe than initial injury.
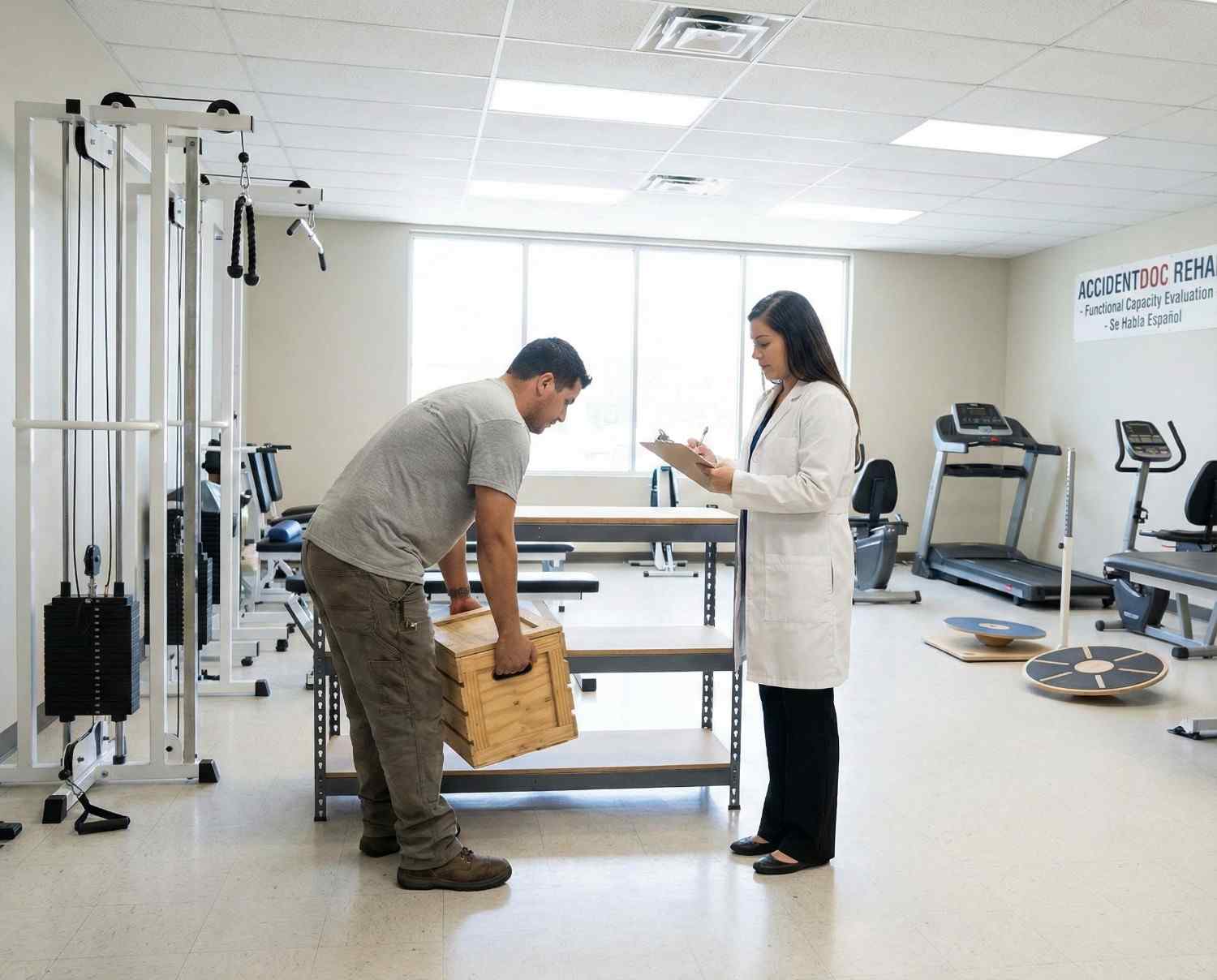
Soft tissue injuries present unique documentation challenges as they often lack dramatic imaging findings despite substantial pain and functional impairment. Thorough clinical documentation is essential for insurance claims and legal cases.
Mechanism documentation establishes causation: "Patient sustained Grade 2 pectoralis major strain when seatbelt loaded chest wall during sudden deceleration in rear-end collision on [DATE]. Physical examination reveals diagonal ecchymosis pattern across right chest consistent with seatbelt mechanism, palpable tenderness over pectoralis insertion, pain with resisted shoulder horizontal adduction, and 4/5 strength compared to 5/5 left side. Mechanism is consistent with and sufficient to cause observed injury."
Physical examination findings must be specific and quantified: "Right pectoralis major demonstrates 15×8 cm ecchymosis from clavicle to mid-chest. Point tenderness to palpation over sternal insertion. Palpable taut band in muscle belly. Active range of motion: shoulder flexion 110° (normal 180°), abduction 90° (normal 180°), internal rotation 45° (normal 70°). Strength testing: flexion 4+/5, abduction 4+/5, horizontal adduction 4/5 (pain-limited, normal 5/5 left). Negative impingement signs. Diagnosis: Grade 2 pectoralis major strain."
Imaging correlation: "Ultrasound right pectoralis major on [DATE] reveals hypoechoic region measuring 3.2×1.8 cm within mid muscle belly with increased vascularity on Doppler, consistent with Grade 2 intramuscular tear with associated hematoma. No complete fiber disruption. These findings correlate with clinical presentation."
Functional limitations documentation supports disability and damages claims: "Patient unable to perform essential job functions as automotive technician due to pectoralis strain. Job requires frequent overhead reaching, pushing/pulling of 25-50 lbs, and use of pneumatic tools creating vibration and resistance. Current restrictions: no lifting >15 lbs, no overhead work, no pushing/pulling >20 lbs. Patient cannot perform oil changes (overhead arm positioning), tire changes (torque wrench use), or brake work (sustained forceful pushing). Recommend light duty assignment if available; otherwise off work. Expected duration of restrictions: 8-12 weeks with comprehensive rehabilitation."
Causation opinion: "Within reasonable medical probability, patient's right pectoralis major strain is directly and proximately caused by the motor vehicle collision of [DATE]. The injury mechanism (seatbelt restraint causing eccentric loading during sudden deceleration) is consistent with the injury. The temporal relationship (symptoms developing immediately post-accident) supports causation. The diagonal ecchymosis pattern is pathognomonic for seatbelt loading. Patient had no prior history of pectoralis injury and was asymptomatic prior to accident."
Prognosis and future medical needs: "Patient prognosis is good for substantial recovery with appropriate rehabilitation. Expected timeline: 50% improvement by 4-6 weeks, 80% improvement by 8-10 weeks, maximum medical improvement at 3-4 months. Future medical needs include completion of physical therapy (estimated 12-16 sessions), possible ultrasound-guided injection if plateau at 8 weeks, and 5-10% risk of chronic pain requiring ongoing intermittent treatment. Permanent partial impairment rating expected at 0-5% upper extremity impairment (converts to 0-3% whole person). No permanent restrictions anticipated for sedentary work; possible permanent restrictions for heavy overhead labor."
- Detailed mechanism documentation with injury causation correlation
- Specific physical examination findings with measurements and functional testing
- Imaging correlation when available (ultrasound, MRI)
- Functional limitations and work restrictions with job-specific analysis
- Causation opinion stated within reasonable medical probability
- Treatment plan with medical necessity justification
- Prognosis with expected recovery timeline
- Future medical needs and estimated costs
- Disability ratings at maximum medical improvement if permanent impairment
While most soft tissue injuries are managed conservatively, certain presentations indicate serious complications requiring emergency evaluation.
Compartment syndrome occurs when pressure within a fascial compartment (containing muscles, nerves, vessels) exceeds perfusion pressure, causing ischemia and potential permanent damage. It develops after severe contusions, crush injuries, or fractures. Classic presentation is "6 P's": Pain out of proportion to injury and worsening despite treatment, Pressure (tense, swollen compartment), Paresthesias (numbness/tingling), Pallor (pale skin), Pulselessness (late finding—irreversible damage likely occurred), Paralysis (late finding). Pain with passive stretching of muscles in affected compartment is the most sensitive early sign. Compartment syndrome is a surgical emergency requiring immediate fasciotomy (incising fascia to release pressure). Any patient with severe contusion and worsening pain, especially if pain with passive stretching develops, requires immediate emergency evaluation with compartment pressure measurement.
Vascular injury with diminished or absent pulses, pale or cool extremity, or expanding hematoma suggests arterial injury requiring immediate vascular surgery consultation. Nerve injury with severe neurological deficits (complete motor/sensory loss) may require surgical exploration and repair. Open wounds with exposed tendon or muscle require emergent irrigation and repair—contamination risk demands antibiotic prophylaxis and tetanus update.
Signs of infection including fever, spreading erythema, warmth, purulent drainage, or red streaking (lymphangitis) warrant immediate evaluation as soft tissue infections can progress rapidly to necrotizing fasciitis, a life-threatening emergency. Patients with large ecchymosis should be monitored for signs of rhabdomyolysis including dark urine (myoglobinuria), decreased urine output, and systemic symptoms—severe cases require hospitalization for IV hydration preventing acute kidney injury.
- Compartment syndrome - Pain out of proportion, tense swelling, pain with passive stretch
- Paresthesias or paralysis developing after injury
- Pulselessness, pallor, or cool extremity (vascular injury)
- Expanding hematoma or uncontrolled bleeding
- Open wound with exposed tendon or muscle
- Fever with spreading redness or purulent drainage (infection)
- Dark urine after severe muscle injury (rhabdomyolysis)
- Chest/abdominal pain after seatbelt injury (internal organ injury)
- Severe pain unrelieved by any intervention
While accidents are often unpredictable, strategies reduce soft tissue injury severity and promote recovery. Proper seatbelt positioning (shoulder belt across clavicle and chest, lap belt across pelvis) distributes forces optimally. Strengthening programs particularly for workers in physical occupations build resilience: rotator cuff strengthening for overhead workers, core and lower extremity strengthening for material handlers. Proper warm-up before physical activity increases muscle temperature and flexibility, reducing strain risk. Post-injury, gradual return to activity following rehabilitation prevents recurrence—studies show inadequately rehabilitated injuries recur at rates exceeding 50%. Maintaining healthy body weight, smoking cessation, and adequate protein intake (0.8-1.0 g/kg bodyweight, higher during healing) support tissue health and repair. Ergonomic modifications and assistive devices reduce workplace injury risk.
Seek Emergency Care Immediately If You Experience:
- Compartment syndrome - severe pain, tense swelling, pain with passive muscle stretching
- Paresthesias (numbness/tingling) or paralysis developing after injury
- Diminished or absent pulses, pale or cool extremity (vascular injury)
- Expanding hematoma or uncontrolled bleeding
- Open wound with exposed muscle, tendon, or bone
- Fever, spreading redness, purulent drainage (infection)
- Dark or tea-colored urine after crush injury (rhabdomyolysis)
- Chest or abdominal pain after seatbelt injury (internal organs)
- Severe unrelenting pain despite medication and ice
Call 911 or go to the nearest emergency room immediately

Traumatic brain injuries (TBI), including concussions, affect over 2.8 million Americans annually, with motor vehicle accidents representing the leading cause among adults. Concussions are complex neurometabolic injuries affecting brain function without necessarily showing structural damage on standard imaging. At AccidentDoc Pasadena, our board-certified physicians specialize in comprehensive concussion evaluation and evidence-based treatment protocols, from acute management through post-concussion syndrome recovery. Early diagnosis and proper treatment prevent long-term cognitive impairment and accelerate return to normal function.
A concussion is a mild traumatic brain injury (mTBI) resulting from biomechanical forces transmitted to the brain, causing a complex neurometabolic cascade without necessarily producing structural injury visible on CT or standard MRI. Understanding the injury mechanism is critical for recognizing concussions that might otherwise go undiagnosed and untreated.
The brain consists of approximately 86 billion neurons suspended in cerebrospinal fluid within the rigid skull. During sudden acceleration-deceleration or rotational forces—common in car accidents—the brain moves within the skull despite CSF cushioning, creating strain on neural tissue, blood vessels, and axonal connections. This movement occurs in two phases: the coup injury where the brain impacts the skull at the point of force application, and the contrecoup injury where the brain rebounds and impacts the opposite skull surface. Rotational acceleration, where the head twists suddenly, creates the most severe shearing forces on axons, particularly at gray-white matter junctions where tissue density differences create maximal strain.
At the cellular level, concussion triggers a neurometabolic cascade: mechanically-stressed neurons release excessive excitatory neurotransmitters, particularly glutamate, causing ionic flux (potassium efflux, calcium influx). This ionic imbalance forces energy-dependent sodium-potassium pumps to work overtime, depleting ATP (adenosine triphosphate) stores when mitochondrial function is simultaneously impaired by calcium overload. The result is an energy crisis where neurons require increased glucose while cerebral blood flow is paradoxically reduced, creating a mismatch between supply and demand. This metabolic dysfunction typically lasts 7-10 days in uncomplicated concussions but can persist weeks to months in severe cases or repeat injuries.
Axonal injury occurs through mechanical shearing and secondary metabolic dysfunction: the disruption of microtubules and neurofilaments impairs axonal transport, causing accumulation of proteins and eventual axonal disconnection. Diffuse axonal injury (DAI) represents the severe end of this spectrum and can occur even without loss of consciousness. Research using advanced neuroimaging including diffusion tensor imaging (DTI) demonstrates that structural axonal injury exists in many "mild" concussions, explaining persistent symptoms despite normal CT scans.
The brain regions most vulnerable to concussion injury include the prefrontal cortex (executive function, impulse control), temporal lobes (memory formation), corpus callosum (interhemispheric communication), and brainstem centers regulating autonomic function. This explains the constellation of cognitive, emotional, and autonomic symptoms characterizing concussion. The developing adolescent brain is particularly vulnerable due to ongoing myelination and synaptic pruning, while elderly brains with age-related atrophy have more space for brain movement within the skull, paradoxically increasing injury risk.
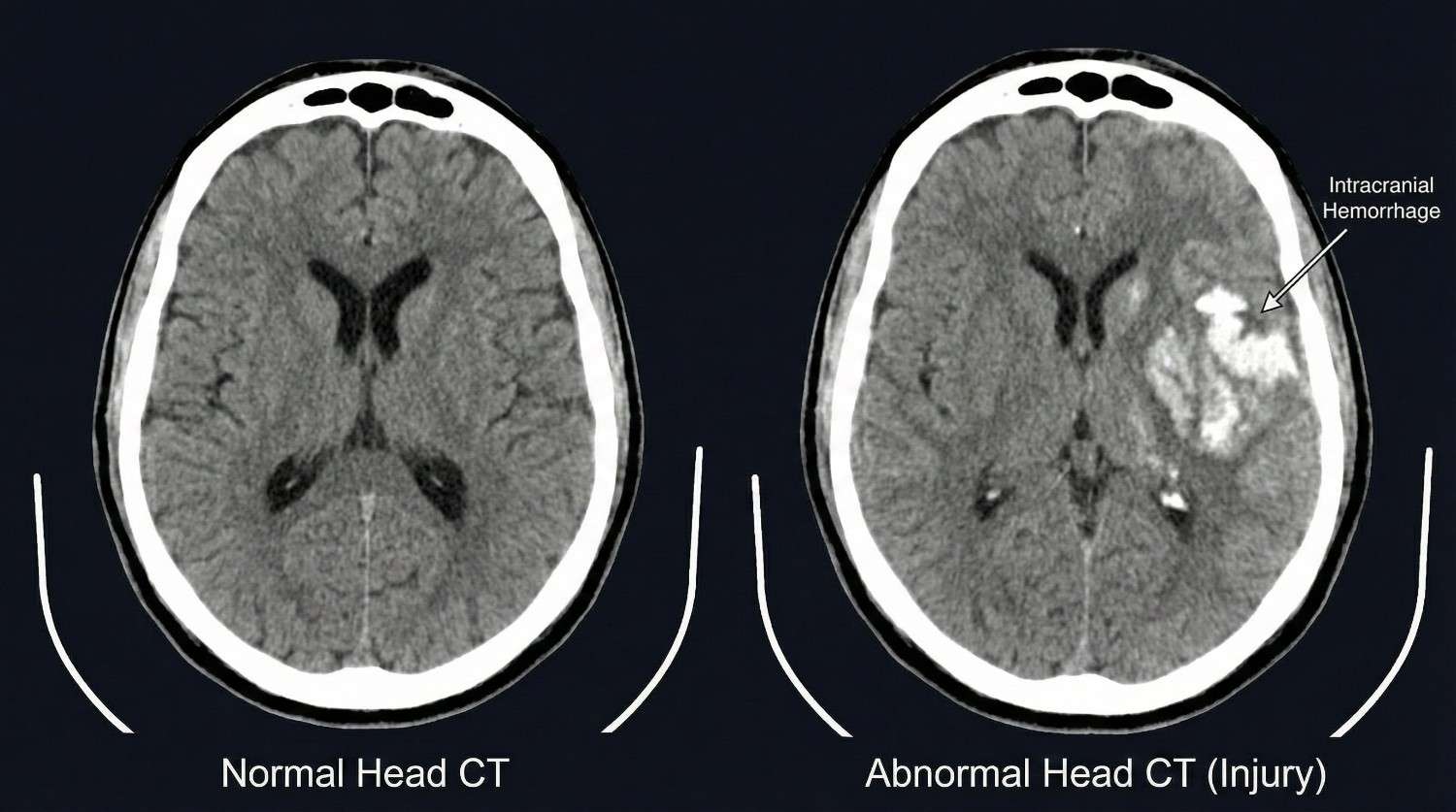
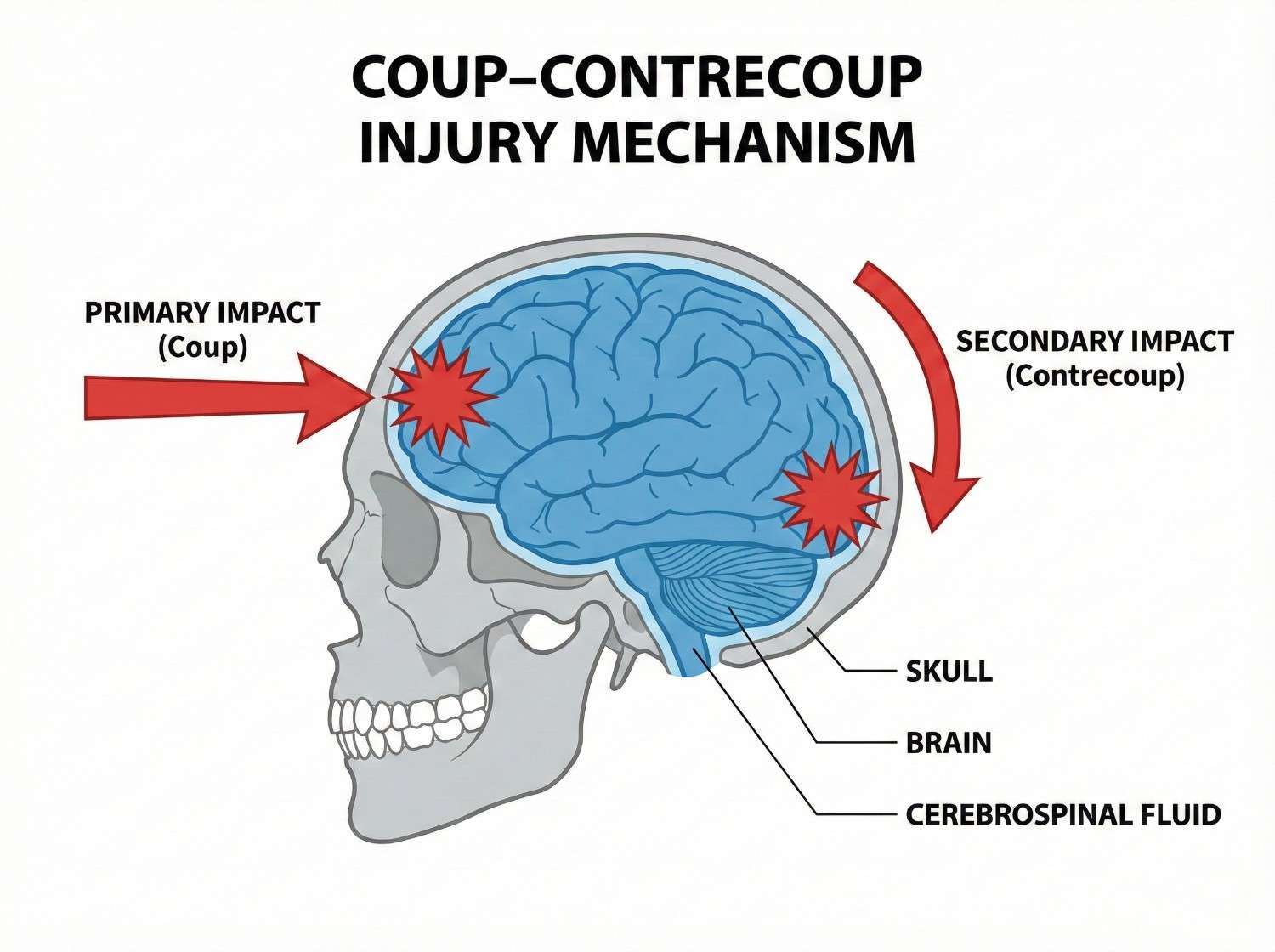
Motor vehicle accidents are the leading cause of traumatic brain injury among adults aged 20-60, accounting for approximately 50% of TBI-related emergency department visits in this demographic. Rear-end collisions produce rapid head acceleration-deceleration: the torso accelerates forward with the seat while the head initially lags (inertia), then snaps forward as neck muscles contract and anterior structures limit extension. This whiplash-type mechanism can cause concussion even without direct head impact, as the brain moves within the skull. Frontal collisions create the reverse mechanism, with airbag deployment sometimes contributing additional impact force to the head, particularly if the occupant is unrestrained or improperly positioned.
Side-impact collisions generate rotational acceleration, the most damaging force for brain tissue. The head rotates suddenly as it's struck by the window, B-pillar, or intruding vehicle structure, creating maximal shearing strain on axons at gray-white matter junctions. Side impacts produce higher concussion rates than frontal or rear collisions of equivalent severity due to these rotational forces. Rollover accidents combine all force vectors—linear, rotational, and vertical—often with multiple impacts as the vehicle rotates, producing severe TBI including both concussion and more serious intracranial hemorrhage.
Pedestrian-vehicle collisions create unique injury patterns: the initial vehicle impact, fall to ground surface (often striking the head on pavement), and sometimes secondary impact from being run over by the vehicle. The unrestrained pedestrian experiences full-body acceleration without protection, frequently resulting in moderate to severe TBI. In the Pasadena and Houston area, pedestrian accidents along high-traffic corridors like Highway 225, Fairmont Parkway, and Red Bluff Road represent significant sources of severe head trauma.
Slip-and-fall accidents, particularly common in retail, restaurant, and workplace settings, cause head injury when the victim strikes their head during the fall or when the head impacts the ground. Falls onto hard surfaces like concrete, tile, or metal grating create high-impact forces despite relatively low falling heights—a fall from standing height can generate 500+ Gs of deceleration when the head strikes concrete. Elderly patients with osteoporosis, balance disorders, or anticoagulation are particularly vulnerable to severe TBI from falls, with subdural hematomas common even from seemingly minor impacts.
Workplace accidents in Pasadena's industrial sector include being struck by falling objects (pipes, tools, equipment), scaffolding collapses, falls from height in construction and refinery work, and blast injuries in petrochemical facilities. Hard hat use reduces but doesn't eliminate concussion risk—the helmet prevents skull fractures but doesn't fully eliminate the internal brain movement causing concussion. Confined space accidents with oxygen deprivation can cause global hypoxic brain injury combined with traumatic injury if the worker collapses and strikes their head.
Assault-related head injuries from physical altercations include direct blows to the head and injuries sustained during falls after being struck. Sports and recreation injuries, while less common in our accident-focused practice, do occur and include cycling accidents without proper helmet use, ATV rollovers, and boating accidents.
- Rear-end collisions - acceleration-deceleration without direct impact (coup-contrecoup)
- Frontal collisions with airbag deployment - combined mechanism
- Side-impact collisions - rotational forces (most dangerous mechanism)
- Rollover accidents - multiple impacts, all force vectors
- Pedestrian-vehicle collisions - multiple injury phases
- Slip-and-fall - head impact on hard surfaces
- Workplace struck-by injuries - falling objects, scaffolding collapses
- Falls from height - construction, ladder, refinery work
- Assault - direct blows and fall-related head impact
Concussion symptoms are organized into four clusters—physical, cognitive, emotional, and sleep-related—with temporal patterns critical for diagnosis and management. Understanding the full symptom spectrum is essential because concussions often lack visible external injury, and patients may not immediately recognize they've sustained a brain injury.
Immediate physical symptoms (0-24 hours) include headache (present in 85-90% of concussions), often described as pressure-like or throbbing, typically generalized or frontal. Dizziness or vertigo occurs in 50-70% of patients, reflecting vestibular system dysfunction or cervical proprioceptor injury. Visual disturbances include blurred vision, difficulty focusing, sensitivity to light (photophobia), and diplopia (double vision). Nausea or vomiting results from brainstem autonomic dysfunction or vestibular disruption. Balance problems and unsteady gait are common, detectable on objective testing like tandem stance or Balance Error Scoring System (BESS). Sensitivity to noise (phonophobia) reflects auditory processing dysfunction. Immediate loss of consciousness (LOC) occurs in only 10-15% of concussions—its absence doesn't rule out concussion.
Immediate cognitive symptoms include confusion or feeling "in a fog," disorientation to time, place, or situation, amnesia for the event (retrograde amnesia) or period after the event (anterograde amnesia), slowed reaction time, and difficulty concentrating. Patients may ask repetitive questions, showing impaired short-term memory formation. Confusion severity doesn't correlate perfectly with injury severity—brief LOC with rapid return to normal orientation may indicate less severe injury than prolonged confusion without LOC.
Delayed symptoms (24 hours to 2 weeks) often exceed initial symptoms as the metabolic crisis persists and patients return to cognitive demands. Headaches may worsen or change character, sometimes evolving into post-traumatic migraine with throbbing pain, photophobia, and phonophobia. Cognitive difficulties become more apparent: impaired concentration and attention particularly noticeable when returning to work, short-term memory problems affecting daily activities, mental fogginess described as "wading through water," slowed processing speed making tasks take longer, and executive function deficits affecting planning, organization, and multitasking. These cognitive symptoms worsen with mental exertion, a phenomenon called cognitive fatigue unique to concussion.
Emotional symptoms emerge as patients struggle with functional limitations: irritability and mood changes, anxiety particularly about cognitive deficits, depression from loss of function and quality of life, emotional lability with inappropriate crying or emotional reactions, and personality changes noticed by family members before patients recognize them. These aren't simply psychological reactions to injury—they reflect actual neurophysiological changes in frontal lobe and limbic system function.
Sleep disturbances are nearly universal: initial hypersomnia (excessive sleeping) in the first week as the brain attempts recovery, followed by insomnia with difficulty falling or staying asleep, disrupted sleep architecture with reduced REM sleep, and daytime fatigue despite adequate sleep hours. Sleep disturbance both results from and worsens concussion recovery, creating a challenging cycle.
Post-concussion syndrome (PCS) develops when symptoms persist beyond expected recovery (>4 weeks in adults, >4-6 weeks in adolescents). PCS affects 10-15% of concussion patients, with risk factors including previous concussions, female gender, younger age, high initial symptom burden, early return to activity, and psychiatric history. PCS symptoms mirror acute concussion but with greater functional impairment and treatment resistance. Some patients develop chronic PCS lasting months to years, requiring comprehensive multidisciplinary treatment.
Symptom exacerbation with activity is a key diagnostic feature: physical exertion, cognitive effort (screen time, reading, problem-solving), and sensory stimulation (bright lights, loud environments) all provoke symptom worsening, distinguishing concussion from other headache disorders or psychological conditions. This symptom provocation guides return-to-activity protocols.
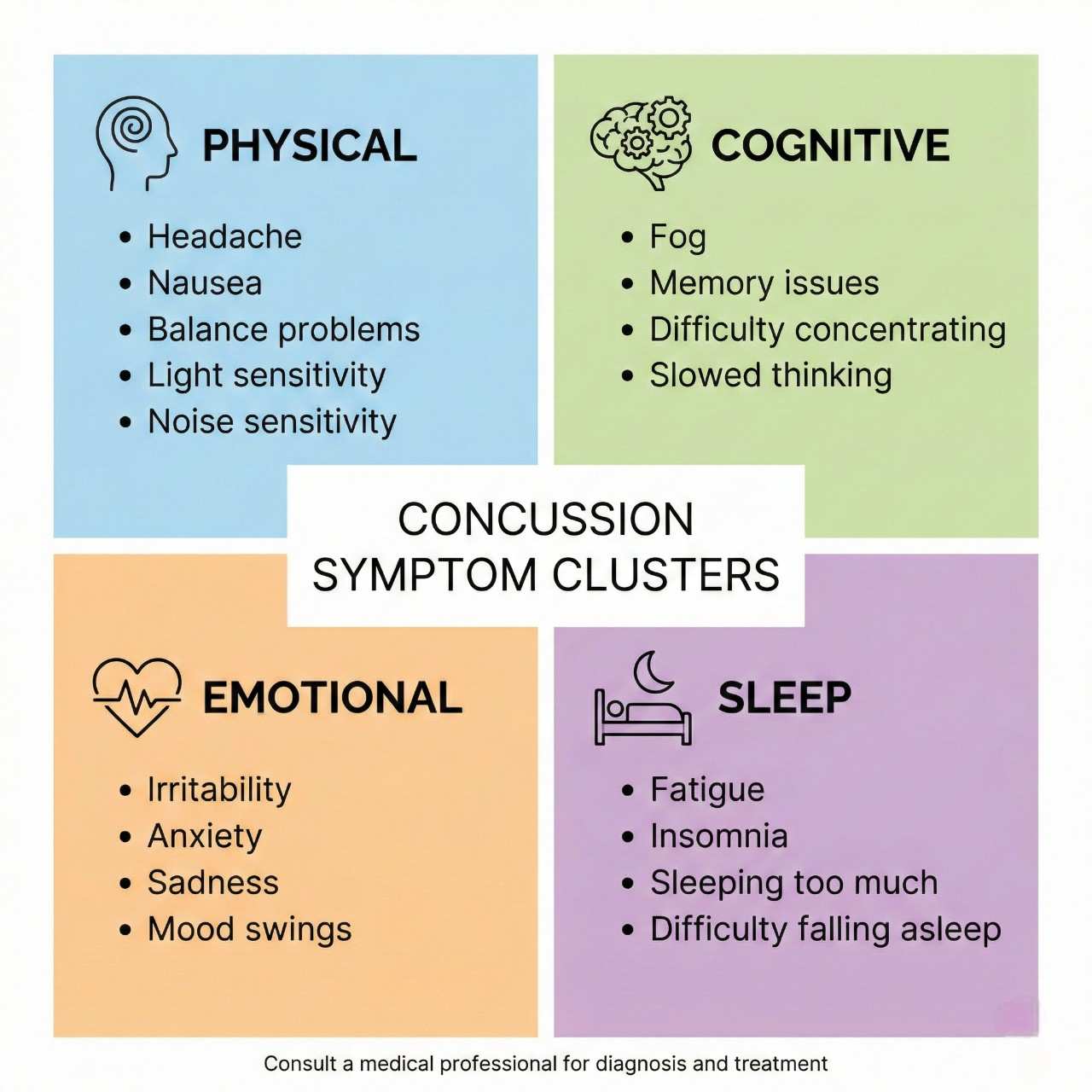
| Symptom | Timing / Description |
|---|---|
| Headache | Immediate (0-24 hours) |
| Dizziness or vertigo | Immediate (0-24 hours) |
| Visual disturbances | Immediate (0-24 hours) |
| Nausea or vomiting | Immediate (0-24 hours) |
| Balance problems | Immediate (0-24 hours) |
| Confusion or "fogginess" | Immediate (0-24 hours) |
| Amnesia | Immediate (0-24 hours) |
| Cognitive difficulties | Delayed (24hrs-2 weeks) |
| Emotional changes | Delayed (24hrs-2 weeks) |
| Sleep disturbances | Immediate to Chronic |
| Post-concussion syndrome | Chronic (>4 weeks) |
| Cognitive fatigue | Delayed to Chronic |
Concussion diagnosis is primarily clinical, based on mechanism of injury, symptom presentation, and structured examination, as standard imaging often appears normal in concussion despite significant functional impairment. Our comprehensive diagnostic approach identifies all injury components and guides treatment selection.
Initial evaluation documents injury mechanism in detail: type of accident, direction and estimated magnitude of forces, whether the head struck an object (direct impact) or the brain moved within the skull without contact (indirect mechanism), immediate symptoms including any LOC duration, and witness observations. This narrative establishes causation for legal documentation.
Structured symptom assessment uses validated tools including the Sport Concussion Assessment Tool 5th Edition (SCAT5) for adults and Child SCAT5 for patients under 13. The SCAT5 documents 22 symptoms across physical, cognitive, emotional, and sleep domains, each scored 0-6 for severity. This quantification allows objective tracking of recovery. Baseline testing, when available from pre-injury evaluations, provides invaluable comparison, though most accident victims lack pre-injury data.
Physical examination assesses multiple domains: Neurological examination includes cranial nerve testing (visual fields, pupillary reflexes, extraocular movements, facial symmetry, hearing, palatal elevation, tongue movement), motor function with strength testing of all major muscle groups, sensory examination for deficits, deep tendon reflexes comparing symmetry, and cerebellar testing (finger-to-nose, heel-to-shin, rapid alternating movements). Abnormalities suggest more severe TBI or structural injury.
Vestibular and balance testing objectively quantifies common concussion deficits: Balance Error Scoring System (BESS) tests three stances (double leg, single leg, tandem) on firm and foam surfaces with eyes closed, counting errors over 20 seconds. Concussed patients show significantly more errors than healthy controls. Vestibular ocular motor screening (VOMS) assesses smooth pursuits, saccades, convergence, and vestibular-ocular reflex (VOR), with symptoms provoked by these maneuvers indicating vestibular dysfunction. Dix-Hallpike maneuver tests for benign paroxysmal positional vertigo (BPPV), common after head trauma.
Cognitive screening uses validated tools: Montreal Cognitive Assessment (MoCA) screens for deficits in attention, executive function, memory, language, and visuospatial skills. Scores <26/30 indicate impairment. Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) is a computerized battery measuring verbal and visual memory, processing speed, and reaction time. While baseline testing is ideal, normative data allows interpretation of post-injury scores. Deficits correlate with symptom severity and predict recovery duration.
Cervical spine examination is critical as whiplash commonly accompanies concussion: cervical range of motion measurement, palpation for vertebral and facet tenderness, upper extremity neurological examination, and Spurling's test for radiculopathy. Cervicogenic headache from concurrent neck injury can complicate concussion management.
Imaging selection follows evidence-based indications: Head CT without contrast is the initial study for moderate to severe TBI or when intracranial hemorrhage is suspected. Indications include Glasgow Coma Scale (GCS) <15, focal neurological deficits, severe persistent headache, repeated vomiting (>2 episodes), seizure, amnesia >30 minutes, dangerous mechanism (high-speed collision, fall >3 feet, pedestrian struck), age >65, or anticoagulation use. CT identifies skull fractures, epidural hematomas, subdural hematomas, subarachnoid hemorrhage, intracerebral hemorrhage, and cerebral contusions requiring neurosurgical consultation. However, CT is often normal in concussion, as the injury is primarily metabolic and functional rather than structural.
MRI brain is more sensitive for subtle structural injury but rarely changes acute management. We order MRI for persistent symptoms beyond 4-6 weeks, atypical symptom progression, focal neurological deficits with negative CT, or suspicion of diffuse axonal injury. Susceptibility-weighted imaging (SWI) and diffusion tensor imaging (DTI) detect microhemorrhages and axonal injury not visible on standard MRI sequences, though these advanced techniques are primarily research tools currently.
Cervical spine imaging (X-rays or MRI) is obtained when neck pain persists or radicular symptoms develop, as concurrent cervical injury affects treatment planning. Neuropsychological testing provides comprehensive cognitive assessment when ImPACT or MoCA suggest deficits, evaluating attention, memory, executive function, processing speed, and emotional functioning. This testing guides cognitive rehabilitation and documents disability for legal proceedings.
Electroencephalography (EEG) is reserved for suspected post-traumatic seizures, not routine concussion evaluation. Blood biomarkers including S100B protein and glial fibrillary acidic protein (GFAP) show promise for concussion diagnosis but aren't yet standard clinical practice. This comprehensive evaluation ensures accurate diagnosis while identifying structural injuries requiring urgent intervention.
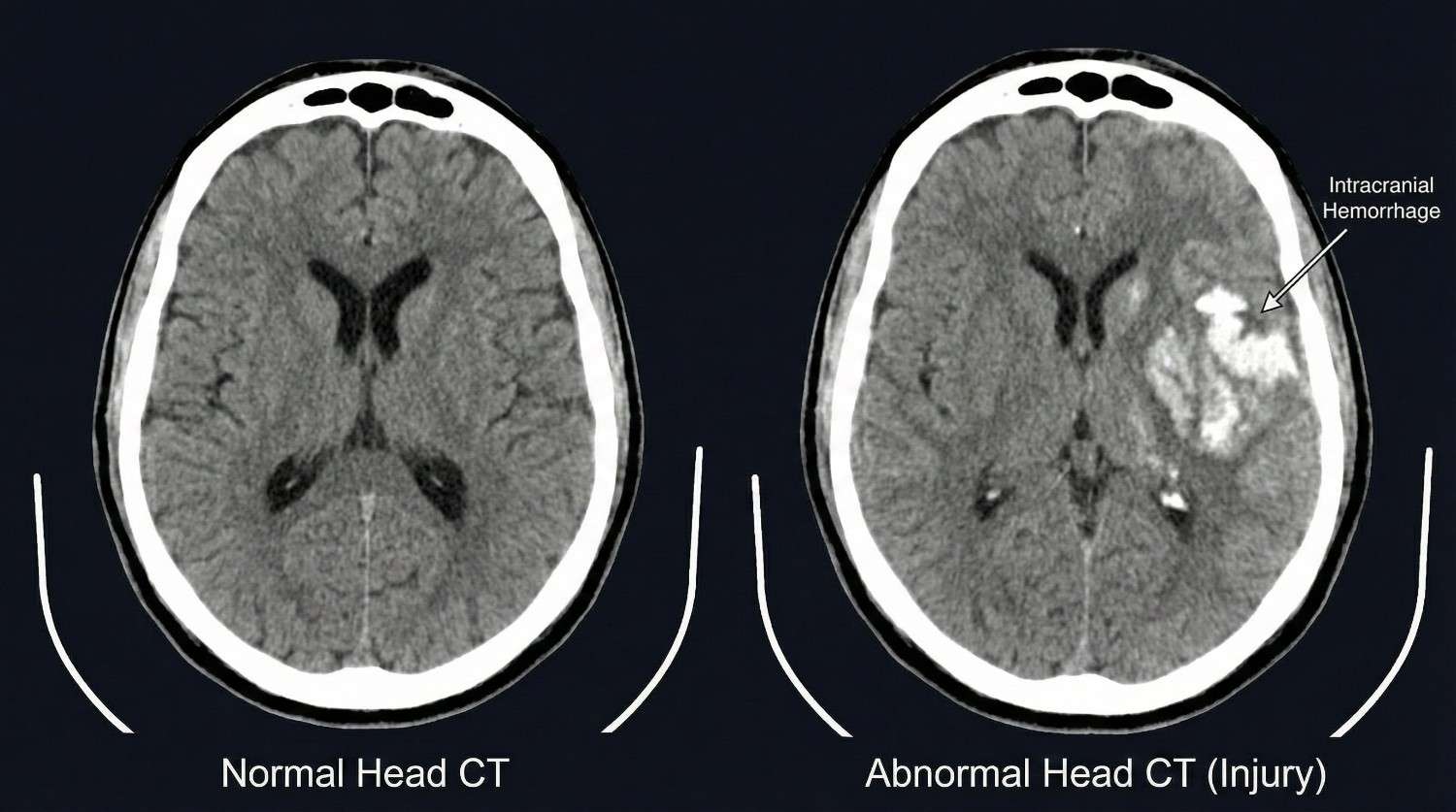

Modern concussion treatment has evolved from prolonged rest in dark rooms to active rehabilitation protocols that optimize recovery while preventing post-concussion syndrome. Our evidence-based approach progresses through phases based on symptom severity and patient response. All treatment is available through Letter of Protection with $0 upfront cost.
Phase 1 (Acute Rest Phase: Days 1-3) emphasizes brief initial rest to allow the neurometabolic crisis to stabilize, but not prolonged inactivity which delays recovery. We recommend 24-48 hours of relative cognitive and physical rest: limiting screen time (phones, computers, television) to <30 minutes at a time, avoiding reading or activities requiring sustained concentration, taking frequent breaks during necessary activities, and avoiding physically demanding activities. However, light activity is encouraged—short walks, light household tasks—as complete bedrest impairs recovery. Sleep optimization is prioritized: maintaining regular sleep schedule, creating dark quiet sleep environment, and avoiding caffeine after noon. Many patients naturally require increased sleep (12-14 hours) in the first few days; this should be allowed.
Symptom management includes analgesics for headache: acetaminophen (Tylenol) is first-line, as NSAIDs theoretically increase bleeding risk in the acute phase, though this risk is likely minimal. If headaches persist beyond 3-4 days, we prescribe migraine-specific medications including triptans (sumatriptan, rizatriptan) for severe headaches, or preventive medications for frequent headaches. Anti-nausea medications (ondansetron, promethazine) address persistent nausea. We avoid opioids and benzodiazepines due to cognitive effects that impair assessment and recovery.
Vestibular symptoms are managed with vestibular suppressants (meclizine) for acute severe vertigo, though these are limited to 2-3 days to avoid delaying central compensation. Canalith repositioning maneuvers (Epley maneuver) treat post-traumatic BPPV if Dix-Hallpike testing is positive.
Phase 2 (Graduated Return to Activity: Days 4-14) introduces progressive activity following the Berlin Consensus Statement on Concussion in Sport guidelines. The protocol includes six stages with 24-hour minimum intervals between stages, advancing only if symptoms don't worsen: Stage 1 (days 1-3): Daily activities that don't provoke symptoms, limited physical and cognitive activity. Stage 2 (days 4-5): Light aerobic exercise—walking, stationary cycling at <70% maximum heart rate for 10-15 minutes. Purpose: increase heart rate without symptom provocation. Stage 3 (days 6-8): Sport-specific exercise without contact—moderate intensity aerobic activity, beginning sport-specific drills. Stage 4 (days 9-11): Non-contact training drills with increased cognitive load—more complex drills, resistance training. Stage 5 (days 12-14): Full-contact practice—after medical clearance, participate in normal training. Stage 6 (day 15+): Return to full activity without restrictions.
This graduated protocol applies to work, school, and physical activity. Cognitive exertion is similarly graduated: initial 30-minute blocks of work or school with breaks, progressively increasing to half-days, then full days as tolerated. Importantly, patients should operate at 80-90% of symptom threshold—mild symptom provocation is acceptable and facilitates recovery, but severe symptom exacerbation requires dropping back to the previous stage.
Phase 3 (Active Rehabilitation: Weeks 2-8) addresses persistent symptoms with targeted interventions. Vestibular rehabilitation therapy is critical for balance and dizziness problems, utilizing habituation exercises (repeated exposure to symptom-provoking movements to facilitate central compensation), gaze stabilization exercises (VOR exercises improving visual stability during head movement), and balance training progressing from stable to unstable surfaces. Studies show 80% of patients with persistent vestibular symptoms improve with vestibular therapy.
Cervical spine treatment addresses concurrent whiplash using physical therapy, chiropractic manipulation, and soft tissue therapy. Cervicogenic headache responds to cervical treatments often better than traditional headache medications. Vision therapy addresses convergence insufficiency (difficulty focusing on near objects) and smooth pursuit or saccade dysfunction affecting reading. Accommodative exercises and vergence therapy improve visual function.
Cognitive rehabilitation for persistent cognitive deficits uses attention training, memory strategy development, compensatory strategy training (external memory aids, organizational systems), and graduated return to work/school with accommodations (extended test time, reduced workload, frequent breaks). Neuropsychologist-guided rehabilitation optimizes outcomes.
Exercise therapy using sub-symptom threshold aerobic exercise (Buffalo Concussion Treadmill Test protocol) demonstrates both diagnostic and therapeutic value: patients exercise to symptom exacerbation, identifying heart rate threshold, then train daily at 80% of threshold heart rate for 20 minutes. This improves autonomic dysregulation and accelerates recovery. Studies show patients using this protocol recover 1-2 weeks faster than standard rest protocols.
Phase 4 (Advanced Interventions: Weeks 8-24) treats persistent post-concussion syndrome with specialized procedures. Greater occipital nerve blocks deliver local anesthetic and corticosteroid to the occipital nerves for cervicogenic and occipital headaches, providing 4-8 weeks of relief and allowing advancement of rehabilitation. Trigger point injections address myofascial pain in cervical, suboccipital, and temporalis muscles contributing to headache. Stellate ganglion blocks show emerging evidence for treating autonomic dysfunction and cognitive symptoms in chronic PCS, modulating sympathetic nervous system dysregulation.
Pharmacological management for specific persistent symptoms includes: amitriptyline or nortriptyline (tricyclic antidepressants) for post-traumatic headache and sleep disturbance; topiramate for headache prophylaxis; methylphenidate for attention and processing speed deficits (used cautiously); selective serotonin reuptake inhibitors (SSRIs) for depression and anxiety; and melatonin for sleep cycle normalization. Medications are selected based on symptom profile and comorbidities.
Psychological support addresses emotional symptoms and teaches coping strategies: cognitive-behavioral therapy (CBT) for anxiety and depression, relaxation techniques and mindfulness training for stress management, and sleep hygiene education. The multidisciplinary approach combining physical rehabilitation, cognitive therapy, and psychological support achieves the best outcomes for complex PCS.

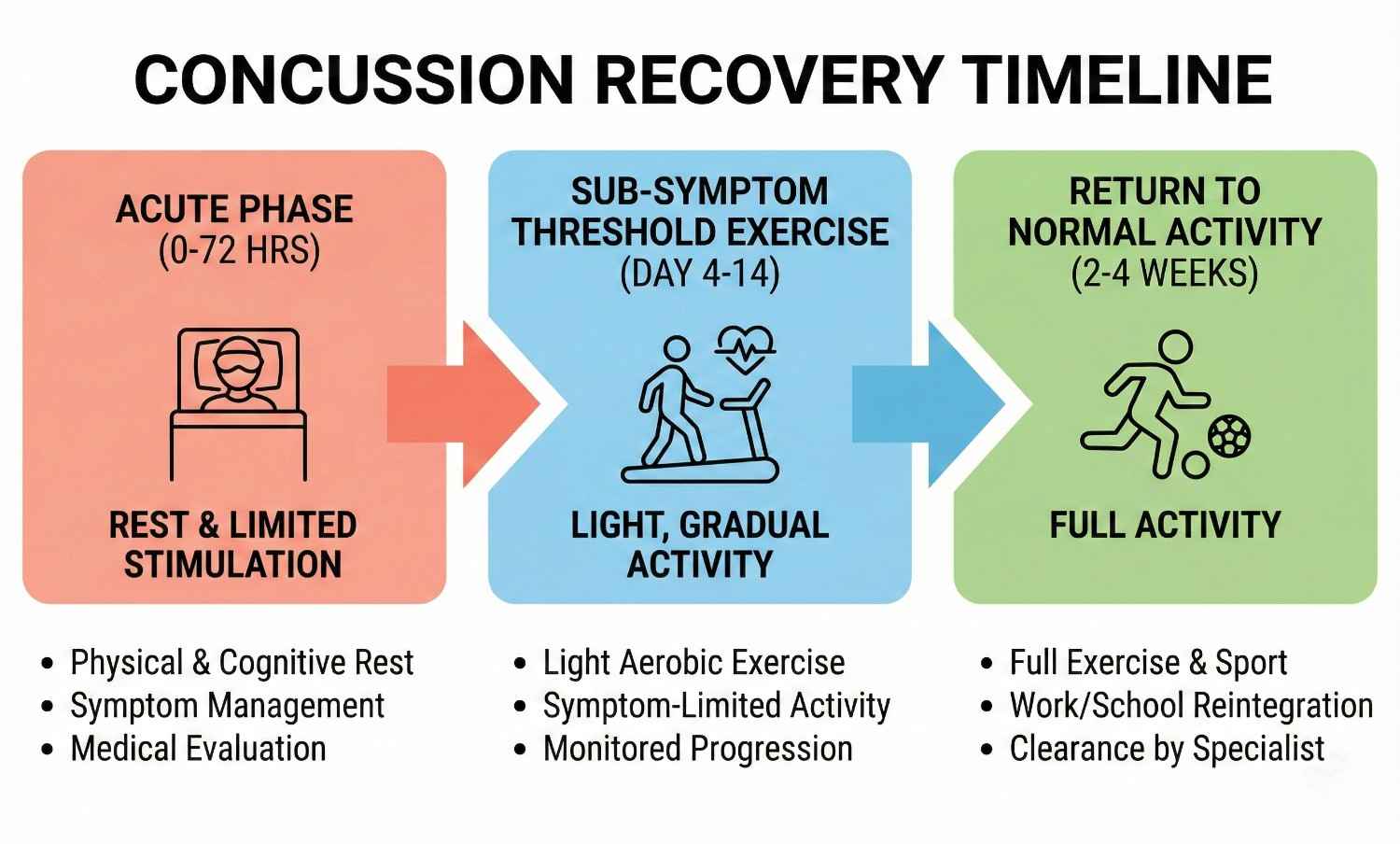
Acute Rest Phase (Days 1-3)
1-3 daysBrief relative rest (24-48 hours), limited screen time and cognitive activity, sleep optimization, symptom management with acetaminophen, anti-nausea medications. Light physical activity encouraged.
Graduated Return to Activity (Days 4-14)
4-14 daysProgressive six-stage protocol: light aerobic exercise, sport-specific drills, non-contact training, full-contact practice, return to full activity. Advance every 24 hours if asymptomatic. Cognitive activity similarly graduated.
Active Rehabilitation (Weeks 2-8)
2-8 weeksVestibular rehabilitation, cervical spine treatment, vision therapy, cognitive rehabilitation, sub-symptom threshold aerobic exercise training. Addresses persistent symptoms.
Advanced Interventions (Weeks 8-24+)
8-24+ weeksOccipital nerve blocks, trigger point injections, stellate ganglion blocks, pharmacological management, psychological support. For post-concussion syndrome and chronic symptoms.
Concussion recovery follows variable timelines influenced by injury severity, patient age, concussion history, and treatment adherence. Understanding expected recovery patterns helps patients maintain realistic expectations and clinicians identify complicated courses requiring advanced intervention.
Uncomplicated concussion in adults typically resolves within 7-14 days, with 80-90% of patients recovering fully by two weeks. Symptom progression follows a predictable pattern: physical symptoms (headache, dizziness) improve first, typically within the first week. Cognitive symptoms (concentration, memory) improve next, by days 7-14. Emotional and sleep symptoms resolve last, by weeks 2-3. This temporal pattern guides return to activity—patients can resume physical activity once physical symptoms resolve but may still require cognitive accommodations at work or school until cognitive symptoms clear.
Adolescents (ages 13-18) require longer recovery, typically 3-4 weeks, due to ongoing brain development and increased vulnerability to metabolic disruption. Children under 13 may require even longer, though they also demonstrate remarkable neuroplasticity facilitating ultimate recovery. Pediatric patients require more conservative return-to-learn and return-to-sport protocols with physician clearance.
Complicated concussion with persistent symptoms beyond 4 weeks (post-concussion syndrome) affects 10-15% of patients. Risk factors include female gender (possibly hormonal influences or reporting differences), history of prior concussions (cumulative injury effect), history of migraines (shared pathophysiology), psychiatric history including depression and anxiety, learning disabilities or ADHD (reduced cognitive reserve), and high initial symptom burden (>4 symptoms or total SCAT5 severity score >30). These patients require specialized multidisciplinary treatment combining vestibular rehabilitation, cognitive therapy, exercise training, and often pharmacological intervention. Recovery timelines extend to 3-6 months with appropriate treatment, though some patients develop chronic symptoms persisting beyond six months.
Second impact syndrome, while rare, represents a catastrophic complication where a second concussion before full recovery from the first causes rapid cerebral edema and often death or severe disability. This risk, though documented primarily in adolescents, mandates that patients be fully asymptomatic and cleared by a physician before returning to contact sports or high-risk activities. We use objective assessments (normal SCAT5 scores, normal balance testing, normal cognitive testing, normal exertional tolerance) in addition to subjective symptom resolution before clearance.
Return-to-work protocols vary by occupation: sedentary office work can typically resume at 50% capacity (half-days) once cognitive symptoms are mild, progressing to full-time over 1-2 weeks as tolerated. Jobs requiring driving, operation of heavy machinery, or work at heights require complete symptom resolution and normal reaction time testing given safety implications. Healthcare providers, pilots, and others in safety-sensitive positions may require formal fitness-for-duty evaluations before full clearance.
Return-to-drive is often overlooked but critical: reaction time impairment persists for days to weeks after concussion, increasing motor vehicle accident risk. We recommend no driving in the first 24-48 hours, then daytime low-demand driving only (short trips, familiar routes, light traffic) until symptoms fully resolve. Patients should not drive if taking sedating medications, experiencing significant cognitive slowing, or having visual disturbances.
Long-term outcomes for single concussions with appropriate treatment are generally excellent, with >95% of patients returning to pre-injury function. However, repeated concussions, particularly when occurring before complete recovery from prior injury, carry cumulative risks: chronic traumatic encephalopathy (CTE) is a progressive neurodegenerative disease associated with repetitive head impacts and concussions, presenting with cognitive decline, mood disturbance, and behavioral changes, typically not apparent until years or decades after injury exposure. While originally described in athletes and military personnel with extensive exposure, emerging evidence suggests CTE may develop with fewer impacts than previously thought. This underscores the importance of proper concussion management preventing repeat injury during the vulnerable recovery period.
Prognostic factors predicting favorable recovery include young age (excluding very young children and elderly), no prior concussions, low initial symptom burden, early presentation for treatment (within 24-48 hours), good social support, no psychiatric comorbidities, and ability to rest adequately initially. Conversely, poor prognostic factors include delayed treatment presentation (>1 week), premature return to activity with symptom exacerbation, multiple prior concussions, pre-existing psychiatric conditions, ongoing stressors (litigation, job loss, family conflict), and comorbid cervical spine injury complicating symptom attribution.
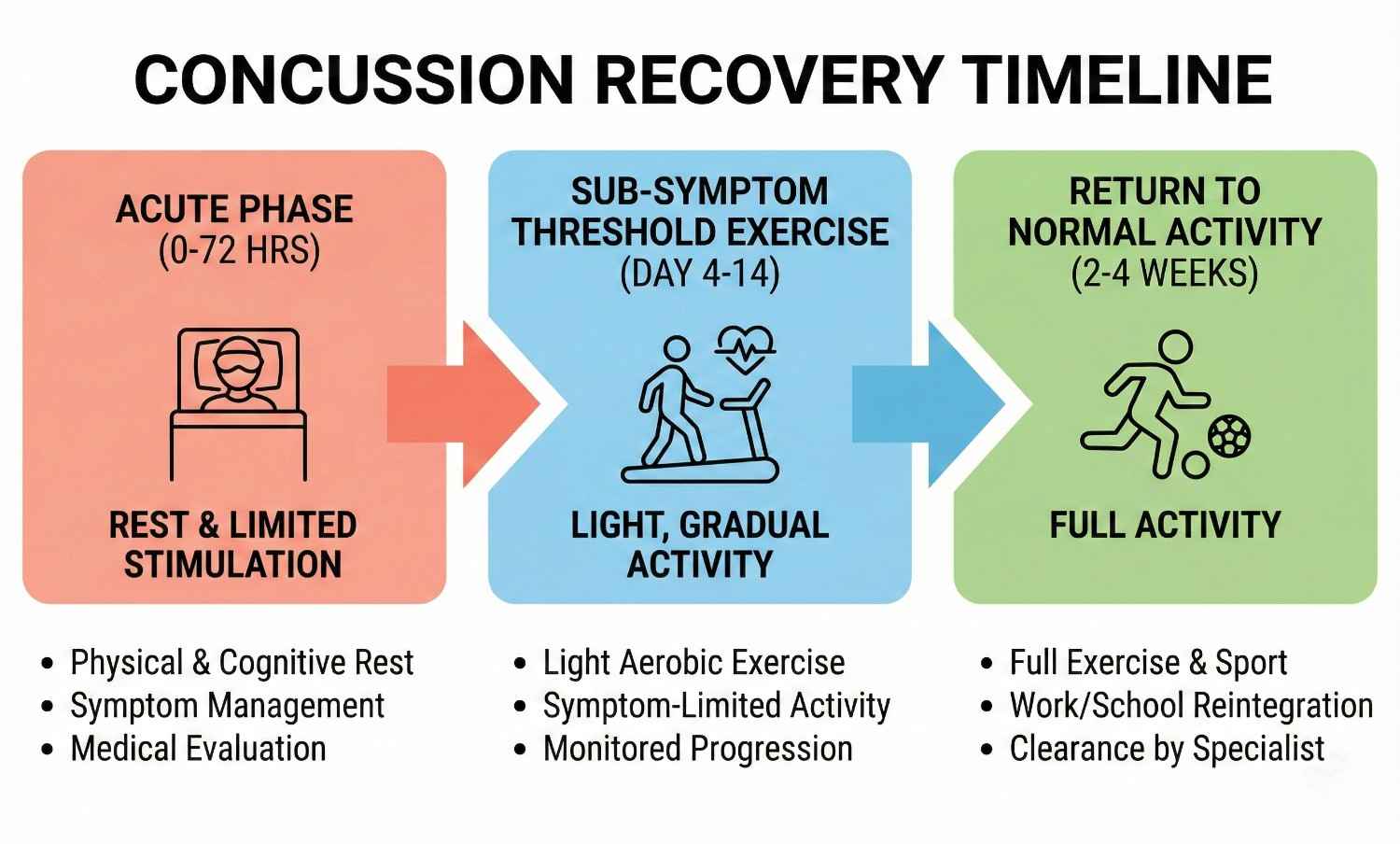
Comprehensive documentation is essential for personal injury claims involving concussion, as the injury often lacks visible external evidence and symptoms may be subjectively reported, creating challenges in proving injury and damages. AccidentDoc Pasadena provides detailed documentation specifically designed to support legal proceedings.
Injury mechanism documentation establishes causation by correlating accident biomechanics with concussion pathophysiology: "Patient sustained concussion on [DATE] when struck from behind at estimated 35 mph while stopped at traffic light on Highway 225. The sudden acceleration-deceleration created coup-contrecoup forces as the brain impacted the frontal skull (coup) then rebounded posteriorly (contrecoup). The documented mechanism is biomechanically consistent with and sufficient to cause mild traumatic brain injury. The patient reports immediate onset of headache, dizziness, and confusion beginning at the accident scene, with symptoms progressing over subsequent hours to include nausea, photophobia, and difficulty concentrating—symptom complex characteristic of acute concussion."
Initial evaluation documentation includes detailed symptom inventory using standardized tools (SCAT5), objective examination findings (balance testing errors, cognitive screening deficits), and functional limitations: "Patient demonstrates 8 errors on BESS testing (normal <5 errors), indicating significant balance impairment. MoCA score 22/30 (<26 abnormal) with deficits in attention and delayed recall. Patient unable to complete work tasks requiring sustained attention, forcing medical leave from employment as [OCCUPATION]."
Serial examinations document symptom evolution and treatment response, critical for establishing persistent injury: "Week 2: Patient reports partial improvement in headache (VAS 8→5) but worsening cognitive symptoms as attempted return to work. Concentration deficit interferes with work performance. SCAT5 symptom severity score 42 (moderate). Week 4: Persistent symptoms despite conservative management, now meeting criteria for post-concussion syndrome. MoCA remains 23/30. Patient unable to work full-time. Week 8: Following vestibular rehabilitation and sub-threshold exercise protocol, symptoms improved to mild severity (SCAT5 score 18). Returned to work 50% capacity with accommodations."
Imaging correlation is documented even when normal: "Head CT obtained [DATE] demonstrates no acute intracranial hemorrhage, mass effect, or skull fracture. The absence of structural abnormality on CT does not exclude concussion, as this injury primarily affects neurometabolic function and axonal integrity not visible on standard imaging. The patient's clinical presentation including documented mechanism, immediate symptom onset, and objective examination abnormalities confirm the diagnosis of mild traumatic brain injury."
Causation statements are clearly articulated: "Within a reasonable degree of medical certainty, this patient's traumatic brain injury including post-concussion syndrome is directly and proximately caused by the motor vehicle collision of [DATE]. The temporal relationship (immediate symptom onset), documented mechanism consistent with concussion, objective findings on standardized testing, and typical symptom progression support causation. The patient had no prior history of head injury, cognitive impairment, or similar symptoms per review of prior medical records obtained from [PRIOR PROVIDERS]. The current condition represents new injury directly attributable to the accident."
Functional limitations are documented with specificity supporting economic damages claims: "Patient's concussion creates measurable functional impairments: (1) Cognitive: Cannot perform work tasks requiring sustained attention, multitasking, or complex problem-solving for more than 20-30 minutes before cognitive fatigue forces breaks. Processing speed reduced to 60% of age-matched norms per ImPACT testing. (2) Physical: Cannot exercise at pre-injury intensity due to exertional headache and dizziness. (3) Social: Cannot tolerate loud restaurants, social gatherings, or bright environments due to sensory sensitivity. (4) Sleep: Requires 10-12 hours sleep nightly vs. pre-injury 7-8 hours, limiting productive hours. These limitations have forced reduced work hours (40→20 hours weekly) with corresponding income loss of approximately $30,000 annually."
Treatment necessity documentation justifies past and future medical expenses: "Patient requires ongoing vestibular rehabilitation (12 sessions completed, 8 additional sessions recommended), neuropsychological cognitive rehabilitation (10 sessions), and possible pharmacological management with headache prophylaxis. Conservative estimated future medical costs: vestibular therapy $1,200, cognitive rehabilitation $1,500, medications $600 annually, annual follow-up evaluations $400, total $3,700 annually for estimated 1-2 years = $5,500-7,400 future medical expenses. Additionally, patient faces 10-20% increased risk of developing chronic headache disorder, early-onset dementia risk elevation with TBI history, and potential need for ongoing cognitive support if persistent deficits remain after one year."
Permanent impairment ratings for concussions reaching maximum medical improvement with residual deficits use AMA Guides: "Patient has reached MMI 12 months post-injury with residual deficits including mild persistent headache (2-3 days weekly), attention/concentration mildly below normative data, and exercise-induced symptom exacerbation limiting high-intensity activity. Using AMA Guides to Evaluation of Permanent Impairment, 6th Edition, Chapter 13 (Central and Peripheral Nervous System), patient has Class 1 impairment (5-8% whole person impairment) based on objective evidence of brain injury with mild functional limitations."
Expert witness testimony explaining concussion pathophysiology, symptom legitimacy despite normal imaging, and long-term prognosis helps juries understand this "invisible injury." Our physicians have extensive experience testifying in depositions and trials regarding traumatic brain injury causation, treatment, and outcomes.
- Detailed mechanism documentation correlating biomechanics with concussion pathophysiology
- Standardized symptom assessments (SCAT5) providing objective quantification
- Serial examinations documenting symptom evolution and treatment response
- Imaging correlation with explanation that normal CT doesn't exclude concussion
- Causation opinions stated within reasonable medical certainty
- Functional limitations documented with economic impact (work capacity loss)
- Treatment necessity justification for past and future medical expenses
- Permanent impairment ratings using AMA Guides at maximum medical improvement
- Expert witness testimony for depositions and trial
- Coordination with life care planners for catastrophic TBI cases
While most concussions are managed on an outpatient basis through our clinic, certain signs and symptoms indicate potentially life-threatening complications including intracranial hemorrhage, cerebral edema, or brain herniation requiring emergency neurosurgical evaluation. Patient and family education about these red flags is critical for preventing catastrophic outcomes.
Decreasing level of consciousness is the most concerning warning sign: if the patient becomes increasingly drowsy, difficult to arouse, or unresponsive after initially being awake and conversant, this suggests evolving intracranial mass effect from hemorrhage or edema. Epidural hematomas classically present with initial loss of consciousness at impact, a "lucid interval" lasting minutes to hours where the patient appears relatively normal, then rapid deterioration as the hematoma enlarges. This pattern requires immediate CT and often emergency craniotomy. We instruct families to check on patients every 2-3 hours during the first 24 hours, ensuring they can be awakened and respond appropriately.
Seizure activity including generalized tonic-clonic seizures (full-body convulsions) or focal seizures (localized shaking, staring spells, altered awareness) indicates cortical irritation from contusion, hemorrhage, or edema. Post-traumatic seizures occur in 5-10% of moderate to severe TBI but are rare in mild concussion. Any seizure warrants emergency evaluation with CT imaging and EEG, as anticonvulsant therapy may be needed and seizures can indicate surgical lesions.
Severe or worsening headache despite medication, particularly if described as "the worst headache of my life," suggests intracranial hemorrhage with rising intracranial pressure. While headache is expected in concussion, progressive worsening or headache of extraordinary severity (patient rating 10/10) mandates CT evaluation. Thunderclap headache (sudden maximal intensity) raises concern for subarachnoid hemorrhage, particularly if associated with nuchal rigidity (stiff neck).
Repeated vomiting (>2 episodes) beyond the initial hours post-injury suggests elevated intracranial pressure. While isolated vomiting once or twice in the immediate aftermath of concussion is common and benign, persistent or recurrent vomiting hours later is concerning. Projectile vomiting (forceful ejection without preceding nausea) is particularly worrisome for elevated ICP.
Focal neurological deficits including unilateral weakness or numbness in arm or leg, facial droop or asymmetry, slurred speech, visual field defects (loss of vision in specific areas), dilated pupil or pupillary asymmetry (anisocoria), and abnormal eye movements all suggest focal brain injury from hemorrhage or contusion affecting specific brain regions. These findings mandate immediate CT and neurosurgical consultation.
Altered mental status beyond initial confusion is concerning: if the patient becomes agitated, combative, or exhibits personality changes dramatically different from baseline, this suggests frontal lobe injury or elevated ICP. Conversely, profound lethargy where the patient shows no interest in surroundings and responds only to painful stimuli indicates severe injury. Persistent confusion beyond the first 2-3 hours, particularly if worsening rather than improving, warrants imaging.
Glasgow Coma Scale (GCS) provides standardized assessment: eyes opening (spontaneous=4, to voice=3, to pain=2, none=1), verbal response (oriented=5, confused=4, inappropriate words=3, incomprehensible sounds=2, none=1), motor response (obeys commands=6, localizes pain=5, withdraws from pain=4, abnormal flexion=3, abnormal extension=2, none=1). GCS <15 indicates need for CT imaging; GCS <13 mandates emergency department evaluation; GCS ≤8 indicates severe TBI requiring ICU admission and often intubation.
Draining fluid from ears or nose (CSF leak indicating skull fracture), clear or blood-tinged drainage particularly if it forms a "halo sign" on gauze (blood center with clear ring), Battle's sign (bruising behind ears appearing 1-2 days post-injury suggesting basilar skull fracture), or raccoon eyes (periorbital ecchymosis suggesting anterior skull base fracture) all indicate skull fracture requiring immediate evaluation. While not all skull fractures require surgery, they increase risk of intracranial injury.
Anticoagulation use including warfarin, direct oral anticoagulants (DOACs like apixaban, rivaroxaban), or antiplatelet agents (Plavix, aspirin) increases hemorrhage risk, warranting lower threshold for CT imaging. These patients should proceed to emergency department for evaluation even with apparently minor head trauma.
When any red flag symptom develops, we direct patients immediately to emergency departments with 24/7 neurosurgical capabilities: Memorial Hermann Southeast Hospital (Houston), Houston Methodist Baytown Hospital, Clear Lake Regional Medical Center, or Ben Taub Hospital (Harris Health System). We provide direct communication with emergency physicians regarding our clinical findings and concerns. After emergency stabilization and neurosurgical management if needed, patients return to our clinic for ongoing post-acute care and rehabilitation coordination.
- Decreasing level of consciousness - increasing drowsiness or difficulty arousing - CALL 911
- Seizure activity - convulsions, shaking, staring spells - EMERGENCY
- Severe or worsening headache unrelieved by medication - possible hemorrhage
- Repeated vomiting (>2 episodes) hours after injury - elevated ICP
- Focal neurological deficits - weakness, numbness, facial droop, vision loss
- Unequal pupils or dilated pupil - suggests mass effect or herniation
- Profound confusion or agitation worsening rather than improving
- Drainage of clear fluid from nose or ears - CSF leak, skull fracture
- Battle's sign or raccoon eyes - skull fracture indicators
- Glasgow Coma Scale <15 - requires immediate CT imaging
- Loss of consciousness >30 seconds - warrants emergency evaluation
- Patients on blood thinners with any head impact - lower threshold for ER
While many accidents causing concussions are unavoidable, evidence-based prevention strategies reduce injury risk and severity. Understanding these measures benefits patients recovering from concussion (preventing repeat injury during vulnerable period) and the general public.
Vehicle safety measures proven to reduce TBI include proper seatbelt use (reducing head impact risk by 60% in frontal crashes), airbag functionality (ensuring airbags aren't deactivated and occupants maintain proper distance from steering wheel), proper headrest positioning (top of headrest level with top of head, 2-3 inches from skull, reducing whiplash and associated concussion), appropriate car seat selection and installation for children (rear-facing until age 2, forward-facing with harness until age 4, booster until properly fitting seatbelt), and avoiding distracted driving (texting, phone use, eating while driving increases collision risk exponentially).
Defensive driving practices reduce accident risk: maintaining safe following distance (3-second rule minimum), scanning environment for potential hazards, avoiding aggressive driving behaviors, adjusting speed for conditions, and expecting unexpected actions from other drivers. In Pasadena's high-traffic areas including Highway 225, I-45, and Fairmont Parkway, heightened vigilance during rush hours, around industrial facilities with large truck traffic, and at major intersections reduces crash probability.
Fall prevention in home and workplace environments includes good lighting (especially stairways and bathrooms), removing tripping hazards (loose rugs, clutter, electrical cords), installing handrails on stairs, using non-slip mats in bathrooms and kitchens, prompt cleanup of spills, proper footwear with good traction, and assistive devices (canes, walkers) for those with balance or mobility impairment. Workplace fall prevention includes proper scaffolding, guardrails, personal fall arrest systems for work at heights, and slip-resistant flooring in areas prone to moisture.
Post-concussion precautions during recovery are critical for preventing second impact syndrome: absolute avoidance of contact sports and high-risk activities (skiing, skateboarding, horseback riding) until symptom-free and cleared by physician, no driving in acute phase (first 24-48 hours minimum) and cautious limited driving until reaction time normalizes, avoiding alcohol which impairs recovery and increases re-injury risk through impaired judgment and balance, using caution in environments with fall risk (crowds, uneven surfaces, dim lighting), and informing family members and coworkers about injury so they can provide monitoring and assistance. Patients with history of concussion should consider avoiding future contact sport participation given cumulative injury risks, particularly if this concussion was their second or third.
Workplace safety in Pasadena's industrial sector includes hard hat use (reduces skull fracture and severe TBI but doesn't fully prevent concussion), situational awareness around heavy equipment and moving machinery, proper lockout/tagout procedures preventing unexpected equipment start-up, confined space safety protocols, and prompt reporting of unsafe conditions. Employers should provide concussion education to workers and supervisors, establish protocols for removing injured workers from duty and ensuring medical evaluation before return to work, and avoid pressuring workers to continue working while symptomatic.
Recognition of subtle concussion symptoms allows early treatment improving outcomes: many accident victims don't realize they've sustained concussion, attributing symptoms to "stress" or "being shaken up." Education about concussion symptoms empowers patients to seek care promptly. We encourage all patients involved in significant accidents with head trauma mechanism—even without direct head impact—to undergo concussion screening, as early diagnosis within 24-48 hours is associated with faster recovery and reduced PCS rates.
Post-recovery, patients should maintain brain health through cognitively stimulating activities, physical exercise supporting cerebrovascular health, Mediterranean diet rich in antioxidants and omega-3 fatty acids, management of vascular risk factors (hypertension, diabetes, hyperlipidemia), adequate sleep (7-9 hours nightly), stress management, and avoidance of smoking and excessive alcohol. These measures support neuroplasticity and cognitive reserve, maximizing long-term brain health after TBI.
Seek Emergency Care Immediately If You Experience:
- Decreasing level of consciousness or difficulty awakening patient
- Seizure activity (convulsions, shaking, staring spells)
- Severe worsening headache unrelieved by medication (worst of life)
- Repeated vomiting (>2 episodes) hours after injury
- Focal weakness, numbness, facial droop, or vision loss
- Unequal or dilated pupils
- Clear fluid draining from nose or ears (CSF leak)
- Profound confusion, agitation, or personality change
- Glasgow Coma Scale <15 (any altered consciousness)
- Loss of consciousness >30 seconds
- Battle's sign (bruising behind ears) or raccoon eyes
- Patients on blood thinners with any head trauma
Call 911 or go to the nearest emergency room immediately

Shoulder and joint injuries represent some of the most complex and debilitating trauma resulting from motor vehicle accidents, workplace incidents, and slip-and-fall events. The shoulder joint, the body's most mobile articulation, sacrifices stability for range of motion, making it particularly vulnerable to dislocation, rotator cuff tears, and labral injuries. Similarly, knee joints endure tremendous forces during accidents, suffering ACL tears, meniscal damage, and ligament sprains. AccidentDoc Pasadena's board-certified physicians specialize in comprehensive evaluation and treatment of all joint injuries, from acute trauma through complete functional restoration, serving Pasadena's industrial workforce with expertise in construction injuries, refinery accidents, and motor vehicle trauma.
The shoulder complex represents the most intricate joint system in the human body, comprising four distinct articulations: the glenohumeral joint (ball-and-socket), acromioclavicular joint (AC joint connecting clavicle to acromion), sternoclavicular joint (clavicle to sternum), and scapulothoracic articulation (scapula gliding on rib cage). The glenohumeral joint achieves remarkable mobility—180° of forward flexion, 180° of abduction, and 90° of external rotation—through a shallow glenoid socket articulating with the large humeral head. This inherent instability necessitates robust soft tissue support.
The rotator cuff consists of four muscles with tendons converging on the humeral head: supraspinatus (abduction initiation, most commonly torn), infraspinatus (external rotation), teres minor (external rotation and adduction), and subscapularis (internal rotation). These muscles function synergistically to compress the humeral head into the glenoid socket (concavity-compression mechanism) and counteract deltoid's superior pull during arm elevation. The supraspinatus tendon passes through the subacromial space, a narrow corridor between the humeral head and acromion, predisposing it to impingement and degenerative tearing.
The glenoid labrum is a fibrocartilaginous rim deepening the glenoid socket by approximately 50%, enhancing stability. Superior labrum anterior-posterior (SLAP) tears occur when sudden traction or compression forces disrupt this structure, common in dashboard bracing during frontal collisions or catching oneself during falls. The long head of biceps tendon originates at the superior labrum, explaining why SLAP tears often present with anterior shoulder pain and bicipital groove tenderness.
Shoulder ligaments provide static stability: the superior, middle, and inferior glenohumeral ligaments resist anterior and inferior translation at various arm positions. The coracohumeral ligament resists inferior subluxation. High-energy trauma can tear these ligaments, causing instability patterns requiring surgical reconstruction.
The knee joint, the body's largest articulation, comprises the tibiofemoral joint (femoral condyles on tibial plateau) and patellofemoral joint (kneecap tracking on femur). Cruciate ligaments provide anteroposterior stability: the anterior cruciate ligament (ACL) prevents anterior tibial translation and internal rotation, most commonly torn during dashboard impacts, twisting injuries, or hyperextension. The posterior cruciate ligament (PCL) prevents posterior tibial translation, classically injured in dashboard knee when the tibia is driven posteriorly. Collateral ligaments resist varus-valgus stress: medial collateral ligament (MCL) prevents valgus (knee bowing inward), lateral collateral ligament (LCL) prevents varus (knee bowing outward).
Menisci are C-shaped fibrocartilage structures (medial and lateral) serving as shock absorbers, load distributors, and stability enhancers. They increase contact area between femoral condyles and tibial plateau by 50-70%, reducing peak contact pressures. Meniscal tears result from rotational forces with the knee flexed and weight-bearing, or from direct compression in accidents. The medial meniscus, firmly attached to the joint capsule and MCL, is less mobile and more frequently torn than the lateral meniscus.
Understanding this complex anatomy guides diagnostic and treatment approaches. Shoulder injuries often involve multiple structures simultaneously—rotator cuff tears commonly coexist with labral pathology and AC joint sprains. Similarly, knee injuries frequently combine ligament and meniscal damage, requiring comprehensive evaluation rather than single-structure focus.
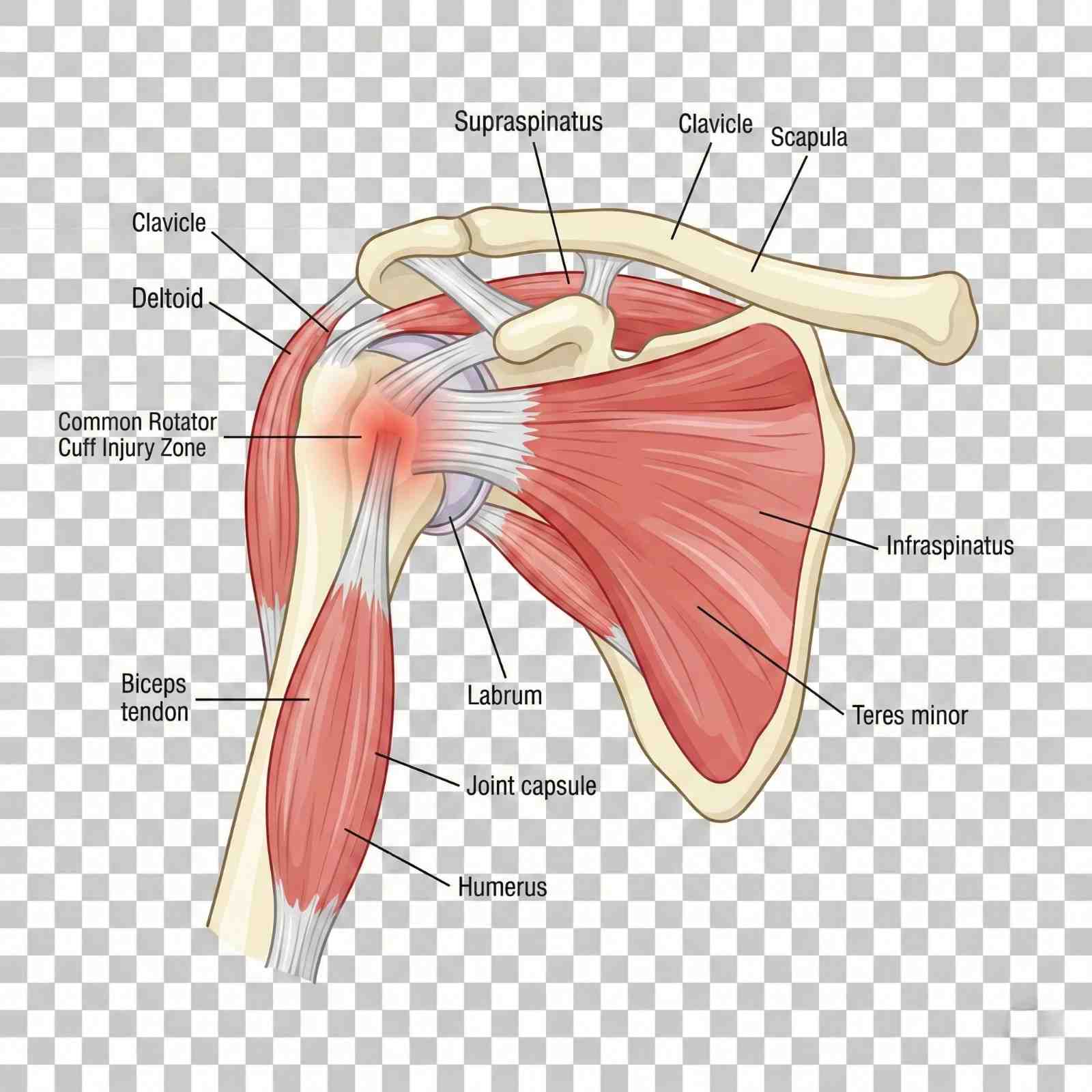
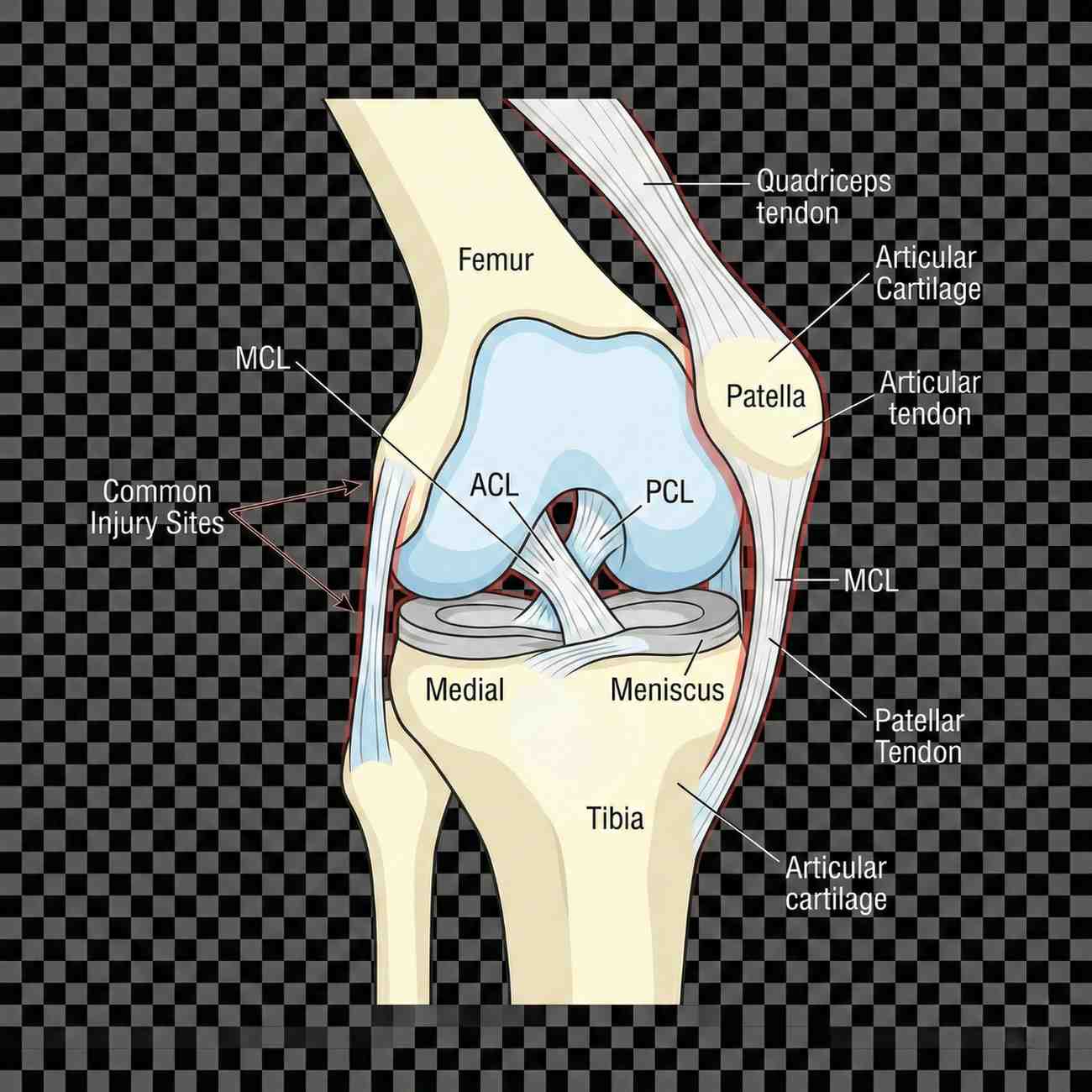
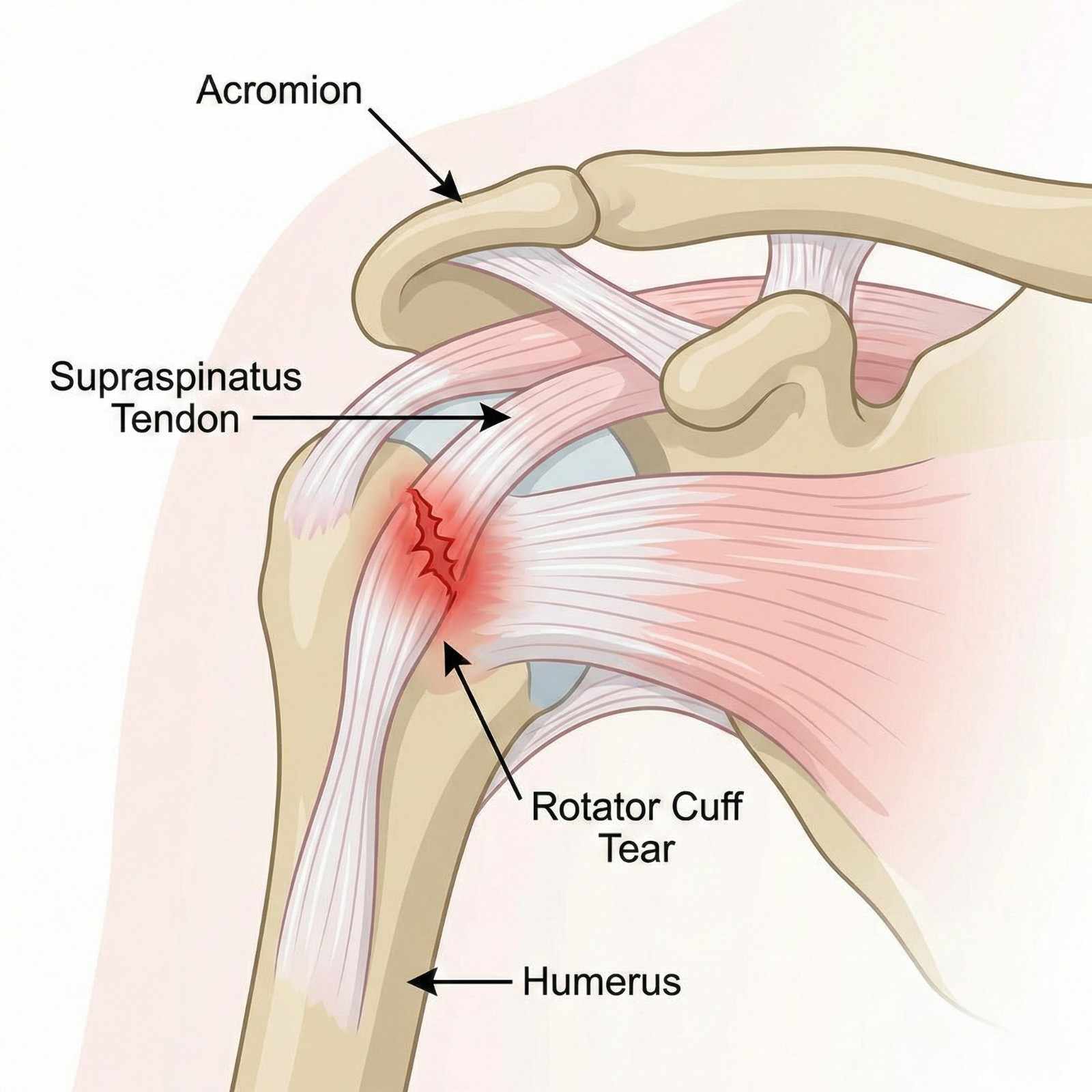
Joint injuries present with variable symptom patterns depending on structures injured, injury mechanism, and timing since trauma. Recognizing these presentations guides differential diagnosis and treatment planning.
Shoulder injuries typically manifest with anterior, lateral, or posterior pain depending on structures involved. Rotator cuff tears produce lateral shoulder pain radiating into the deltoid region, worse with overhead activities, reaching behind the back, or sleeping on the affected side. Night pain is characteristic—patients often report inability to sleep on the injured shoulder. Weakness with arm elevation, particularly abduction between 60-120° (painful arc), suggests supraspinatus involvement. Complete tears produce profound weakness—patients cannot initiate abduction or maintain arm elevation against gravity (positive drop arm test).
Shoulder dislocations cause severe acute pain, visible deformity with the arm held in slight abduction and external rotation, and reluctance to move the shoulder. Anterior dislocations (95% of cases) result from arm abduction with external rotation and extension, classic during motor vehicle accidents when bracing against dashboard or during falls on outstretched hand. The humeral head displaces anteriorly, creating a "squared-off" shoulder appearance compared to the opposite side. Associated axillary nerve injury occurs in 10-40% of cases, producing deltoid weakness and numbness over the lateral upper arm—this must be documented before and after reduction attempts.
AC joint separations produce point tenderness and often visible deformity at the top of the shoulder where the clavicle meets the acromion. Grade 1 sprains cause tenderness without visible deformity. Grade 2 injuries show mild elevation of the distal clavicle compared to the opposite shoulder. Grade 3-6 separations demonstrate obvious clavicle elevation ("piano key sign"—pressing down on the prominent clavicle causes it to spring back up). Pain worsens with cross-body adduction (bringing arm across chest) and overhead activities.
Labral tears, particularly SLAP lesions, cause deep anterior shoulder pain, often described as catching or clicking with overhead motions. Patients may report feeling that the shoulder "gives way" or "goes dead" during activities. Pain radiating into the biceps region is common. SLAP tears are notoriously difficult to diagnose clinically and often require MRI arthrog raphy for confirmation.
Knee injuries present distinct patterns. ACL tears typically occur during non-contact twisting injuries or dashboard impacts. Patients often report hearing or feeling a "pop" at injury, followed by immediate swelling (hemarthrosis developing within hours rather than days suggests ACL tear). The knee feels unstable or "gives way" during cutting or pivoting movements. Chronic ACL deficiency causes recurrent instability episodes and risk of secondary meniscal and cartilage damage.
MCL sprains cause medial knee pain and tenderness along the ligament course. Grade 1 sprains produce pain with valgus stress but maintain stability. Grade 2 tears show increased laxity with valgus stress but maintain a firm endpoint. Grade 3 complete tears demonstrate gross instability with no firm endpoint. Isolated MCL injuries have good healing potential with conservative treatment, but combined ACL-MCL injuries may require surgical reconstruction.
Meniscal tears cause mechanical symptoms: catching, locking (inability to fully extend the knee), or giving way. Pain localizes to the medial or lateral joint line depending on which meniscus is torn. A "locked" knee unable to extend beyond 15-20° flexion suggests displaced meniscal fragment blocking full extension—this requires urgent orthopedic evaluation. Swelling typically develops gradually over 12-24 hours (synovitis from mechanical irritation) rather than immediately (distinguishing from ligament injuries with hemarthrosis).
Patellofemoral injuries range from patellar dislocation to chondral fractures. Patellar dislocations cause immediate lateral knee pain, often with visible deformity (patella displaced laterally). Many dislocations spontaneously reduce before medical evaluation. Patients report feeling the kneecap "slide out of place." Significant swelling and tenderness along the medial retinaculum (torn during lateral dislocation) are present. Recurrent patellar instability affects 15-50% of patients after initial dislocation.
Bursitis commonly develops after direct trauma. Prepatellar bursitis (housemaid's knee) from kneeling impacts causes anterior knee swelling directly over the kneecap. Olecranon bursitis from elbow impacts produces posterior elbow swelling. Trochanteric bursitis causes lateral hip pain worse with lying on that side. These inflammatory conditions require distinction from septic bursitis (infected bursa requiring aspiration and antibiotics).
Red flag symptoms requiring urgent evaluation include diminished pulses distal to injury (vascular compromise), progressive neurological deficits (nerve injury), fever with joint swelling (septic arthritis), severe pain disproportionate to exam findings with tense swelling (compartment syndrome), and open joint injuries with visible bone or articular cartilage (infection risk).
Accurate diagnosis of joint injuries requires systematic physical examination combined with strategic imaging studies. Clinical examination provides immediate diagnostic information, while imaging confirms clinical suspicions and identifies associated injuries not apparent on examination.
Shoulder examination begins with inspection: observe for deformity, atrophy, or asymmetry compared to the opposite side. Palpate bony landmarks—acromioclavicular joint, coracoid process, bicipital groove, and greater tuberosity—identifying point tenderness. Range of motion testing quantifies functional limitations: forward flexion (normal 180°), abduction (normal 180°), external rotation with arm at side (normal 60-90°), and internal rotation assessed by hand-behind-back reach (normal to mid-scapula level).
Specific provocative tests isolate injured structures. The Jobe test (empty can test) evaluates supraspinatus: patient abducts arms to 90° in scapular plane (30° forward of coronal plane), internally rotates shoulders (thumbs pointing down), and resists downward pressure—pain or weakness indicates supraspinatus pathology. External rotation strength testing targets infraspinatus and teres minor. The lift-off test examines subscapularis: patient places hand behind back and attempts to lift hand away from back against resistance.
Impingement tests reproduce pain from subacromial pathology. Neer's impingement sign: examiner forward flexes patient's arm to maximum elevation while preventing scapular rotation—pain suggests impingement. Hawkins-Kennedy test: arm flexed to 90° then internally rotated—pain indicates impingement.
Instability testing assesses ligamentous integrity. Apprehension test: patient supine, arm abducted 90° and externally rotated—apprehension or pain suggests anterior instability. Relocation test: posterior pressure on humeral head while in apprehension position relieves pain, confirming anterior instability. Sulcus sign: downward traction on the arm creates visible sulcus below acromion, indicating inferior instability.
Labral tests detect tears. O'Brien's test (active compression test): arm forward flexed 90°, adducted 10-15°, and internally rotated (thumb down); patient resists downward force—pain suggests labral pathology, particularly SLAP tears.
Knee examination evaluates ligamentous stability. Lachman test is most sensitive for ACL tears: knee flexed 20-30°, examiner stabilizes femur and applies anterior force to proximal tibia—excessive anterior translation with soft or absent endpoint indicates ACL tear. Anterior drawer test (knee flexed 90°) is less sensitive but more specific. Pivot shift test mimics giving-way sensation: knee extended then flexed while applying valgus and internal rotation forces—sudden reduction of subluxed tibia confirms ACL deficiency.
Valgus stress testing evaluates MCL: knee at 0° (tests MCL and capsule) and 30° flexion (isolates MCL)—increased laxity indicates injury severity. Varus stress tests LCL similarly. Posterior drawer test assesses PCL integrity.
Meniscal tests include McMurray's test: knee fully flexed, tibia internally rotated and knee extended while applying valgus stress (medial meniscus), or externally rotated with varus stress (lateral meniscus)—pain or clicking suggests meniscal tear. Thessaly test: patient stands on one leg, knee flexed 20°, and internally/externally rotates body—pain suggests meniscal pathology.
Imaging studies confirm clinical diagnoses. X-rays are first-line for all joint injuries: standard shoulder series includes AP, lateral (Y-view or scapular lateral), and axillary views identifying fractures, dislocations, and degenerative changes. AC joint views with and without weights quantify AC separation severity. Knee X-rays include AP, lateral, and sunrise (patellofemoral) views. Standing films assess alignment and joint space narrowing. Stress views may be obtained for ligament injuries.
MRI is gold standard for soft tissue injuries: rotator cuff tears (90% sensitivity/specificity), labral tears, ligament injuries, meniscal tears, and cartilage defects. MRI arthrography (contrast injected into joint) improves labral tear detection. Standard protocol MRI without contrast typically suffices for most injuries.
Ultrasound performed by experienced operators can diagnose rotator cuff tears with accuracy comparable to MRI. Advantages include lower cost, real-time dynamic assessment, and lack of contraindications. Limitations include operator dependence and inferior visualization of labrum and glenohumeral ligaments.
CT scans excel for bony detail: fracture characterization, alignment assessment, and surgical planning. CT arthrography can detect labral tears when MRI is contraindicated.
At AccidentDoc Pasadena, we provide in-office X-rays for immediate fracture assessment and arrange expedited MRI within 72 hours when soft tissue injuries require confirmation. This rapid diagnostic approach ensures treatment begins promptly, crucial for optimal outcomes and medico-legal documentation.
Joint injury treatment spans conservative management for mild-moderate injuries to surgical reconstruction for severe trauma, guided by injury severity, functional demands, and patient goals. Most joint injuries initially receive conservative treatment, progressing to surgery only when non-operative approaches fail or injury severity mandates surgical intervention.
Acute phase management (first 2 weeks) focuses on controlling pain and inflammation while protecting injured structures. RICE protocol (Rest, Ice, Compression, Elevation) remains foundational. Ice application 20 minutes every 2-3 hours during the first 48-72 hours reduces swelling and pain. Compression with elastic wraps or braces controls edema. Elevation above heart level utilizes gravity for fluid drainage.
Immobilization duration requires careful balance. Shoulder slings prevent painful motion and protect healing tissues but should be limited to 1-2 weeks maximum for most injuries (excluding fractures and surgical repairs) to prevent stiffness. Range of motion exercises begin early, even during immobilization periods, to maintain mobility. Complete immobilization causes rapid loss of motion—shoulder stiffness develops within days, particularly in patients over 40 years old.
Knee bracing provides stability for ligament injuries. Hinged knee braces allow controlled range of motion while restricting potentially harmful varus-valgus stress. ACL braces help prevent giving-way episodes in ACL-deficient knees for patients opting for non-operative management or awaiting surgery. Patellar stabilizing braces prevent lateral subluxation in patellofemoral instability.
Pharmacological management utilizes NSAIDs for anti-inflammatory and analgesic effects. Ibuprofen 400-600mg three times daily or naproxen 500mg twice daily provides adequate relief for most patients. Patients with cardiovascular risk factors, kidney disease, or gastrointestinal ulcer history may require alternatives. Acetaminophen 1000mg three-four times daily provides analgesia without anti-inflammatory effects. Topical NSAIDs (diclofenac gel) offer localized pain relief with minimal systemic absorption, useful for patients unable to tolerate oral NSAIDs. Short courses of oral corticosteroids (methylprednisolone dose pack) may be prescribed for severe inflammation.
Corticosteroid injections provide targeted anti-inflammatory therapy. Subacromial injections for rotator cuff tendinopathy combine corticosteroid with local anesthetic, providing both immediate pain relief and anti-inflammatory effects lasting weeks to months. AC joint injections treat AC joint arthritis and sprains. Knee injections address inflammatory arthritis, bursitis, or as temporizing treatment for degenerative changes. While effective for pain relief, corticosteroid injections do not heal torn tendons or ligaments and should be used judiciously—repeated injections can cause tendon weakening or cartilage damage.
Hyaluronic acid (viscosupplementation) injections for knee osteoarthritis provide lubrication and potential disease-modifying effects, though evidence remains controversial. A series of 3-5 injections given weekly may provide months of symptom relief.
Platelet-rich plasma (PRP) injections represent regenerative medicine approach: patient's blood is centrifuged to concentrate platelets containing growth factors, then injected into injured tissues. Evidence supports PRP for partial rotator cuff tears and knee osteoarthritis, though insurance coverage remains limited.
Physical therapy is cornerstone of conservative management. Therapists guide progressive strengthening, restore range of motion, improve proprioception, and correct biomechanical deficiencies contributing to injury. Shoulder therapy focuses on rotator cuff strengthening, scapular stabilization, and restoring normal shoulder mechanics. Knee therapy emphasizes quadriceps strengthening (particularly vastus medialis obliquus for patellar stability), hamstring strengthening, proprioceptive training, and return-to-sport drills for athletes.
Surgical indications for shoulder injuries include complete rotator cuff tears in active patients (surgery within 6 months optimizes outcomes before muscle atrophy and tendon retraction), recurrent shoulder dislocations (particularly in young patients with >90% recurrence risk), displaced fractures, and labral tears causing mechanical symptoms or instability unresponsive to conservative treatment. Arthroscopic techniques allow rotator cuff repair, labral repair, and AC joint reconstruction through small incisions with faster recovery than open procedures.
Knee surgical indications include ACL tears in active individuals or those with instability affecting daily activities (reconstruction typically using patellar tendon or hamstring autograft), displaced meniscal tears causing locking or persistent pain (arthroscopic partial meniscectomy or meniscal repair), and multi-ligament knee injuries. Isolated meniscal tears in patients over 40 with degenerative tears often respond to conservative management, avoiding surgery.
Recovery timelines vary by injury severity and treatment approach. Minor sprains and strains resolve in 4-8 weeks with conservative treatment. Moderate injuries requiring aggressive rehabilitation may need 3-4 months for return to full activities. Surgical reconstructions typically require 4-6 months for return to sports, with full strength restoration taking 9-12 months. At AccidentDoc Pasadena, we coordinate with orthopedic surgeons when surgical evaluation is indicated, ensuring seamless care transitions while maintaining continuity for non-operative management.
Joint injury recovery follows predictable phases, though individual timelines vary based on injury severity, age, comorbidities, and treatment adherence. Understanding expected progressions helps patients maintain realistic expectations and clinicians identify concerning deviations requiring intervention.
Acute inflammatory phase (days 0-7) involves hemostasis and initial inflammatory response. Tissues are fragile and susceptible to re-injury. Pain and swelling peak within 24-72 hours. Treatment focuses on protection (immobilization or bracing), pain control, and edema management. Gentle range of motion exercises begin immediately for most injuries to prevent stiffness, performed within pain-free ranges. Strengthening is contraindicated during this phase.
Proliferative phase (weeks 1-6) encompasses tissue repair. Fibroblasts produce collagen forming scar tissue bridging injured structures. This new tissue is weak and disorganized. Treatment emphasizes gradual mobilization, progressive range of motion exercises, and introduction of light strengthening. Joint mobilization techniques improve mechanics. Modalities including ultrasound and electrical stimulation may accelerate healing. Pain should decrease progressively—persistent or worsening pain suggests inadequate healing or complications.
Remodeling phase (weeks 6-12+) involves collagen reorganization along stress lines, increasing tensile strength. Treatment focuses on progressive strengthening, functional training, and return-to-activity protocols. For surgical reconstructions, tissue healing requires longer—tendon-to-bone healing (rotator cuff repair, ACL reconstruction) takes 3-4 months for secure biologic incorporation. Protected loading during this period prevents graft failure.
Shoulder rehabilitation protocols vary by injury. Rotator cuff tendinopathy without full-thickness tear: weeks 1-2 focus on pain control and gentle range of motion. Weeks 3-6 introduce scapular stabilization and rotator cuff strengthening using resistance bands. Weeks 7-12 progress to sport-specific training. Full return to overhead activities typically occurs at 3-4 months.
Post-operative rotator cuff repair requires more conservative progression due to tendon-to-bone healing requirements. Phase 1 (weeks 0-6): passive range of motion only (therapist moves arm, patient relaxed) with sling immobilization between exercises. Phase 2 (weeks 6-12): active-assisted then active range of motion begins. Phase 3 (weeks 12-20): progressive strengthening begins once healing confirmed on imaging. Phase 4 (months 5-9): advanced strengthening and return to unrestricted activities. Overhead athletes may require 9-12 months for full return to sport.
Shoulder dislocation rehabilitation: first-time dislocations in young patients have 90% recurrence risk without surgery, so early surgical stabilization is often recommended. Post-stabilization surgery protocol: weeks 0-6 immobilization in sling, pendulum exercises only. Weeks 6-12: progressive range of motion restoration. Months 3-4: strengthening begins. Months 5-6: return to non-contact sports. Months 6-9: return to contact sports with protective bracing.
ACL reconstruction rehabilitation: immediate post-operative phase (weeks 0-2) focuses on edema control, restoring full extension (crucial to prevent arthrofibrosis), and initiating quadriceps activation. Protected weight-bearing with crutches advances to full weight-bearing as tolerated. Weeks 2-6: restore full flexion, progress closed-chain strengthening, maintain extension. Months 2-3: progressive strengthening, proprioceptive training, initiate straight-line jogging. Months 3-4: advance running program, sport-specific drills. Months 5-6: functional testing (hop tests, strength testing) guides return-to-sport decisions—return when achieving >90% limb symmetry on objective testing. Full return typically at 6-9 months for recreational athletes, 9-12 months for competitive athletes.
Meniscal tear rehabilitation depends on treatment. Meniscectomy (partial removal) allows rapid progression: immediate weight-bearing, full range of motion as tolerated, return to sports at 4-8 weeks once strength restored. Meniscal repair requires slower progression to protect healing: 6 weeks partial weight-bearing, restricted motion, then gradual advancement. Full return to sports at 4-6 months post-repair.
Complications affecting recovery include arthrofibrosis (abnormal scar causing stiffness), particularly after shoulder surgery or prolonged immobilization—aggressive physical therapy and occasionally surgical lysis of adhesions may be required. Complex regional pain syndrome (CRPS, formerly reflex sympathetic dystrophy) causes disproportionate pain, allodynia, vasomotor changes, and progressive dysfunction—requires specialized pain management. Re-injury from premature return to activity sets recovery back weeks to months.
Return-to-work considerations depend on occupational demands. Sedentary desk work may resume in 1-2 weeks for most injuries. Light-duty work with lifting restrictions up to 10-20 lbs may be possible at 4-6 weeks. Heavy manual labor, construction, or warehouse work typically requires 8-12 weeks minimum, longer for surgical repairs. Work restrictions must balance functional recovery with financial necessity—we work closely with employers to facilitate modified duty when possible, preventing prolonged work absence.
Return-to-sport decisions require objective criteria, not arbitrary timelines. Athletes must demonstrate full pain-free range of motion, >85-90% strength compared to opposite side, sport-specific functional capacity, and psychological readiness. Functional tests including hop tests (single-leg hop, crossover hop, triple hop for distance) and cutting maneuvers assess readiness. Premature return risks re-injury with potentially worse outcomes than original injury.
Comprehensive documentation is essential for joint injury claims, as insurance companies frequently dispute causation, necessity of treatment, and permanency of impairments. AccidentDoc Pasadena provides detailed medical-legal documentation specifically designed to support litigation and workers' compensation proceedings.
Injury mechanism documentation establishes causation through biomechanical correlation: "Patient sustained right shoulder injury on [DATE] during motor vehicle collision when struck from left side by vehicle traveling estimated 40 mph. The lateral impact created sudden valgus and external rotation force on the braced right arm as patient gripped steering wheel, producing mechanism consistent with rotator cuff tear and labral injury. This specific injury mechanism is biomechanically sufficient to cause documented pathology." Detailed mechanism description correlates accident forces with tissue damage patterns, rebutting insurance arguments that injuries pre-existed or arose from degenerative processes.
Initial evaluation documentation establishes temporal relationship and baseline severity: "Patient presented [X days] post-accident reporting immediate onset right shoulder pain and inability to lift arm above shoulder level. Prior to accident, patient worked as [OCCUPATION] performing [SPECIFIC DUTIES] without shoulder limitations—no prior shoulder injuries or treatments per review of prior medical records obtained from [PROVIDERS]. Physical examination reveals severe limitation of active range of motion—forward flexion 80° (normal 180°), abduction 70° (normal 180°), external rotation 20° (normal 90°). Significant weakness with resisted abduction (2/5 strength). Positive impingement signs, positive drop arm test. These findings are acute, causally related to documented trauma, and represent new injury not present pre-accident."
Diagnostic imaging correlation provides objective evidence: "MRI performed [DATE] demonstrates full-thickness tear of supraspinatus tendon measuring 2.1 cm in anteroposterior dimension with 1.5 cm retraction of tendon edge, indicating complete rupture. Associated findings include moderate muscle atrophy and fatty infiltration (Goutallier grade 2) indicating chronicity of tear. However, clinical correlation with recent trauma and acute symptom onset indicates acute-on-chronic pathology—pre-existing degenerative tendon suffered complete rupture during accident. The acute traumatic component is the predominant cause of current disability and treatment necessity." This language acknowledges imaging findings of degeneration while establishing acute trauma as causative factor, addressing insurance company arguments about pre-existing conditions.
Treatment documentation justifies medical necessity: "Conservative management initiated including subacromial corticosteroid injection ([DATE]), physical therapy (20 sessions from [DATE] to [DATE]), and oral NSAIDs. Despite 4 months of aggressive non-operative treatment, patient demonstrates persistent pain (VAS 7/10), functional limitation (unable to perform overhead work duties), and objective evidence of complete rotator cuff tear. Surgical consultation obtained [DATE]—orthopedic surgeon recommends arthroscopic rotator cuff repair. Surgery is medically necessary to restore function and prevent progressive rotator cuff arthropathy. Without repair, patient faces permanent disability affecting occupational and personal activities."
Surgical documentation details procedures performed: "Patient underwent arthroscopic rotator cuff repair on [DATE] performed by Dr. [SURGEON NAME]. Operative report confirms full-thickness tear of supraspinatus and partial-thickness tear of infraspinatus. Surgical findings consistent with traumatic etiology—tear margins showed acute appearance without significant degenerative fraying. Repair performed using [TECHNIQUE]. Post-operative rehabilitation has progressed through [CURRENT PHASE]. Expected recovery timeline is 6-9 months for return to full duty work."
Functional limitations quantify disability: "Current functional deficits include inability to lift objects above shoulder level (maximum safe lift 10 lbs at waist level), inability to reach overhead, inability to sleep on injured side, and inability to perform [SPECIFIC JOB DUTIES]. These limitations directly result from accident-caused shoulder injury and persist despite treatment. Patient requires ongoing restrictions: no lifting >20 lbs, no overhead reaching, no repetitive use of injured arm until surgical repair healed—estimated [DATE]."
Causation opinions stated with medical certainty: "Within a reasonable degree of medical certainty, this patient's right shoulder rotator cuff tear, labral tear, and associated functional impairments are directly and proximately caused by the motor vehicle collision of [DATE]. The temporal relationship (injury onset coinciding with accident), documented mechanism consistent with injury pattern, absence of prior shoulder complaints or treatment, and objective confirmation on MRI all support causation. Alternative explanations including spontaneous degenerative tear are inconsistent with the clinical presentation."
Permanent impairment ratings when maximum medical improvement (MMI) reached: "Patient reached MMI on [DATE], 12 months post-surgery. Residual impairments include loss of range of motion (forward flexion 160° vs normal 180°, abduction 170° vs 180°), loss of strength (4+/5 vs 5/5 pre-injury), persistent pain with strenuous activities, and permanent work restrictions (no repetitive overhead reaching, maximum lift 30 lbs). Using AMA Guides to Evaluation of Permanent Impairment, 6th Edition, upper extremity impairment is [X]% which converts to [Y]% whole person impairment. This permanent impairment directly resulted from accident and affects patient's earning capacity and quality of life."
Future medical costs are documented: "Patient will require ongoing monitoring with orthopedic follow-up annually to assess for progressive degenerative changes in repaired shoulder. Future treatment needs may include periodic corticosteroid injections (estimated $500 each, up to 2 per year), revision surgery if repair fails (15-20% risk, cost $30,000-50,000), and possible shoulder replacement in 15-20 years if post-traumatic arthritis develops (cost $40,000-60,000). Conservative estimated lifetime future medical costs: $25,000-75,000."
Expert witness testimony explaining biomechanics, causation, and treatment rationale helps juries understand complex joint injuries. Our physicians have testified in Harris County courts regarding shoulder and knee injuries, rotator cuff pathology, surgical necessity, and permanency ratings.
Seek Emergency Care Immediately If You Experience:
- Diminished or absent pulses distal to injury (vascular compromise)
- Knee dislocation - 30-40% risk of popliteal artery injury requiring emergency vascular evaluation
- Severe pain out of proportion with tense swelling (compartment syndrome)
- Inability to perform straight leg raise with palpable gap (extensor mechanism rupture)
- Complete motor or sensory loss in nerve distribution (possible nerve transection)
- Locked knee unable to extend beyond 15-20° (displaced meniscal tear)
- Open joint injury or penetrating wound near joint (infection risk)
- Expanding hematoma or uncontrolled bleeding
- Fever with severe joint swelling, warmth, inability to move (septic arthritis)
- Progressive neurological deterioration despite treatment
- Fracture-dislocation visible on imaging (requires urgent reduction)
Call 911 or go to the nearest emergency room immediately

Occupational injuries affect millions of American workers annually, with construction, warehouse, and industrial workers in the Pasadena-Harris County area facing particularly high risks due to the concentration of refineries, petrochemical plants, and manufacturing facilities along the Houston Ship Channel. Work-related musculoskeletal disorders (WMSDs) account for over 30% of all workers' compensation claims in Texas, encompassing acute traumatic injuries from workplace accidents and cumulative trauma disorders from repetitive motion, forceful exertion, and awkward postures. AccidentDoc Pasadena specializes in occupational medicine, providing comprehensive evaluation, treatment, and documentation for both workers' compensation claims and personal injury cases when claims are denied. Our board-certified physicians understand the unique medical-legal requirements of occupational injuries, offering same-day appointments to ensure injured workers receive prompt care while protecting their legal rights.
Occupational injuries encompass two distinct but often overlapping categories: acute traumatic injuries resulting from specific workplace incidents, and cumulative trauma disorders (CTDs) developing gradually from repetitive exposures to biomechanical stressors. Understanding this distinction is critical for proper diagnosis, treatment, and workers' compensation claim processing.
Acute traumatic injuries involve sudden, identifiable events causing immediate tissue damage. In construction settings, these include falls from scaffolding or ladders causing fractures and spinal injuries, being struck by falling objects or equipment resulting in contusions and orthopedic trauma, caught-between accidents involving machinery causing crush injuries, and overexertion injuries from lifting or moving heavy materials causing acute lumbar strain or disc herniation. In warehouse environments, forklift accidents, falling merchandise, and acute lifting injuries predominate. Refinery and petrochemical workers face unique hazards including chemical exposures, confined space accidents, falls from elevated structures, and high-energy trauma from equipment failures. These acute injuries produce immediate symptoms, clear temporal relationships to workplace incidents, and are generally straightforward to establish as work-related under Texas workers' compensation law.
Cumulative trauma disorders develop insidiously from repeated microtrauma exceeding tissue repair capacity. Each individual exposure may be subcritical for injury, but accumulated over weeks, months, or years, the cumulative effect produces symptomatic tissue damage. Common CTDs include carpal tunnel syndrome from repetitive hand motions with wrist flexion (assembly work, computer use, tool operation), lateral epicondylitis (tennis elbow) from repetitive forearm pronation-supination with gripping (tool use, material handling), medial epicondylitis (golfer's elbow) from repetitive wrist flexion and forearm pronation (lifting, hammering), rotator cuff tendinopathy from repetitive overhead reaching (electrical work, painting, construction), De Quervain's tenosynovitis affecting thumb tendons from repetitive grasping with ulnar deviation (packaging, assembly), and chronic lumbar strain from repetitive bending, lifting, and twisting (warehouse work, construction, healthcare).
Ergonomic risk factors quantified by occupational medicine research include: Force - the amount of muscular effort required (lifting >25 lbs repeatedly increases injury risk exponentially); Repetition - cycles per minute performing similar motions (>10 repetitions per minute of the same motion significantly elevates risk); Posture - deviation from neutral anatomical positions (sustained wrist flexion >30°, shoulder abduction >60°, lumbar flexion while lifting increases tissue stress); Duration - time spent in risk positions without rest (continuous exposure >2 hours without breaks); and Vibration - exposure to hand-arm or whole-body vibration (power tool use, heavy equipment operation).
The National Institute for Occupational Safety and Health (NIOSH) has established exposure limits for various occupational activities. The NIOSH lifting equation calculates recommended weight limits based on horizontal distance, vertical distance, asymmetry, coupling, and frequency—loads exceeding calculated limits place workers at high risk for lumbar injury. The ACGIH (American Conference of Governmental Industrial Hygienists) publishes threshold limit values (TLVs) for hand activity levels correlating repetition and force with distal upper extremity disorder risk.
In Pasadena's industrial corridor, workers face compound risk factors: 12-hour shifts reduce recovery time between exposures, physically demanding work in petrochemical facilities and construction sites involves high force requirements, and production pressures may limit adequate rest breaks. Our occupational medicine approach identifies specific workplace risk factors, correlates them with clinical findings, and provides detailed causation analysis supporting workers' compensation claims or personal injury litigation when claims are wrongfully denied.
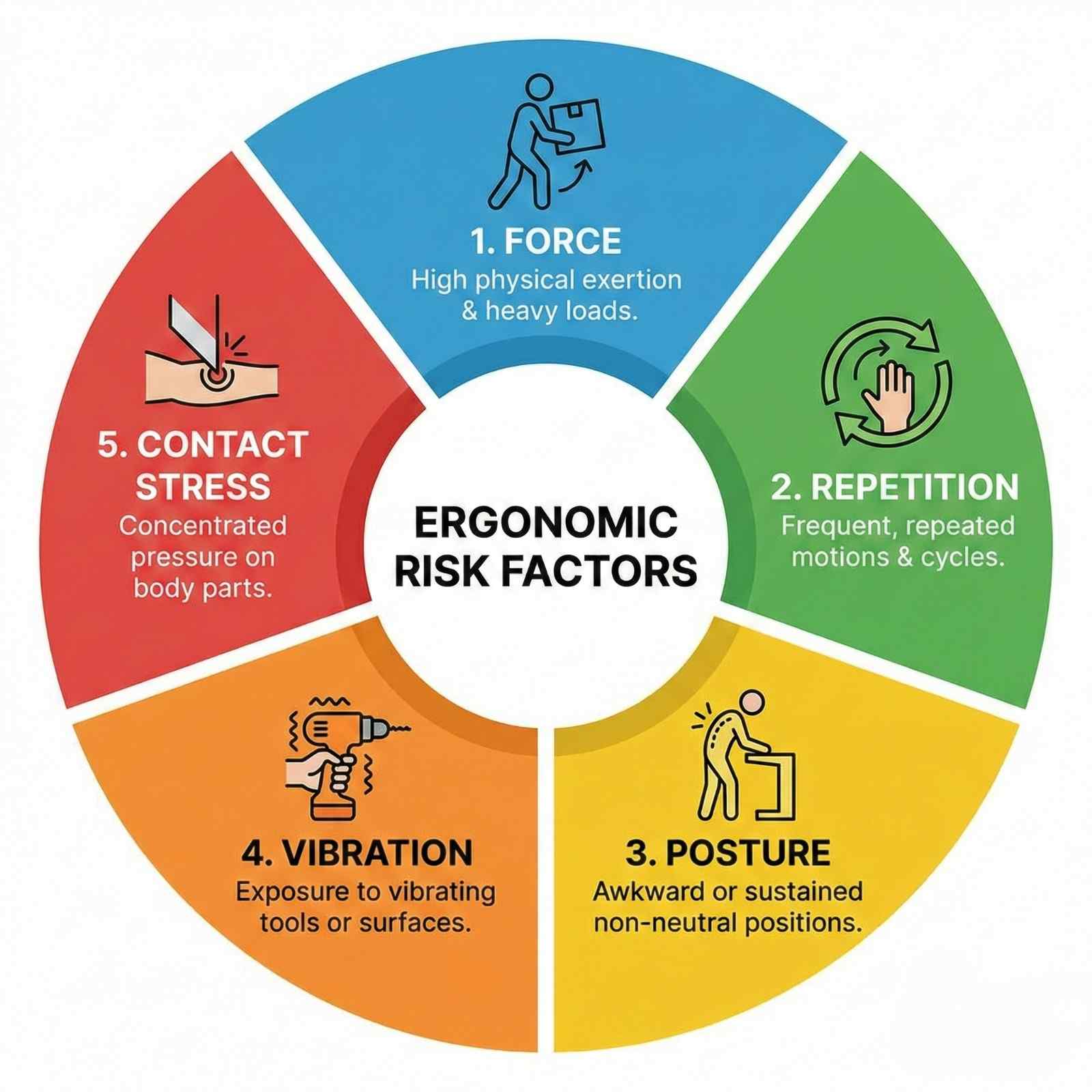
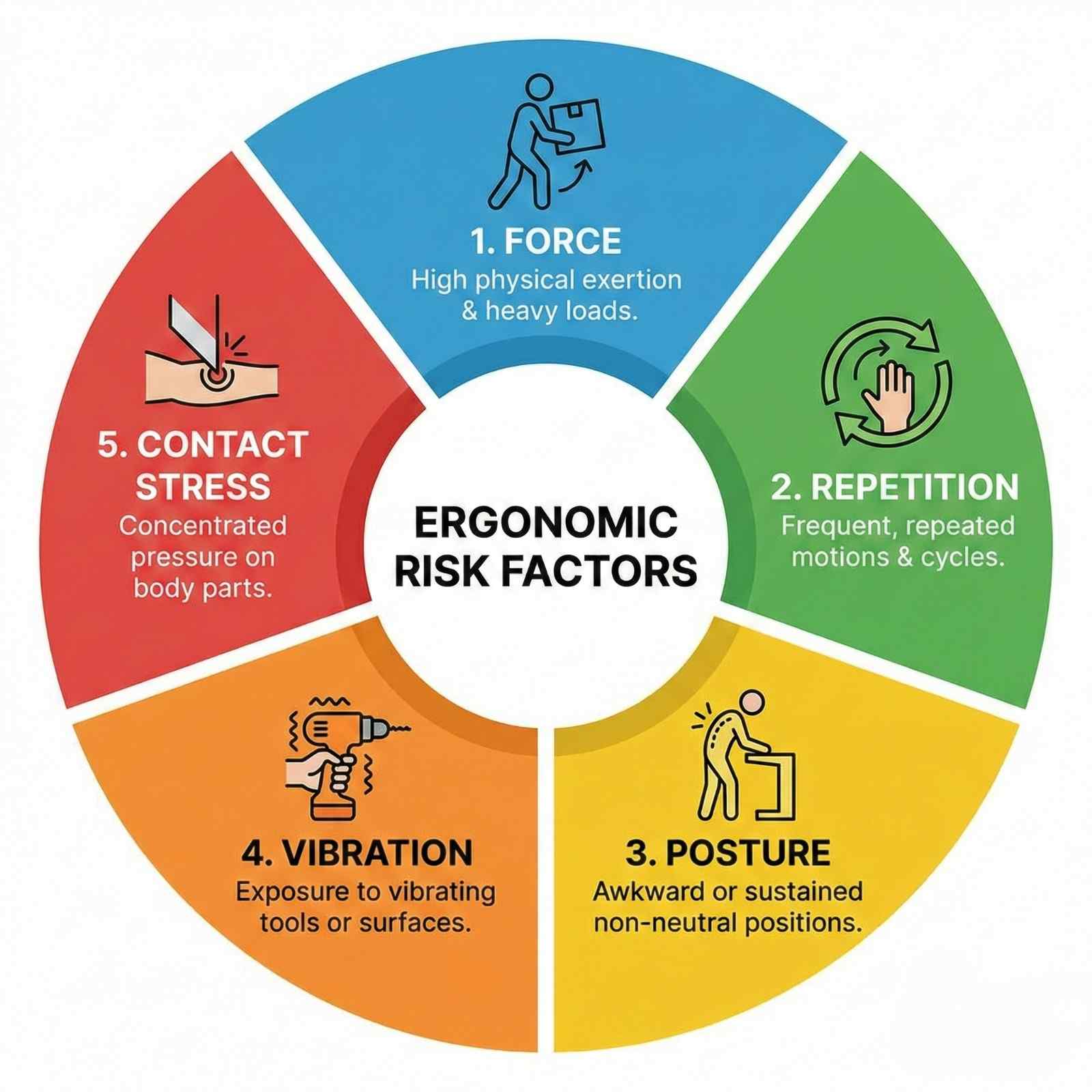
Occupational injury symptoms vary dramatically between acute traumatic injuries and cumulative trauma disorders, requiring different diagnostic approaches and treatment strategies.
Acute workplace injuries present with immediate, easily identified symptoms. Falls from heights produce sudden onset back pain, extremity pain from fractures, or head injury symptoms. Struck-by injuries cause localized pain, swelling, and bruising at impact sites. Lifting injuries typically manifest as acute low back pain with immediate onset during or within hours of lifting incident—"something snapped" or "felt something tear" are common descriptions. Caught-between injuries cause crushing trauma with severe localized pain, swelling, and often open wounds or obvious deformity.
The key diagnostic feature of acute injuries is clear temporal relationship: specific incident, immediate symptom onset, and identifiable injury mechanism. Documentation must capture: exact date and time of injury, detailed mechanism (how did it happen, what position was body in, what forces involved), immediate symptoms reported to supervisor, and any witnesses. Texas workers' compensation law requires injury reporting to employer within 30 days, though earlier reporting strengthens claims.
Cumulative trauma disorders develop insidiously, making recognition more challenging. Early symptoms include vague discomfort, achiness, or stiffness in affected regions during or after work activities. Many workers initially ignore these symptoms, attributing them to normal work fatigue or aging. As exposure continues, symptoms progress through predictable stages:
Stage 1 (Reversible): Aching and tiredness during work shifts, resolving overnight and on weekends. No functional limitations. Symptoms may persist several months. This stage is often dismissed by workers and supervisors but represents critical intervention opportunity—ergonomic modifications and early treatment can prevent progression.
Stage 2 (Reduced Work Capacity): Symptoms persist through nights and weekends. Work performance declines—reduced speed, accuracy, or endurance. Workers may develop compensatory strategies using different muscle groups or modifying techniques to avoid pain, potentially causing secondary injuries. Sleep disruption is common. Medical intervention becomes necessary. With treatment and work modifications, many patients stabilize at this stage, though complete resolution is less likely than Stage 1.
Stage 3 (Chronic/Permanent): Symptoms present at rest and during non-work activities. Unable to perform previously tolerated tasks. Significant functional limitations affecting both occupational and personal activities—difficulty with household chores, hobbies, self-care. Depression and anxiety frequently develop. Outcomes are generally poor; permanent work restrictions or disability often result. Early diagnosis and intervention are crucial to prevent reaching this stage.
Carpal tunnel syndrome (CTS), the most common work-related upper extremity disorder, presents with numbness and tingling in thumb, index, and middle fingers, worse at night. Patients often report waking at night shaking their hands to restore sensation. Daytime symptoms initially occur during provocative activities (gripping, typing, vibration exposure) but progress to constant symptoms. Thenar atrophy (wasting of thumb muscle at base of thumb) and profound weakness indicate severe, long-standing compression requiring urgent surgical decompression. Bilateral CTS suggests systemic factors (diabetes, hypothyroidism, pregnancy) or occupational exposure if symptoms correlate with work patterns.
Lateral epicondylitis (tennis elbow) causes lateral elbow pain radiating into forearm extensors. Pain worsens with gripping, tool use, and wrist extension against resistance. Simple activities like shaking hands, turning doorknobs, or lifting coffee cups become painful. Medial epicondylitis (golfer's elbow) causes medial elbow pain with wrist flexion and forearm pronation activities.
Rotator cuff tendinopathy from repetitive overhead work presents with gradual onset lateral shoulder pain, worse with overhead reaching, lifting, or sleeping on affected side. Morning stiffness improving with activity is characteristic. Progressive weakness indicates advancing from tendinopathy (inflammation) to partial-thickness tear (structural damage) to full-thickness tear (complete rupture).
Low back cumulative trauma manifests as generalized lumbar aching and stiffness after repetitive bending, lifting, or prolonged postures. Symptoms initially occur after work shifts, progressing to occur during work, then persist at rest. Radicular symptoms (leg pain, numbness, weakness) indicate nerve root involvement from disc herniation or spinal stenosis, requiring urgent evaluation. Red flags including bowel/bladder changes, saddle anesthesia, progressive weakness, or fever mandate emergency evaluation for cauda equina syndrome or infection.
De Quervain's tenosynovitis causes radial wrist pain and swelling over the thumb side of wrist, worse with thumb and wrist motion. Finkelstein's test is diagnostic: patient makes fist with thumb tucked inside fingers, then examiner ulnar deviates (bends wrist toward pinky side)—sharp pain over radial wrist confirms diagnosis.
Trigger finger causes catching or locking of affected finger during flexion-extension, often with palpable nodule in palm at base of affected finger. Initially intermittent, catching becomes constant without treatment. Patients may require using opposite hand to straighten locked finger.
Thoracic outlet syndrome from repetitive overhead work or carrying heavy loads causes arm pain, numbness, weakness, and sometimes color changes or swelling. Symptoms vary depending on whether compression affects nerves (numbness, tingling, weakness), arteries (coldness, color changes, diminished pulses), or veins (swelling, discoloration). Diagnosis is challenging, requiring EMG/NCS and sometimes vascular studies.
Chemical exposures common in Pasadena's petrochemical corridor cause additional symptoms. Dermatitis from irritants or allergens causes localized itching, redness, blisters. Respiratory symptoms from inhaled irritants include cough, wheezing, shortness of breath—may represent occupational asthma requiring pulmonary evaluation. Neurological symptoms including headache, dizziness, cognitive impairment, or peripheral neuropathy may result from neurotoxin exposures (solvents, heavy metals, organophosphates).
Documenting symptom progression is crucial for CTD claims. Workers should maintain symptom diaries recording when symptoms occur, what activities provoke them, severity ratings, and functional limitations. Medical providers must document temporal patterns, correlation with work activities, and aggravating/alleviating factors. Progressive worsening despite conservative treatment strengthens claims for advanced interventions or permanent restrictions.
Diagnosing occupational injuries requires clinical examination, strategic imaging, and often electrodiagnostic studies, combined with detailed occupational history establishing work-relatedness.
Occupational history is foundational: job title alone is insufficient—detailed understanding of actual tasks, postures, forces, and exposures is essential. Effective occupational history includes: specific tasks performed (percentage of time in each task), tools and equipment used, weights lifted (typical and maximum, frequency, technique), work postures (sitting, standing, bending, reaching overhead), cycle time (how many repetitions per minute/hour), shift length and break frequency, recent changes in work demands or processes, and use of personal protective equipment.
Job site analysis or ergonomic evaluation provides objective data. Some cases warrant job site visits with measurements of forces, repetition rates, postural demands, and workplace layout. Video recording work activities allows biomechanical analysis. These evaluations are particularly valuable for disputed CTD claims where causation is challenged.
Physical examination for upper extremity cumulative trauma focuses on identifying affected structures and provocative movements. Inspection notes muscle atrophy, swelling, or deformities. Palpation identifies tenderness along specific tendons, muscles, or nerve pathways. Range of motion testing quantifies limitations. Strength testing using manual muscle testing (0-5 scale) or dynamometry quantifies deficits. Provocative tests reproduce symptoms: Phalen's test (wrist flexion for 60 seconds reproduces CTS symptoms), Tinel's sign (tapping over median nerve at wrist produces tingling in median nerve distribution), Finkelstein's test (De Quervain's), resisted wrist extension (lateral epicondylitis), empty can test (rotator cuff).
Electrodiagnostic studies (EMG/NCS) are gold standard for diagnosing nerve compression syndromes and radiculopathies. Nerve conduction studies measure nerve signal transmission: prolonged distal latency, slowed conduction velocity, or reduced amplitude indicate nerve damage. EMG evaluates muscle electrical activity: abnormal spontaneous activity (fibrillations, positive sharp waves) indicates denervation from nerve injury. These studies objectively confirm and quantify nerve damage, critical for medical-legal documentation.
Carpal tunnel syndrome diagnosis requires median nerve conduction delay across wrist: median sensory latency >3.5ms or median motor latency >4.5ms is abnormal. Comparing median to ulnar nerve conduction in same hand improves sensitivity. Electromyography of thenar muscles shows denervation in severe cases. EMG/NCS correlation with clinical findings is essential—abnormal studies without symptoms may reflect subclinical changes or measurement error, while clinical CTS with normal studies (10-15% of cases) should still be treated based on clinical diagnosis.
Cervical or lumbar radiculopathy evaluation includes: MRI identifying nerve root compression from disc herniation, foraminal stenosis, or other pathology; EMG/NCS demonstrating specific nerve root involvement through paraspinal denervation potentials and decreased amplitude in corresponding myotome; and clinical correlation with dermatome (sensory) and myotome (motor) distribution matching imaging and electrodiagnostic findings.
Imaging studies guide diagnosis. X-rays identify bony abnormalities: fractures (acute injuries), degenerative changes (arthritis, bone spurs), and alignment problems. Ultrasound performed by experienced operators diagnoses rotator cuff tears, tendinopathy, and De Quervain's tenosynovitis dynamically and at lower cost than MRI. MRI is gold standard for soft tissue pathology: rotator cuff tears, labral tears, tendon tears, and disc herniations. CT scans excel for bony detail and surgical planning.
Laboratory testing excludes systemic conditions mimicking occupational injuries. Rheumatoid factor and anti-CCP antibodies evaluate rheumatoid arthritis. ESR and CRP assess systemic inflammation. Thyroid function (TSH) evaluates hypothyroidism causing CTS. Vitamin B12, hemoglobin A1c evaluate metabolic causes of peripheral neuropathy. Uric acid assesses gout. These tests are particularly important when bilateral symptoms, systemic symptoms, or atypical presentations suggest non-occupational etiologies.
Causation assessment integrates clinical findings with occupational exposure. Bradford Hill criteria provide framework: strength of association (high exposure correlates with high disease rates), consistency (multiple studies show same association), temporality (exposure precedes disease), dose-response relationship (increased exposure increases risk), biologic plausibility (mechanism makes scientific sense), and coherence (findings consistent across different study types). For individual cases, causation requires: documented workplace exposure to recognized risk factor, injury or condition consistent with that exposure, adequate latency (time between exposure onset and symptom development), temporal relationship (symptoms correlate with work patterns—worse during work, improve on vacation), and exclusion of non-occupational causes.
Work-relatedness documentation must address: specific ergonomic risk factors present in job (NIOSH lifting equation violations, high repetition rates, forceful exertions); comparison of patient's exposures to established occupational exposure limits; medical literature supporting that specific exposures cause diagnosed condition; and analysis of alternative explanations (pre-existing conditions, non-work activities, systemic diseases). This documentation is crucial for workers' compensation acceptance or personal injury claims when compensation is denied.
Functional capacity evaluation (FCE) objectively measures physical abilities: lifting capacity, carrying capacity, postural tolerances, and sustained work capacity. FCE results guide return-to-work decisions, establish permanent restrictions, and provide objective data for disability ratings. Physical and occupational therapists certified in FCE administration provide legally defensible evaluations.
Occupational injury treatment requires addressing both tissue pathology and causative ergonomic factors—treating symptoms without modifying workplace exposures results in symptom recurrence and treatment failure.
Acute traumatic injury management follows standard trauma protocols. Fractures require immobilization, reduction if displaced, and orthopedic referral for surgical fixation when indicated. Sprains and strains receive RICE therapy, NSAIDs, protected weight-bearing or immobilization, and progressive rehabilitation. Lacerations require wound care, tetanus prophylaxis, and sometimes surgical repair. Concussions follow return-to-work protocols similar to return-to-play in sports—cognitive rest followed by gradual return with symptom monitoring.
Cumulative trauma disorder treatment emphasizes early intervention. Stage 1 CTDs respond well to conservative measures: activity modification reducing provocative exposures, ergonomic interventions eliminating biomechanical risk factors, anti-inflammatory treatments including NSAIDs and ice, and splinting for wrist/hand conditions (wrist neutral splints for CTS, counterforce braces for epicondylitis). Many Stage 1 conditions resolve completely with these interventions, allowing continued work without restrictions.
Stage 2 CTDs require more aggressive conservative treatment: physical therapy combining manual therapy, therapeutic exercise, and modality treatments; corticosteroid injections for localized inflammatory conditions (carpal tunnel, trigger finger, epicondylitis, rotator cuff tendinopathy); work restrictions limiting provocative activities; and potential job modification or reassignment if current position cannot be safely performed despite accommodations. Treatment duration extends weeks to months. Response to treatment guides prognosis—persistent symptoms despite 3-6 months aggressive conservative care suggests surgical evaluation.
Stage 3 CTDs often require surgical intervention. Carpal tunnel release (open or endoscopic) decompresses median nerve. Trigger finger release incises constricting A1 pulley. Lateral epicondylitis debridement removes degenerative tendon tissue. Rotator cuff repair addresses tears. Early surgical intervention in Stage 3 improves outcomes compared to prolonged conservative attempts that allow progressive tissue damage.
Physical therapy is cornerstone of CTD treatment. Manual therapy including soft tissue mobilization, myofascial release, and joint mobilization addresses tissue restrictions and improves mechanics. Therapeutic exercise strengthens supporting musculature, improves endurance, and corrects biomechanical deficiencies. Postural training and body mechanics education prevent compensatory patterns. Work conditioning programs progressively increase work-relevant capacity, facilitating return to full duty.
Ergonomic interventions address root causes. Engineering controls modify workplace: adjustable workstations allowing neutral postures, mechanical assists reducing lifting forces (lift tables, hoists, forklifts), tool modifications reducing grip forces or vibration (powered tools replacing manual tools, vibration-dampening gloves), and workstation layout changes reducing reaching distances or awkward postures. Administrative controls modify work organization: job rotation limiting continuous exposure to single task, increased rest breaks allowing tissue recovery, work pace adjustments reducing repetition rates, and two-person lift policies for heavy loads. Personal protective equipment including anti-vibration gloves, wrist supports, and back belts provides last line of defense, though effectiveness varies.
Texas workers' compensation covers reasonable and necessary medical treatment. Injured workers have right to choose initial treating doctor (though insurance carriers may direct care to network providers after initial visit). Medical treatment guidelines in Texas Workers' Compensation Act establish evidence-based treatment protocols—preauthorization may be required for treatments outside guidelines. Disputes about treatment necessity, return-to-work readiness, or permanent impairment ratings can be resolved through insurance carrier appeals, Division of Workers' Compensation benefit review conferences, and contested case hearings.
When workers' compensation claims are denied (common for cumulative trauma where causation is disputed), injured workers may pursue personal injury claims against third parties or direct treatment payment. At AccidentDoc Pasadena, we offer Letter of Protection treatment for workers whose compensation claims are disputed—allowing treatment to proceed while causation litigation is resolved, with payment from settlement proceeds.
Injection therapies provide targeted treatment. Corticosteroid injections reduce inflammation in tendinopathy, bursitis, and nerve compression. Carpal tunnel injections provide temporary relief and help confirm diagnosis—significant improvement post-injection supports CTS diagnosis and predicts surgical success. Trigger finger injections often provide definitive cure, avoiding surgery. Platelet-rich plasma (PRP) injections for tendinopathy show promise in research, though evidence remains mixed and insurance coverage is limited. Prolotherapy (injection of irritant solution stimulating healing response) lacks strong evidence.
Surgical interventions for occupational injuries follow standard indications. Carpal tunnel release is indicated for severe symptoms, thenar atrophy, abnormal EMG/NCS, or symptoms unresponsive to 3-6 months conservative treatment. Endoscopic release allows faster recovery than open technique, though outcomes are equivalent long-term. Trigger finger release is simple outpatient procedure with excellent outcomes. Epicondylitis surgery (debridement of degenerative tendon tissue) is reserved for symptoms persisting >12 months despite conservative treatment. Rotator cuff repair follows guidelines discussed in joint injuries section.
Return-to-work coordination is critical. Modified duty allowing injured worker to remain employed during recovery prevents deconditioning, maintains income, and improves outcomes compared to complete work absence. Gradual return-to-work protocols start with light duty, progressively increasing demands as healing allows. Functional capacity evaluations objectively define safe work capacities, guiding restriction development. Treating physicians provide detailed restrictions: maximum lift weight, frequency of lifting, postural limitations, repetition limits, and duration restrictions. Employers must accommodate restrictions when possible—failure to provide reasonable accommodation may constitute workers' compensation retaliation or ADA violation.
Prevention is paramount. Pre-employment functional testing ensures workers have physical capacity for job demands. Early intervention programs encourage symptom reporting before injuries become severe—many employers have on-site occupational health clinics providing immediate evaluation and treatment. Ergonomic assessments identify hazardous jobs requiring modification. Safety training teaches proper lifting techniques, tool use, and hazard recognition.
Occupational injury recovery timelines vary dramatically between acute trauma and cumulative disorders, influenced by injury severity, age, comorbidities, job demands, and employer accommodation capabilities.
Acute injury recovery generally follows predictable timelines. Simple sprains and strains without complications resolve in 4-8 weeks with appropriate treatment. Moderate injuries requiring extended immobilization or limited surgical intervention need 8-16 weeks. Severe injuries with major surgery or complications may require 6-12 months. Fractures heal according to bone type and location—upper extremity fractures typically allow return to light duty at 6-8 weeks, full duty at 12-16 weeks. Lower extremity fractures affecting weight-bearing require longer disability—tibia fractures may need 12-24 weeks before unrestricted work.
Return-to-work after acute injury follows progressive phases: Phase 1 (weeks 0-2): Complete work restriction while acute symptoms managed, immobilization/protection of injured part. Phase 2 (weeks 2-6): Modified duty begins with significant restrictions—sedentary or light duty only, frequent position changes, no use of injured extremity for primary job functions. Phase 3 (weeks 6-12): Progressive return to full duty with gradually reduced restrictions as healing progresses and functional capacity improves. Phase 4 (week 12+): Unrestricted full duty work when healing complete, strength restored, and functional capacity meets job demands.
Cumulative trauma disorder recovery is less predictable. Stage 1 CTDs caught early may resolve completely in 4-8 weeks with ergonomic modifications and conservative treatment, allowing unrestricted return to work. Stage 2 CTDs typically require 3-6 months treatment, often necessitating permanent work restrictions or job modifications to prevent recurrence—many patients achieve symptom control allowing continued work but not complete cure. Stage 3 chronic CTDs have poor recovery prospects—even with surgery and aggressive rehabilitation, many patients require permanent significant restrictions or work disability.
Return-to-work after CTD treatment must address causative factors. Returning to identical job conditions without modifications guarantees symptom recurrence. Successful return requires: ergonomic modifications eliminating biomechanical risk factors, work restrictions matching functional capacity and preventing symptom exacerbation, graduated return-to-work increasing exposure progressively while monitoring symptom response, and long-term monitoring with periodic reassessment.
Work restrictions for CTDs are highly job-specific. Common restrictions include: lifting limitations (maximum weight, frequency, technique requirements—5-10 lbs occasionally vs frequently, floor-to-waist vs overhead), postural restrictions (minimize repetitive bending, overhead reaching, sustained awkward postures), repetition limits (vary tasks every 20-30 minutes, frequent microbreaks), tool use restrictions (avoid high-vibration tools, forceful gripping), and duration limits (4-6 hour shifts initially progressing to 8-10 hours as tolerated).
Modified duty job descriptions must be detailed and specific, addressing: primary job functions and percentage of time on each task, physical demands (lifting, carrying, pushing, pulling with specific weights and frequencies), environmental conditions, tools and equipment used, and postural requirements. This specificity prevents misunderstandings and allows treating physicians to determine if proposed modified duty is medically appropriate.
Carpal tunnel syndrome recovery post-surgery: weeks 0-2 post-release involve bandage and light activity restriction—typing and light grasping permitted, no heavy lifting. Weeks 2-6: progressive strengthening, return to normal daily activities. Months 2-3: return to full duty work for most jobs. Manual labor positions may require 3-4 months. Symptom improvement is often immediate post-surgery (relief of numbness), but strength and endurance return gradually. 90% of patients achieve good-to-excellent outcomes with carpal tunnel release.
Trigger finger recovery post-release is rapid: 2-3 weeks restricted use, then gradual return to activities. Full recovery typically by 6-8 weeks. Outcomes are excellent with low recurrence rates.
Rotator cuff repair recovery for occupational injuries: protective phase (0-6 weeks) with sling immobilization, passive range of motion only, no return to work. Progressive mobilization phase (6-12 weeks): active motion begins, light duty office work may resume. Strengthening phase (12-20 weeks): progressive resistance training, light-moderate duty work. Return to full duty (20-24 weeks): for non-manual labor. Heavy manual labor requires 6-9 months minimum.
Lumbar injury recovery varies by pathology. Acute lumbar strain without disc herniation or radiculopathy: 2-4 weeks complete or modified duty, then progressive return. Disc herniation with radiculopathy: 6-12 weeks conservative management before considering surgery. Post-discectomy: 4-6 weeks restricted duty, 8-12 weeks return to full duty for sedentary work, 12-24 weeks for heavy manual labor.
Maximum medical improvement (MMI) occurs when condition has stabilized and further improvement is not expected with additional treatment. For acute injuries, MMI typically occurs when healing is complete—3-6 months for most injuries. For CTDs and surgical repairs, MMI may take 12-24 months. Reaching MMI triggers permanent impairment rating.
Permanent impairment ratings quantify lasting functional deficits. Texas workers' compensation uses AMA Guides to the Evaluation of Permanent Impairment, 4th Edition (unlike most states using 6th Edition). Ratings consider: anatomic loss or loss of use, loss of range of motion, pain and sensory deficits, functional loss, and need for ongoing treatment. Upper extremity ratings convert to whole person impairment: shoulder 60%, elbow 70%, wrist 60%, hand 90%, thumb 40%. Impairment ratings determine compensation for permanent partial disability—workers receive weekly benefits for specified number of weeks based on rating.
Disputes about MMI, impairment ratings, or return-to-work capacity frequently occur. Independent medical examinations (IME) by insurance-selected doctors often conclude earlier MMI and lower ratings than treating physicians—creating adversarial situations. Designated doctor examinations by Division-selected neutral physicians resolve disputes, with designated doctor opinions given presumptive weight.
Vocational factors influence outcomes. Younger workers with transferable skills and higher education have better employment outcomes even with permanent restrictions. Older workers in manual labor positions with limited education face poor prospects when permanent significant restrictions prevent return to pre-injury work—vocational rehabilitation, job retraining, or permanent disability may result.
Psychological factors significantly impact recovery. Depression, anxiety, fear-avoidance behaviors, pain catastrophizing, and litigation stress worsen outcomes. Multidisciplinary treatment addressing psychological factors improves functional outcomes beyond physical treatments alone. Cognitive-behavioral therapy, acceptance and commitment therapy, and motivational interviewing show efficacy in chronic pain and work disability.
Secondary gain complicates some cases. Financial incentives (workers' compensation benefits, disability benefits, litigation settlements) may unconsciously influence symptom reporting and treatment response. Symptom magnification or malingering occurs but is far less common than insurance companies suggest. Most injured workers strongly desire return to productivity. Objective testing including FCE, repeat examination for consistency, and correlation of complaints with examination findings help identify exaggeration.
Comprehensive medical-legal documentation is critical for occupational injury claims, as workers' compensation disputes about causation, treatment necessity, work-relatedness, and permanent impairment are common. AccidentDoc Pasadena provides detailed documentation supporting both workers' compensation claims and personal injury litigation when claims are wrongfully denied.
Initial injury report documentation establishes temporal relationship and work-relatedness: "Patient presented [DATE], [X] days after workplace injury occurring [DATE] at [EMPLOYER] where patient works as [JOB TITLE]. Injury occurred when [DETAILED MECHANISM]: patient was [SPECIFIC TASK] when [SPECIFIC EVENT] resulting in [INJURY]. Injury was immediately reported to supervisor [NAME] on [DATE]. Patient has worked at [EMPLOYER] for [X] years in this position without prior injury to this body part. Past medical history per records review shows no prior treatment for [BODY PART] conditions."
For acute injuries, detailed mechanism documentation establishes causation and injury severity: "Patient works as warehouse associate performing order fulfillment. On [DATE] at approximately [TIME], patient was lifting 50-lb box of merchandise from floor to conveyor belt. Box unexpectedly shifted causing sudden twisting motion while in flexed position. Patient immediately experienced severe low back pain with radiation into right leg. Unable to continue work duties. Coworker [NAME] witnessed incident. Injury mechanism—sudden asymmetric loading with flexion and rotation—is biomechanically consistent with lumbar disc herniation."
For cumulative trauma disorders, causation documentation requires detailed exposure analysis: "Patient works as assembly line worker at [EMPLOYER] for 8 years. Job duties require repetitive forceful gripping of pneumatic screwdriver for 85% of 10-hour shifts, performing approximately 400 screw-driving operations per hour (6.7 per minute) with forceful grip requiring estimated 15-20 lbs grip force. Wrist maintained in flexed position 30-40° during tool operation. No microbreaks provided; 30-minute lunch and two 15-minute breaks during 10-hour shift. These exposures exceed ACGIH threshold limit values for hand activity level and constitute high-risk ergonomic factors for carpal tunnel syndrome development. Ergonomic assessment performed [DATE] by certified ergonomist [NAME] documented these exposures (report attached). Patient developed bilateral hand numbness and tingling approximately 2 years ago, progressively worsening over time. Right hand symptoms significantly worse than left, correlating with right-hand dominant tool use. Symptoms worse during work shifts, partially improving on weekends. No non-occupational exposures or systemic conditions (diabetes, hypothyroidism, rheumatoid arthritis) identified. Clinical examination and electrodiagnostic studies confirm bilateral carpal tunnel syndrome, with right greater than left corresponding to exposure pattern."
Examination documentation must quantify objective findings: "Physical examination reveals [SPECIFIC FINDINGS]: tenderness to palpation over [LOCATION], swelling measuring [X cm], ecchymosis [DESCRIPTION], deformity [DESCRIPTION]. Range of motion: [SPECIFIC DEGREES for each plane]. Strength testing: [SPECIFIC MUSCLE GROUPS with 0-5 grade]. Neurological examination: sensation [DERMATOME FINDINGS], reflexes [SPECIFIC REFLEXES with +/++/+++/++++]. Special tests: [TEST NAME] positive, [TEST NAME] negative. Functional limitations observed during examination: unable to [SPECIFIC ACTIVITY], compensatory movements when attempting [ACTIVITY]."
Diagnostic test correlation: "X-rays performed [DATE] demonstrate [SPECIFIC FINDINGS with measurements]. MRI performed [DATE] shows [DETAILED PATHOLOGY with location, size, severity]. EMG/NCS performed [DATE] by Dr. [NAME] reveals [SPECIFIC NERVE CONDUCTION ABNORMALITIES with latencies, velocities, amplitudes]. These objective findings confirm clinical diagnosis of [CONDITION] and establish severity as [MILD/MODERATE/SEVERE]."
Treatment documentation justifies medical necessity: "Treatment plan: (1) Work restrictions—no lifting >10 lbs, limited standing to 2 hours per shift, frequent position changes, no repetitive bending. (2) Physical therapy 3x weekly for 6 weeks focusing on [SPECIFIC INTERVENTIONS]. (3) NSAIDs—ibuprofen 600mg TID for 4 weeks. (4) Follow-up in 2 weeks. If symptoms persist despite conservative management, consider MRI and specialist referral. Treatment goals: reduce pain to allow function, restore strength and range of motion, prevent chronic disability, return to work capacity."
Progress note documentation tracks treatment response: "Patient returns for Week 4 follow-up. Compliance: attended 10/12 PT sessions, taking medications as prescribed, following restrictions (confirmed with employer). Subjective: pain decreased from 8/10 to 5/10, sleeping better. Objective: ROM improved—flexion increased 20°, strength 3/5 to 4-/5. Functional improvements: can now [SPECIFIC ACTIVITY]. Assessment: moderate improvement with conservative treatment. Plan: continue current treatment plan, progress PT intensity, follow-up in 4 weeks."
When treatment plateaus or fails: "Patient has received 6 months conservative management including 24 PT sessions, two corticosteroid injections, trial of multiple NSAIDs, and work restrictions. Despite this aggressive non-operative treatment, patient demonstrates persistent significant symptoms: pain 6/10, functional limitations preventing [JOB DUTIES], objective examination shows [PERSISTENT FINDINGS]. MRI confirms [STRUCTURAL PATHOLOGY]. Conservative treatment has failed to restore function. Surgical consultation with Dr. [ORTHOPEDIST] obtained [DATE]—recommends [SURGICAL PROCEDURE]. Surgery is medically necessary to address structural pathology and restore work capacity."
Causation statements for workers' compensation: "Within a reasonable degree of occupational medicine certainty, this patient's [CONDITION] is causally related to workplace exposures at [EMPLOYER]. Causation is established by: (1) Documented exposure to recognized ergonomic risk factors (detailed in occupational exposure analysis above) exceeding established threshold limits. (2) Temporal relationship—symptom onset correlating with work pattern. (3) Dose-response relationship—symptoms worse during high-exposure periods, partial improvement with reduced exposure (weekends/vacations). (4) Absence of alternative explanations—no systemic diseases, non-occupational exposures, or pre-existing conditions explaining symptoms. (5) Consistency with medical literature establishing [SPECIFIC EXPOSURES] cause [CONDITION]. (6) Objective confirmation on clinical examination and diagnostic testing. This injury arose out of and in the course of employment at [EMPLOYER]."
Work capacity evaluation: "Patient's current work capacity based on functional examination, objective testing, and clinical judgment: Maximum lift 15 lbs occasionally (5% of workday), 10 lbs frequently (33% of workday). No overhead reaching. No sustained awkward postures. No repetitive gripping >2 lbs force. No high-vibration tool use. Can sit continuously 30 minutes, stand 20 minutes, walk 15 minutes before position change required. These restrictions are permanent [or temporary pending further treatment/healing]. Current restrictions prevent performance of pre-injury job duties which require [SPECIFIC DEMANDS]. Modified duty or alternate position necessary."
Permanent impairment rating at MMI: "Patient reached Maximum Medical Improvement on [DATE], [X] months post-injury. Residual impairments include: loss of range of motion ([SPECIFIC MEASUREMENTS]), strength deficit ([SPECIFIC GRADES]), sensory deficits ([DISTRIBUTION]), functional limitations ([SPECIFIC ACTIVITIES]). Using AMA Guides to the Evaluation of Permanent Impairment, 4th Edition, Chapter [X], Table [X]: [CALCULATION METHOD] = [X]% upper extremity impairment which converts to [Y]% whole person impairment using Table [X]. Permanent restrictions: [SPECIFIC RESTRICTIONS]. These impairments directly result from work injury of [DATE] and are permanent."
When claims are denied and personal injury litigation is pursued: "Patient's workers' compensation claim was denied by carrier [CARRIER NAME] on [DATE] based on assertion injury is not work-related [or other stated reason]. I disagree with carrier's determination based on [SPECIFIC MEDICAL EVIDENCE contradicting denial basis]. Alternatively, if injury is determined to have resulted from third-party negligence or employer intentional conduct, patient pursues personal injury claim. My opinions regarding causation, treatment necessity, and permanent impairment are unchanged regardless of whether proceeding under workers' compensation or tort claim."
Seek Emergency Care Immediately If You Experience:
- Progressive hand weakness or rapidly developing thenar atrophy
- Bilateral leg symptoms with saddle anesthesia or bowel/bladder changes
- Progressive foot drop or leg weakness worsening daily
- Severe pain out of proportion to findings - possible CRPS
- Infection signs after injections or surgery - fever, redness, increasing pain
- Compartment syndrome after crush injury - severe pain with passive stretch
- Constant numbness or fixed weakness not improving over 4-8 weeks
- Chemical exposure with respiratory or neurological symptoms
Call 911 or go to the nearest emergency room immediately
Frequently Asked Questions
Common questions about injury treatment at AccidentDoc Pasadena
What types of injuries do you treat at AccidentDoc Pasadena?
We treat all accident-related injuries including whiplash and neck injuries, back pain and spinal injuries, soft tissue damage (sprains, strains, contusions), concussions and traumatic brain injuries, herniated discs, joint injuries (shoulder, knee, wrist), fractures and broken bones, and more. Our board-certified physicians specialize in car accident injuries, truck accident trauma, slip and fall injuries, and work-related injuries.
How soon after an accident should I see a doctor for my injuries?
You should see a doctor within 24-72 hours maximum after any accident. Many serious injuries like whiplash, concussions, and internal injuries don't show symptoms immediately due to adrenaline. Waiting more than 72 hours gives insurance companies ammunition to deny your claim by arguing "if you were really hurt, you would have seen a doctor immediately." Same-day appointments are available at AccidentDoc Pasadena.
Do I need health insurance to get treatment for my injuries?
No. We offer Letter of Protection (LOP) treatment, which means you pay $0 out-of-pocket until your case settles. Your attorney issues a guarantee that medical bills will be paid from your settlement proceeds. This allows you to receive comprehensive medical care immediately without worrying about upfront costs or monthly bills. We also accept PIP (Personal Injury Protection), MedPay, and all major health insurance.
What is the difference between soft tissue injuries and serious injuries?
Soft tissue injuries involve muscles, ligaments, and tendons (like sprains, strains, whiplash, contusions) and typically heal with conservative treatment like physical therapy and pain management within 6-12 weeks. Serious injuries involve bones, joints, nerves, or organs (like fractures, herniated discs, traumatic brain injury, spinal cord damage) and may require surgery, long-term rehabilitation, or result in permanent disabilities. Both types deserve immediate medical attention and proper documentation for insurance claims.
How long does it take to recover from common accident injuries?
Recovery time varies by injury severity: Mild whiplash and soft tissue injuries: 4-8 weeks with proper treatment. Moderate whiplash with disc bulges: 8-16 weeks. Herniated discs: 12-24 weeks, sometimes requiring surgery. Fractures: 6-12 weeks for bone healing plus rehabilitation. Traumatic brain injury: 3-12 months or permanent effects. Our doctors provide personalized treatment plans and realistic recovery timelines based on your specific injuries and response to treatment.
Will treating my injuries affect my personal injury claim?
Yes, in the best way possible. Proper medical treatment strengthens your claim by: Establishing medical causation (proving accident caused injuries), creating detailed documentation insurance companies can't dispute, demonstrating injury severity through objective clinical findings and diagnostic imaging, and supporting higher settlement values with comprehensive treatment records. Conversely, delaying treatment or skipping appointments damages your claim. Insurance adjusters use treatment gaps to argue injuries weren't serious.
Can I choose my own doctor after an accident in Texas?
Yes. Texas law allows you to choose your treating physician after an accident. Insurance companies may suggest you see "their doctor" or an "approved provider"—you are NOT required to follow this recommendation. In fact, insurance company doctors often minimize injuries to reduce claim payouts. Choose a doctor who specializes in accident injuries and works with personal injury attorneys, like AccidentDoc Pasadena.
What should I bring to my first injury evaluation appointment?
Bring: Photo ID, Insurance card (if using insurance), Accident details (date, time, location, how it happened), Police report or accident report number, Photos of accident scene and vehicle damage, Any emergency room discharge papers or previous medical records, List of current symptoms and medications, and Attorney contact information (if you have retained one). Don't have everything? Come anyway—delayed treatment hurts your claim more than missing paperwork.
Specialized Treatment for Your Injury Type
We offer comprehensive care for all types of accident injuries
Car Accidents
Specialized treatment for car accident injuries including whiplash, back pain, and soft tissue damage. Same-day appointments with no upfront costs.
Truck Accidents
Expert care for commercial truck and 18-wheeler accident victims. We understand the severe injuries caused by large vehicle collisions.
Slip & Fall
Comprehensive treatment for slip and fall injuries, including fractures, sprains, head trauma, and soft tissue injuries.
Work Injuries
Specialized workplace injury treatment with documentation for workers' compensation claims. We handle all injury types from lifting injuries to industrial accidents.